1. Red Dots! : Microaneurysms
Seen in Diabetic Retinopathy, retinal vein occlusions, hypertensive retinopathy, radiation retinopathy. Microaneurysms are usually the first ophthalmoscopically detectable sign of diabetic retinopathy. They are focal saccular outpouchings of the capillary wall due to pericyte loss. Arise from the deep part of the inner retinal capillary plexus, and are present in the inner nuclear layer.1
Features:
Appear as small round red dots - usually seen at the posterior pole, especially temporal to the fovea. 10- 100 microns in diameter. Only > 30 microns is visible ophthalmoscopically (better on red-free illumination). < 30 microns can be seen on FFA and hence more microaneurysms are seen on FFA than fundus examination.
Shapes – saccular, fusiform, pedunculated, focal bulge, irregular, mixed.
FFA- Hyperfluorescent with leakage.
OCT – Ring sign, span more than 1 retinal layer.
Course- disappear in 3-6 months. Can continue to exudate, bleed or thrombose.
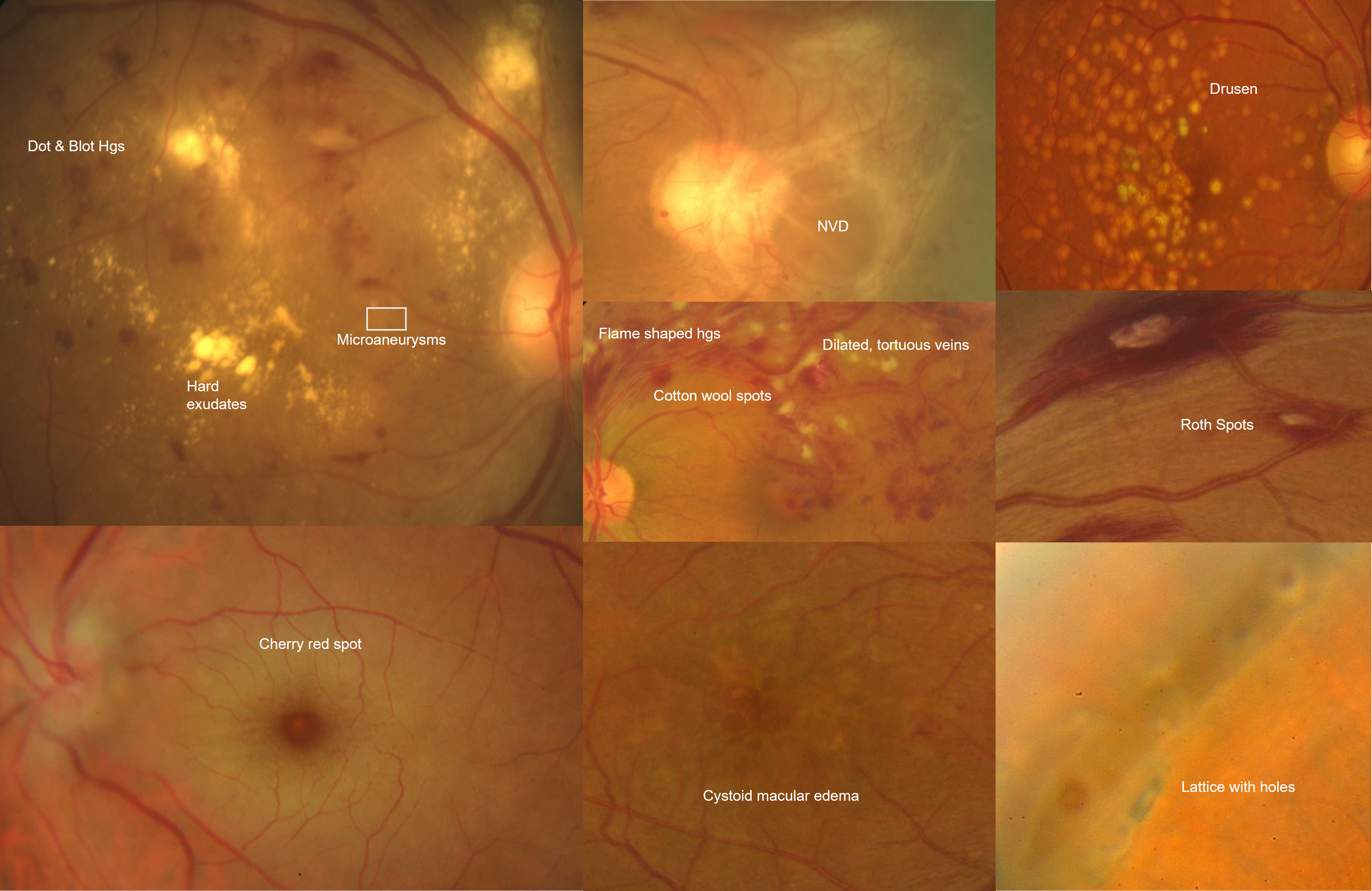
2. And it was all yellow! : Hard Exudates
Seen in - Diabetic retinopathy, Hypertensive retinopathy, BRVO, Radiation retinopathy, Telengiectasias, Neuroretinitis, VHL disease. Associated with high serum lipid levels. They are composed of lipoproteins and lipid-filled macrophages leaking from the impaired blood-retinal barrier. Deposited within the outer plexiform and inner nuclear layers. Occurs due to leakage from microaneurysms and surrounding capillaries. Due to chronic localized retinal edema, develops between the junction of the normal and edematous retina. 2,3
3. Bloody red! : Retinal Hemorrhages
Seen in Diabetic retinopathy, hypertensive retinopathy, Venous occlusions, trauma, blood dyscrasias, etc. Retinal hemorrhages areclassified according to the location in the retina:4,5
|
Types of Hemorrhages |
Description |
Causes |
Three types: |
Superficial and follow the direction, shape, and spread of the RNFL bundles |
|
|
Feathery appearance, superficial, diffuse, found in the posterior pole Resolve around 6 weeks |
Hypertensive retinopathy, retinal vein occlusions, blood dyscrasias, anemias, papilledema |
|
Superficial splinter-shaped hemorrhages. Perpendicular to the disc margin. Start at the optic disc notch. Prelaminar optic disc, cross peripapillary zone, and extend into adjacent RNFL area. |
Normal-tension glaucoma (most common), primary open-angle glaucoma, diabetes, anemia, hypertension, retinal vascular disease etc |
|
Roth spots are round in shape with a white center. Capillary rupture with extravasation, and central fibrin–platelet plug gives the white center to the Roth spot. |
Subacute bacterial endocarditis, leukemia, anemia. |
|
Dense, dark red, sharply outlined. Outer plexiform/ inner nuclear layers. Pre-venular capillaries affected. Takes longer to resolve than flame-shaped hemorrhages |
Diabetic retinopathy, retinal vein occlusions, ocular ischemic syndrome, sickle cell retinopathy, idiopathic juxtafoveal retinal telengiectasias etc. |
|
Between the neurosensory retina and the retinal pigment epithelium (RPE). Deep red in color and broader in shape with diffuse margins. The shape is amorphous due to the absence of firm attachments between the neurosensory retina and RPE. |
CNVM secondary to ARMD, presumed ocular histoplasmosis, high myopia, PCV, retinal macroaneurysm, and trauma |
|
These hemorrhages are located between RPE and Bruch membrane and appear darker red with well-defined sharp borders because of tight junctions of RPE. |
CNVM, choroidal tumors, and choroidal rupture secondary to acute trauma |
|
“Boat” or ‘D’ shaped hemorrhages which collect between the posterior limiting membrane of the vitreous and internal limiting membrane (ILM) of the retina. |
Terson syndrome, Valsalva retinopathy, proliferative diabetic retinopathy, proliferative retinopathy after retinal vein occlusions, trauma |
|
Bleeding into the vitreous cavity. Old vitreous hemorrhage will have an amber-yellow colour. |
Proliferative diabetic retinopathy, retinal vein occlusions, retinal arteriolar microaneurysm, during posterior vitreous detachment, trauma etc. A subretinal hemorrhage can cause a breakthrough bleeding into the vitreous such as in PCV. |
4. Cotton Wool! : Cotton Wool Spots/ Soft Exudates
Occurs secondary to local ischemia from pre-capillary retinal arteriole obstruction → obstruction of axoplasmic flow in the nerve fibre layer → swelling of nerve fibers.6,7
Causes:
- Vascular Diseases: Diabetic Retinopathy, Hypertensive Retinopathy, Vein occlusions, Ocular Ischemic Syndrome, Papilledema, Radiation Retinopathy
- Hematological Disorders: Anemia, Leukemia, Sickle Cells Anemia
- Infectious Diseases: HIV Retinopathy, Neuroretinitis
- Collagen vascular disorders: Giant Cell Arteritis, Behcet’s, SLE
Features: Small, yellow-white/ grayish white elevated fluffy lesions with a feathery border with striations parallel to the nerve fibers in the superficial retina. Obscures the underlying blood vessel. Commonly in the posterior pole. Can resolve in weeks to months leaving a small depression known as ‘Depression Sign’.
FFA: Hypofluorescence due to capillary non-perfusion and the area corresponding to the cotton wool spots as well as blockage by axoplasm stasis. OCT: Hyperreflective lesion in inner retinal layers.
5. Dancing vessels over the retina! : Neovascularisation
NVD- New vessels on or within one disc diameter of the disc; NVE- New vessels elsewhere
Pathophysiology- Increasing hypoxia causes upregulation of angiogenic growth factors like VEGF and PDGF leading to neovascularization. Occurs due to an attempt at vascularizing the ischemic retina. The new vessels lack the integrity and bifurcation of normal vessels and are fragile - bleed spontaneously leading to vitreous hemorrhage.8
Retinal and vitreous hemorrhages attract fibroglial elements → fibrovascular stalks → vitreous contraction → traction on retina → RD
The neovascularization arises from the existing vascular supply of the normal optic disc and nerve fiber layer that includes both a uveal and retinal source.
Causes: Proliferative Diabetic Retinopathy, Retinal vein occlusions, Ocular ischemic syndrome, Sickle cell retinopathy, retinopathy of prematurity, Uveitis, etc.
FFA- leakage and staining in the late phase. OCT – hyperreflective lesion breaking through ILM into the vitreous face.
6. All the vessels! – Retinal Vascular abnormalities
The retinal blood supply –
- Arterial supply - Central retinal artery and choriocapillaris.
- Venous drainage- Central retinal vein.9
The Normal AV ratio is 2:3. Any change in the ratio can assist in diagnosing vascular pathology. Abnormal vascular findings like changes in shape, color, and caliber are generally the biomarkers for major systemic diseases and should be carefully evaluated.
|
Vascular abnormality |
Ocular condition |
Systemic causes |
|
Narrowed retinal arterioles |
Central retinal artery occlusion |
Hypertension, diabetes, atherosclerosis, valvular heart disease, drug abuse, |
|
Dilated retinal arterioles |
Retinal artery macroaneurysm |
Hypertension, atherosclerosis |
|
Tortuous retinal arterioles |
Hypertensive retinopathy |
Hypertension, diabetes |
|
Dilated and tortuous retinal venules |
Central retinal vein occlusion |
Hypertension, diabetes, Hypercoagulable states, Arteriosclerosis, Collagen vascular diseases, hemoglobinopathies |
|
Dilated non-tortuous retinal venules |
Ocular ischaemic syndrome |
Trauma, hypertension, diabetes, Atherosclerosis, Dissecting aneurysm of the carotid artery, Giant cell arteritis |
|
Neovascularisation |
Diabetic retinopathy Retinal Vein occlusion Retinal artery occlusion Chronic retinal detachment |
Hypertension, diabetes, atherosclerosis, Hypercoagulable states |
|
Collaterals |
Retinal vein occlusion |
Hypertension, diabetes, atherosclerosis, Hypercoagulable states |
|
Telangiectatic vessels |
Coats disease MacTel |
Idiopathic Diabetes, hypertension |
7. Red in the middle of white! : Cherry Red Spot
Appearance of a red-tinted region at the center of the macula surrounded by retinal opacification.10
Causes: CRAO, Tay Sachs disease, Niemann picks disease, Gaucher's disease, Commotio retinae, drug toxicity like quinine, dapsone, etc. In CRAO, the vascular supply of the choroid is unaffected. Inner retinal layers are absent in mature foveola. Thus, the foveola, the thinnest part of the central retina, does not lose its transparency during inner retinal ischemia. In lipid storage disorders, there is an accumulation of material in the ganglion cells of the retina The foveola is devoid of the ganglion cell layer and hence remains transparent and allows transmission of the color of the choroid and the RPE.
Features: Reddish area in the center of macula surrounded by retinal whitening. Its appearance is because of the relative transparency of the macula. Seen bilaterally in metabolic disorders, quinine, and other drug toxicity and Leber's congenital amaurosis; whereas, it is seen unilaterally in most cases of CRAO, orbital contusions. Ruling out serious life-threatening or sight-threatening diseases is of paramount importance in a patient with a cherry-red spot at the macula. The management varies according to the cause.
Useful Mnemonic: Cherry Trees Never Grow Tall- CRAO, Tay Sachs, Niemann Pick, Gauchers, Trauma
8. Cysts at the macula! : Macular Edema
Accumulation of fluid in the center of the macula secondary to causes such as diabetic retinopathy, retinal vein occlusions, post-cataract surgery (Irvine-Gass Syndrome), uveitis, age-related macular degeneration, retinitis pigmentosa, retinoschisis, drug-related.11
Cystoid macular edema(CME) involves fluid accumulation in the outer plexiform layer secondary to leakage from perifoveal retinal capillaries.
Remember "DEPRIVEN" (diabetes, epinepherine, pars planitis, retinitis pigmentosa, Irvine-Gass syndrome, venous occlusion, E2-prostaglandin analogs, nicotinic acid/niacin).
Features: 78 D or 90 D examination is better to identify CME. There will be loss of foveal reflex and the presence of multiple cyst-like fluids in the macula with retinal thickening. Cysts can be present in honeycomb patterns: Appearance is Due to the radial arrangement of Henle's layer fibers. FFA: Classic petaloid leakage seen in CME. OCT: Intraretinal cystic areas with retinal thickening.
9. Sand Dunes! – Drusen
They are accumulations of extracellular material immediately beneath the retinal pigment epithelium (RPE) and Bruch’s membrane. 12
Causes: Normal aging (>50 years of age), Age-related macular degeneration (>50 years of age), Inherited retinal disorders (early-onset <50 years of age), Systemic disorders- MPGN, Alport's syndrome, Vitamin A deficiency, Pseudoxanthoma elasticum
Features: Yellowish white deposits under RPE in posterior pole and periphery and sometimes on the disc.
Types
- Smalldrusen(“drupelets”) are less than 63 µm in diameter,
- Intermediatedrusenare 63 to 125 µm, and
- Large drusen are greater than 125 µm.
Hard drusen -Bright yellow, well-defined margins <63 microns, asymptomatic mostly
Soft drusen- pale yellow, ill-defined, >63 microns, high risk of Neovascular AMD.
Has 3 subtypes -It can be membranous (63-175 microns), granular (250 microns), and serous (500 microns)
Subretinal drusenoid deposits (also known as reticular pseudodrusen) are located above the RPE and are associated with progression to advanced AMD.
Early-onset drusen- Types – Cuticular drusen, Large colloidal drusen, Autosomal dominant radial drusen
FFA – Small drusen – hyperfluorescence in the early phase. Large drusen- late pooling or staining. OCT - is valuable in the differential diagnosis of drusen. Appear as nodular elevations under RPE and sometimes as retinal pigment epithelial detachments.
10. Criss-Crossing!: Lattice Degeneration
Peripheral retinal degeneration with spindle-shaped areas of retinal thinning, the most common degeneration to cause retinal detachment. 8-10% incidence. Present in 20-30% of Rhegmatogenous retinal detachment (RD). Symmetrical and bilateral, most common supero-temporarily.13,14
Discontinuity of internal limiting membrane. Overlying area of liquified vitreous. Condensation and exaggerated adherence of vitreous gel at the margin of the lesion. Atrophy of inner retina.
Features: Elongated lesions with a long axis parallel to the ora serrata, located in the peripheral retina, usually hyperpigmented and mottled looking. Scleral depression may be required to identify the lesions. Lesions that are located at or posterior to the equator tend to be larger. The base of the lesion has a moth-eaten uneven appearance, and the overlying thin degenerating retina is often jagged. Sclerosed white vessels display a crisscrossing pattern - the appearance responsible for the term ‘lattice’.
Abnormal pigmentation - the most common finding - increases with age. Tiny white or yellow flecks can be present between the retinal surface and the vitreous cortex.
Indications for treatment with barrage laser: Symptomatic patients, positive family history of retinal detachment, retinal detachment in the fellow eye, trauma-related retinal breaks.
References:
- Henry E. Wiley, Frederick L. Ferris, Chapter 47 - Nonproliferative Diabetic Retinopathy and Diabetic Macular Edema, Retina (Fifth Edition), W.B. Saunders, 2013
- Davoudi S, Papavasileiou E, Roohipoor R, Cho H, Kudrimoti S, Hancock H, Hoadley S, Andreoli C, Husain D, James M, Penman A, Chen CJ, Sobrin L. OPTICAL COHERENCE TOMOGRAPHY CHARACTERISTICS OF MACULAR EDEMA AND HARD EXUDATES AND THEIR ASSOCIATION WITH LIPID SERUM LEVELS IN TYPE 2 DIABETES. Retina. 2016 Sep;36(9):1622-9.
- Otani T, Kishi S. Tomographic findings of foveal hard exudates in diabetic macular edema.American journal of ophthalmology.2001;131:50–54.
- Kanukollu VM, Ahmad SS. Retinal Hemorrhage. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
- Shechtman, D., Kabat, A. “The Many Faces of a Retinal Hemorrhage.” Optometric Management.
- Purnima S. Patel, SriniVas R. Sadda. "Retinal Artery Obstructions." In Retina (Fifth Edition), by Stephen J. Ryan, 1012-1025. Elsevier Inc., 2012
- Adam T. Gerstenblith, Michael P. Rabinowitz. Wills Eye Manual, The: office and emergency room diagnosis and treatment of eye disease, 6th edition. Lippincott Williams & Wilkins, 2012.
- Henkind P. Retinal blood vessels. Neovascularization, collaterals, and shunts. Aust J Ophthalmol. 1981 Nov;9(4):273-7.
- Leticia Rousso, Joseph Sowka, Recognizing Abnormal Vasculature, Review of Optometry, Jan 2017
- Tripathy K, Patel BC. Cherry Red Spot. 2021 Feb 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
- Gass JD, Norton EW. Follow-up study of cystoid macular edema following cataract extraction.Trans Am Acad Ophthalmol Otolaryngol. 1969;73:665-682.
- Susan B. Bressler, Neil M. Bressler, Chapter 65 - Age-Related Macular Degeneration: Non-neovascular Early AMD, Intermediate AMD, and Geographic Atrophy, Retina (Fifth Edition),W.B. Saunders, 2013
- Byer NE, Lattice degeneration of the retina. Surv Ophthalmol. 1979 Jan-Feb; 23(4):213-48.
- Wilkinson CP. Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment.Cochrane Database Syst Rev.2014;9:CD003170.

