Chief Complaint:
A 37 years old male presented to us with a history of progressive deterioration of vision on 30/09/2020.
History of Present Illness:
He was diagnosed elsewhere to have glaucoma and came to us for further management.
Past Ocular History:
He was already on on Latanoprost ED HS, Dorzolamide + Timolol combination BD.
The patient underwent Trabeculectomy in both eyes in the year 2010 and 2013
Baseline IOP from old records was noted to be 18 mm of Hg in the right eye and 17 mm of Hg in the left eye
Family History:
Strong family history of glaucoma in father and elder sister
Review of Systems/Systemic Examination
Not a known case of hypertension, diabetes, asthma or cardiological problem, not on any systemic medication.
OCULAR EXAMINATION
Best Corrected Visual Acuity (Snellen)
- Right eye (OD): 6/6,N6
- Left eye (OS): 6/9,N6
Ocular Motility/Alignment- EOM full and free
Intraocular Pressure (IOP)
- OD: 11 mm of Hg
- OS: 10 mm of Hg
Pupils: OD – round , regular and reacting to light
OS- Sluggishly reacting with grade 2 RAPD
Slit-lamp exam:
|
RE (OD) |
LE (OS) |
|
|
BCVA |
6/6 for distance, N6 for near |
6/9 for distance, N6 for near |
|
Colour vision |
21/21 (with Ishihara chart) |
21/21 (with Ishihara chart) |
|
Bleb |
Flat bleb, surgical PI patent |
Flat bleb, surgical PI patent |
|
Cornea |
clear |
clear |
|
CCT |
522 microns |
516 microns |
|
AC |
Normal depth, VH III-IV, quiet All quadrants open till Scleral spur(SS) on gonioscopy |
Normal depth, VH III-IV, quiet All quadrants open till Scleral spur(SS) on gonioscopy |
|
Pupil |
RRR, Brisk |
Sluggish, RAPD+ (Grade II) |
|
Lens |
Clear |
Clear |
Dilated Fundus examination
- Vitreous: normal both eyes
- Disc: Right eye- Average sized disc, VCDR 0.8:1, IR notch, SR thin
Left eye - Average sized disc, VCDR 0.9:1, IR loss, SR thin
- Macula: FR+ both eyes
- Vessels: normal calibre maintaining normal A:V ratio
- Periphery: Retina on with normal peripheral fundus in both eyes
Ancillary Investigations:
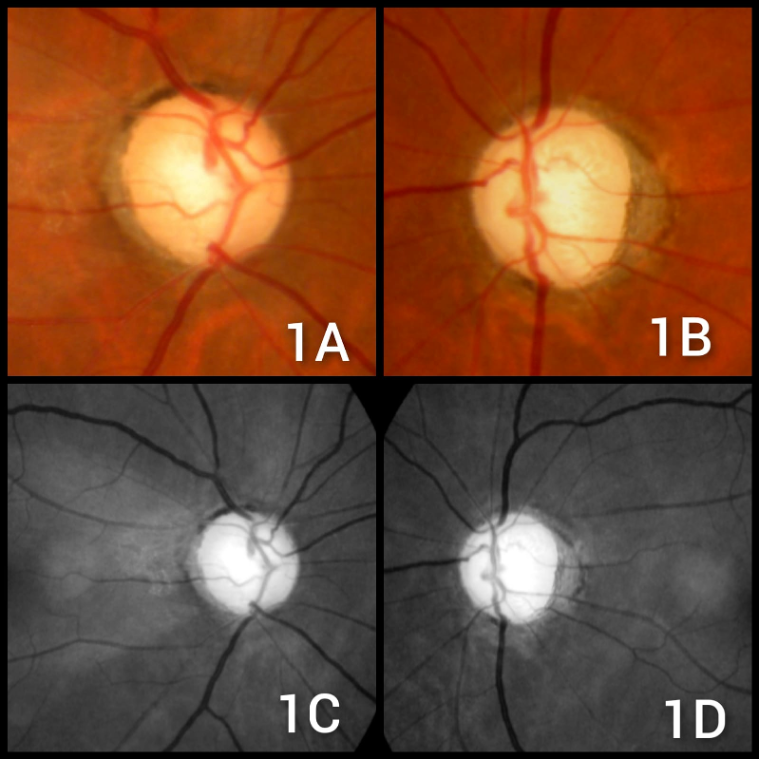
20-degree color disc photo and 30-degree red-free images(FIG 1 ) show both eyes glaucomatous damage as noted along with the wedge-shaped nerve fiber layer defect, more prominent in the red free ones.
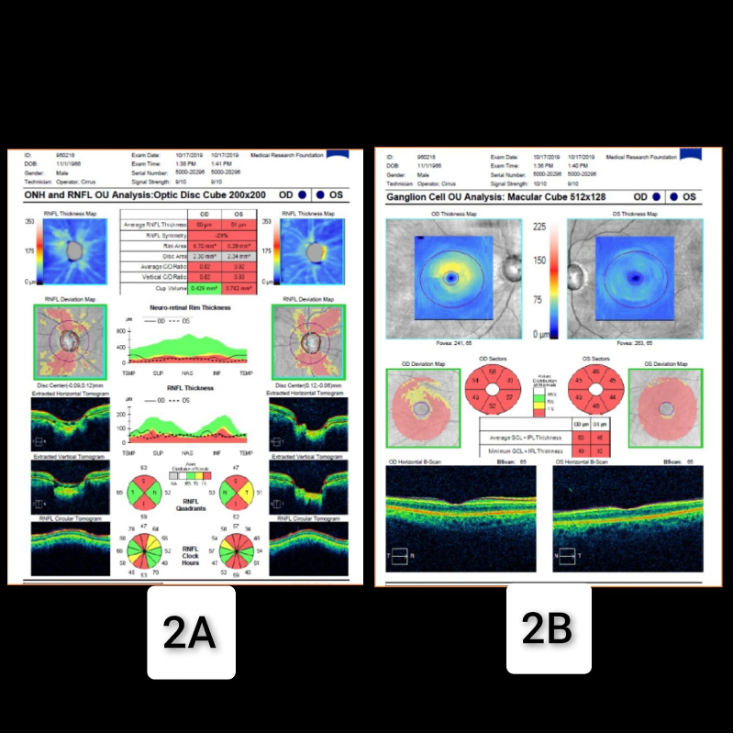
OPTICAL COHERENCE TOMOGRAPHY (FIG 2) Both eyes superior and inferior nerve fibre layer thinning corresponds to the disc images. The ganglion cell complex shows thinning too.
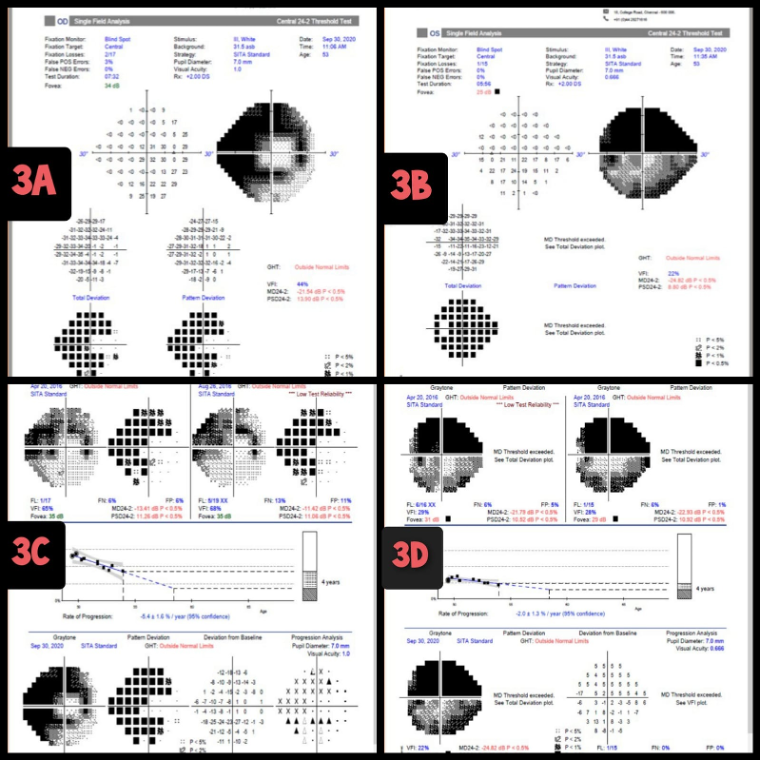
GLAUCOMA PROGRESSION ANALYSIS(GPA) ON HUMPHREY VISUAL FIELDS (HVF) (FIG 3)- both eyes HVF showing damage corresponding to the disc. other eyes GPA analysis on HVF shows how glaucoma is progressing over the years
Clinical Course of the condition:
A 52-year-old male presented with gradually progressive diminution of vision for the last 1 year due to progressive glaucoma. The IOP was never above 21 mm of Hg but the glaucoma was progressing even on multiple anti-glaucoma medications. The patient underwent office hours Diurnal variation test (DVT) which did not reveal any spike in intraocular pressure (IOP). The patient underwent trabeculectomy with MMC in both eyes elsewhere but the progression of glaucoma never deterred. The patient was also investigated for 24 hours ambulatory BP monitoring, Carotid Doppler, ischaemic workup, and sleep study to rule out Obstructive sleep apnoea syndrome. Although the other investigations turned out negative, the Sleep study revealed mild obstructive sleep apnoea syndrome. The patient was started on treatment for OSAS along with continuation for Antiglaucoma medications
Differential Diagnosis:
- Primary open-angle glaucoma
- Steroid-induced glaucoma
- Pseudo-exfoliation glaucoma
- Uveitic glaucoma
Diagnosis:
A case of normal-tension glaucoma associated with Obstructive sleep apnoea
DISCUSSION
EtiologyNormal-tension glaucoma is a form of Open-angle glaucoma characterized by glaucomatous optic atrophy associated with Intraocular pressure consistently below 21 mm of Hg in all visits.
The etiology of normal tension glaucoma is still unclear. It has been theorized that the disease process in NTG results from an enhanced sensitivity to what would otherwise be physiologic IOP, resulting in glaucomatous damage of the optic nerve. This enhanced sensitivity may be due to impaired optic nerve blood flow or a structurally abnormal lamina cribrosa, which cannot withstand a normal range of IOP.
EpidemiologyPopulation-based studies have found that anywhere from 10% to 48% of all open-angle glaucoma patients in the United States, Europe, and Scandinavia have NTG, and up to 66% of the Japanese population have NTG. This form of glaucoma is more common in the elderly. The mean age group in various clinical studies are 60 years
PathophysiologyThe mechanism for the development of glaucomatous optic neuropathy is unknown. How the optic nerve damage happens in the setting of normal IOP that still remains a matter of debate.Current research is in part directed towards the physiologic forces that affect perfusion of the optic nerve vasculature as well as cellular oxidative changes that occur with changes in perfusion.
The relationship between systemic hypertension and hypotension, ocular vascular perfusion pressure, and local regulation of ocular blood flow by vascular tone mediators such as endothelin seem to play a role in the maintenance of constant perfusion of optic nerve tissues.In addition, mechanical factors are being investigated as to their role in the pathogenesis of optic neuropathy. Focal and/or diffuse compromise in the structural integrity of the lamina cribrosa has also been suggested in the pathogenesis of the disease. Recent research has also found an increased prevalence of OSAS among the NTG group of patients.
OSAS is characterized by recurrent interruption of normal breathing during sleep, owing to upper airway obstruction (apnoeic spells) The apnoeic spells can cause a decrease in arterial oxygen saturation and a rise in carbon dioxide saturation during sleep. OSAS also compromises circulation at the optic nerve head by causing hypoxia and vascular dysregulation in patients with NTG. The prevalence overall for OSAS among NTG is 5.7% and in cases of severe OSAS 7.1%.
Clinical Features
Diagnosing NTG is a diagnosis of exclusion.
The main clinical features present in a case of normal tension glaucoma are-
- A mean IOP off treatment consistently equal to or less than 21 mm Hg on diurnal testing, with no single measurement greater than 24 mm Hg
- Open drainage angles up to scleral spur on an undilated darkroom gonioscopy
- Absence of any secondary cause for a glaucomatous optic neuropathy—for example, a previously raised IOP following trauma, a period of steroid administration, or an episode of uveitis
- Typical optic disc damage with glaucomatous cupping and loss of neuroretinal rim (NRR)
- Visual field defect compatible with the glaucomatous cupping (disc/field correlation)
- NTG is generally a progressive disorder and without intervention can proceed rapidly.
Few researchers have noted to find advanced Neuroretinal rim loss along with peri-papillary atrophy in cases of normal tension glaucoma
Significance of Disc Haemorrhages in Patients With NTG
Several studies have found a link between the presence of disc hemorrhages and NTG. The presence of a disc or Drance hemorrhage can be a worrisome sign that the patient’s glaucoma is poorly controlled and that the patient will likely experience progression of loss in visual fields over the next few months. Assessing for the presence of a disc hemorrhage should be part of the routine ophthalmologic examination, and when a hemorrhage is found, optic nerve head photography should be performed for documentation.
Visuals defects in NTG
Visual field defects typically appear deeper, steeper, and closer to fixation in patients with NTG than in patients with POAG. NTG tended to be more localized than that in Open-angle glaucoma. Several groups have shown that the superior hemifield is most frequently affected in NTG.
Ancillary Investigation
The following investigations hold an important role in the diagnosis of NTG
Goldmann Applanation TonometryThe IOP should never go above 21 mm of Hg for the diagnosis of NTG. GAT has to be monitored at different times of the day.
Diurnal variation test (DVT) or Phasing24 hours IOP monitoring helps to determine the Intraocular pressure spikes and is used as an important diagnostic tool. In case of inability to perform 24 hrs IOP monitoring, one can resort to office hours of IOP monitoring- although the chance of missing the morning spikes are higher.
PachymetryAssessment of central corneal thickness (CCT) through pachymetry is essential in the workup of normal tension glaucoma. The measured IOP by applanation may be artifactually low in eyes with low CCT. Many patients with a diagnosis of NTG will demonstrate a low CCT. In some cases, correction of this under measurement (based on published correction factors) may reveal an actual IOP more consistent with POAG
Visual FieldsAutomated static perimetry is the most common modality used to detect and monitor for progression of the field loss associated with normal tension glaucoma. Visual field defects may include those common to POAG including nasal step and arcuate scotoma. However, defects noted in NTG tend to be more focal and occur closer to fixation early in the disease. Dense paracentral scotomas may characteristically be noted at the initial diagnosis.
Optic disc imagingOptic disc imaging is an important and objective structural assessment of optic nerve health. For several decades, the gold standard for detecting disease and monitoring changes in the optic nerve head has been stereo disc photography (20-degree color and 30-degree red-free).
Glaucoma Imaging- Various imaging technologies likeOptical coherence tomography (OCT)and confocal scanning laser ophthalmoscope (Heidelberg retina tomograph [HRT]) are also being used to document and monitor changes due to glaucomatous damage in the optic disc and the retinal nerve fibre layer
Gonioscopy- regular darkroom gonioscopy to document the open angles in all visits are animportant cornerstone for the diagnosis of NTG
Other Laboratory Investigation-
Other investigations include 24-hour blood pressure monitoring to exclude nocturnal systemic hypotension; blood tests to rule out other causes of glaucomatous optic neuropathy such as vitamin B12 and folate levels, ESR/CRP, and serum ACE. Cranial MRI may be necessary to rule out intracranial space-occupying lesions (SOLs), and nail fold capillaroscopy with cold provocation may detect blood flow abnormalities. Polysomnography can also be done to check for OSAS.
Treatment The main goal of glaucoma treatment is IOP reduction. The two most important study have given insight into the management of NTG.
The Early Manifest Glaucoma Trial(EMGT) showed that glaucoma progression was decreased by 10% with a reduction of each mm Hg of IOP.
According to the Collaborative Normal-Tension Glaucoma Study(CNTGS) Group, an IOP reduction of 30% slowed the progression of normal-tension glaucoma. Criteria for initiation of treatment of the NTG patients in this study were defined as: documented visual field or optic nerve progression, visual field loss threatening fixation, or presence of disc hemorrhage. The treatment group had a 12% risk of progression at 5 years compared to 35% progressing in the non-treatment group.
Medical therapy
Topical IOP lowering medications including prostaglandin analogs, alpha-2 agonists, beta-blockers, and carbonic anhydrase inhibitors are the mainstays of medical therapy. Medications should be chosen on an individual basis to provide treatment that achieves a sufficient IOP reduction with minimal side effects and ease of administration. Medication choice should also be cost-effective for the patient based on their resources. For a full discussion of medical management please see the POAG main article.
Surgical Therapy
Laser and surgical treatment options for NTG is the same as those for POAG.
Selective Laser trabeculoplasty (SLT) may be a useful moderately invasive treatment with or without medical therapy. Indeed, there is some literature that supports an IOP lowering and decreased IOP variability, the effect of SLT in NTG patients.
For patients with IOP targets that are not achievable with medical/laser therapy, filtration surgery with or without a drainage device is the mainstay of surgically lowering IOP.
In CNTGS, the IOP reduction of 30% was only achieved in 57% of patients by topical medication and/or laser trabeculoplasty, while the remaining 43% required filtering surgery.
While IOP lowering with filtration surgery has been shown to be effective in decreasing visual field progression a continued, slowed progression has been reported in postoperative patients followed for up to 6 years
The newer Minimally Invasive Glaucoma Surgery(MIGS) holds an interesting prospect in the treatment of normal tension glaucoma (NTG).
NORMAL TENSION GLAUCOMA |
|
|
Etiology
|
Signs
|
|
Symptoms
|
Differentials
|
|
Investigations
|
Treatment
|
