Choroidal neovascular membrane (CNVM) is an ingrowth of new vessels from the choriocapillaris through a break in the outer aspect of Bruch’s membrane into the sub-pigment epithelial space.
These new vessels are accompanied by fibroblasts, resulting in a fibrovascular complex that proliferates within the inner aspect of Bruch’s membrane. This fibrovascular complex can disrupt and destroy the normal architecture of the choriocapillaris, Bruch’s membrane, and the RPE. In addition, fibroglial and fibrovascular tissue can also disrupt and destroy the normal architecture of the photoreceptors and the remaining outer retina leading to the formation of a disciform scar.
Within the subpigment epithelial space, the CNV can leak fluid and blood and may be accompanied by a serous or hemorrhagic detachment of the RPE.
CNVM that remains restricted to the sub-RPE space is Type1 CNVM and when it becomes sub-retinal it is Type 2 CNVM.
Clinical Features
Symptoms of CNVM:
-
Sudden onset of decreased vision
-
Metamorphopsia
-
Central scotoma
Signs of CNVM:
-
Presence of subretinal fluid
-
Subretinal or sub-RPE bleed
-
Subretinal or intraretinal lipid
-
Subretinal pigment ring
-
Irregular elevation of RPE
-
Subretinal grey-white lesion
-
Cystoid macular edema
-
Subretinal small vessels
Diagnosis of CNVM:
Fundus fluorescein angiography(FFA) is the gold standard for diagnosis of CNVM. When there is overlying blood or occult CNVM, Indocyanine green angiography(ICGA) helps in decision making.
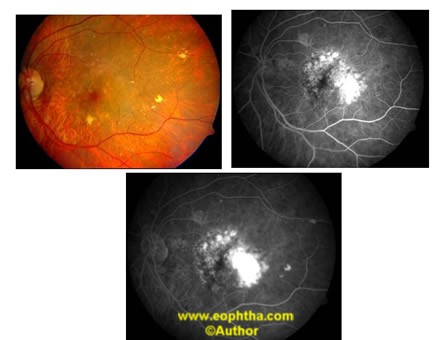
FFA patterns of CNVM: Two main patterns are seen---Classic and occult. Additionally there may be combinations of the two also.
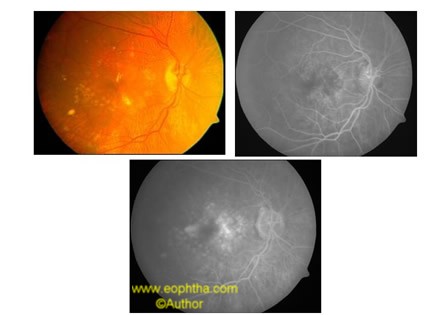
Classic CNVMis seen as an area of bright, hyperfluorescence seen in the early phase of the angiogram which intensifies throughout the transit phase and leaks in the late phase showing fuzziness of borders in late phase. The early hyperfluorescence is often seen as a lacy pattern with well defined borders. Depending on its location with respect to the fovea, classic CNVM may be:
-
Extrafovealwhen the CNVM is more than 200microns from the centre of the foveal avascular zone(FAZ).
-
Subfovealwhen the centre of the FAZ is involved either by extension from an extrafoveal area or by originating directly under the centre of the fovea.
-
Juxtafovealwhen the CNVM is closer than 200microns from the centre of the FAZ but does not involve it.
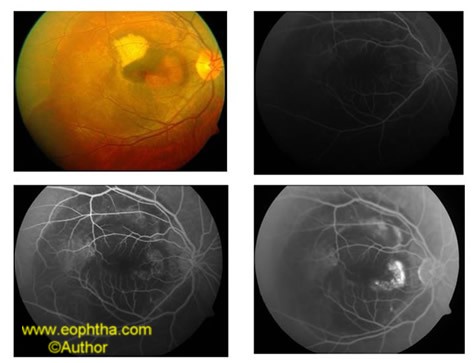
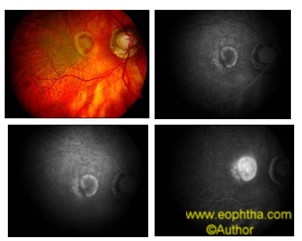
Fig 1: Large Classic CNVM
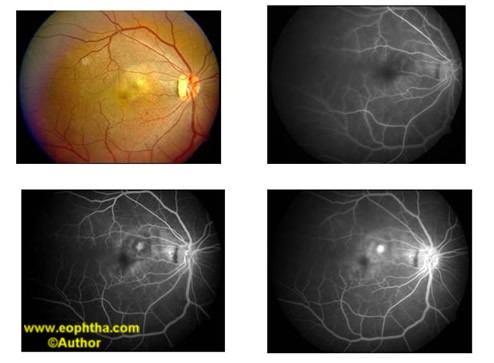
Fig 2: Extrafoveal Classic CNVM
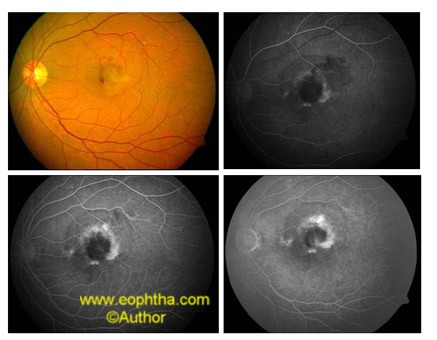
Fig 3: Subfoveal CNVM
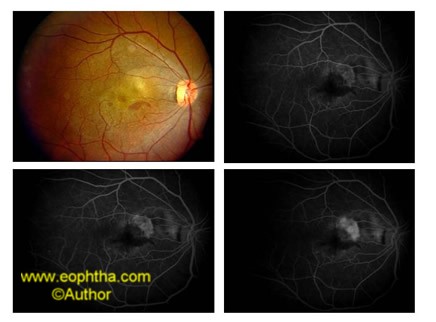
Fig4: Juxtafoveal Classic CNVM
Occult CNVMis a poorly defined membrane. It may present in two forms:
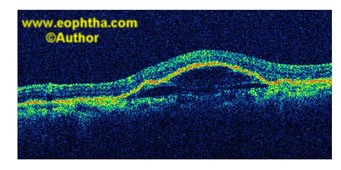
Fibrovascular pigment epithelial detachment (PED)which is an irregular elevation of RPE with stippled or granular irregular fluorescence seen in early phase usually by 1-2 minutes after dye injection. There is progressive leakage from these regions with a stippled hyperfluorescent pattern that is not as diffuse as seen in classic CNVM.
Fig 5: Fibrovascular PED
Fig 6: OCT image of Fibrovascular PED
Late leakage of an undetermined sourcewhen regions of hyperfluorescence are seen at the level of RPE which are best appreciated in the late phase of the angiogram.
Fig 7: Diffuse Hyperflourescence of undetermined source
When looking at the size of a CNVM, all areas of classic and occult CNVM as well as areas with obscured features such as blood in contiguity with the CNVM, pigment, scar tissue as well as serous PED ,must be taken into account.
The terms predominantly classic, minimally classic, and occult with no classic are used to determine who will benefit from photodynamic therapy.Predominantly classic lesionsare those where the CNVM occupies more than 50% of the lesion,(including contiguous blood, pigment, scar and staining) and the proportion of classic CNVM also occupies more than 50% of the entire lesion.Minimally classic CNVMis one where the proportion of classic CNVM occupies between 1% and 49% of the entire lesion.Occult with no classic CNVMis when there is no classic CNVM in the lesion and the whole lesion is only occult CNVM.
Causes of CNVM:
-
Neovascular age related macular degeneration
-
Ocular Histoplasmosis Syndrome
-
Angioid Streaks
-
Pathologic Myopia
-
Idiopathic CNVM
-
Choroidal rupture from trauma
-
Intense photocoagulation(iatrogenic)
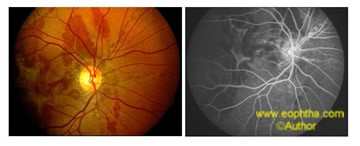
Fig 8: Angioid streak with CNVM
Fig 9: Myopia with CNVM
Fig 10: Choroidal rupture
Differential Diagnosis:
Retinal Arterial Macroaneurysm: The clinical picture may resemble haemorrhage from a CNVM. Fundus fluorescein angiography and ICG angiography will demonstrate the dilated lumen of the microaneurysms along the arteriole.
Adult vitelliform dystrophy: The lesion may look like a retinal PED or an area of large confluent drusen. On FFA early hypofluorescence (blocked) and late staining of the vitelliform lesion is seen.
Polypoidal choroidal vasculopathy: Multiple and recurrent serosanguinous retinal PEDs resembling haemorrhagic detachment of AMD are seen. These serosanguinous detachments are often peripapillary, multifocal, orange, and nodular.ICG angiography demonstrates the presence of polyps.
Central serous retinopathy: It is seen in younger patients and subretinal haemorrhage is not usually seen.FFA shows a characteristic leak and areas of RPE atrophy.
Inflammatory conditions: Disorders like posterior scleritis, systemic lupus erythematosus, and Harada disease may cause serous elevation of the macula. They should be differentiated from CNVM based on other clinical features and FFA picture.
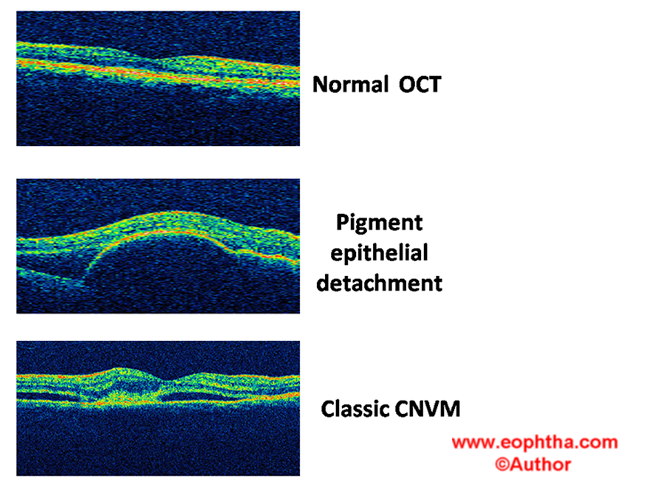
OCT features of CNVM:
A classic CNVM shows a thickening or disruption of the RPE-choriocapillaris complex and thickening of retina and subretinal fluid.
Occult CNVM shows a disruption of the RPE-choriocapillaris complex and most of the fibrovascular complex lies under the RPE.There may be associated subretinal fluid and retinal edema.
A serous PED is seen as an elevation of RPE with a clear space under it.
A fibrovascular PED is seen as an elevation of RPE with some amount of reflectivity under it.
A haemorrhagic PED is seen as an elevation of RPE with shadowing of the choroidal layers.
Treatment of CNVM:
There has been considerable progress in the way CNVM is treated;from thermal laser ablation to photodynamic therapy to pharmacotherapy.
Laser photocoagulation: This is used for classic CNVM or for classic CNVM with occult components where the lesion extent is well demarcated. It is used mainly to treat extrafoveal lesions and some juxtafoveal lesions only. The aim of therapy is to prevent further loss of vision. The disadvantage is that a central scotoma remains after therapy.
Photodynamic therapy: This is a treatment where first a photosensitizing agent is injected intravenously and is followed by application of light of a particular wavelength to the affected tissue to cause a localized chemical reaction which causes release of reactive oxygen species that lead to capillary endothelial cell damage and vessel thrombosis. Verteporfin is injected intravenously at a dose of 6mg/kg body weight over 10minutes.After five minutes of the injection, diode laser of 689nm wavelength is applied to the area of CNVM for 83seconds.Retreatment is done for areas of persistent or new leakage at three monthly intervals till the whole CNVM is obliterated.PDT has been approved by FDA for treatment of predominantly classic CNVM in AMD and for eyes with CNVM associated with pathologic myopia and ocular histoplasmosis.
Transpupillary thermotherapy: Here a diode laser of 810nm wavelength is applied over the area of CNVM for one minute. It is thought to act by slightly raising the choroidal temperature in a subtheshold manner thus treating the CNVM and causing only minimal damage to the overlying retina.
Pharmacotherapy: Various anti-vascular endothelial growth factor(VEGF)agents are being used as intravitreal injections to treat active CNVM lesions. The three drugs in use are pegaptanib, ranibizumab, and bevacizumab (used off-label). Pegaptanib blocks the 165 isoform of VEGF whereas ranibizumab and bevacizumab are not isoform specific. There are several trials on to determine the safety and efficacy and injection frequency of these agents. Clinical evidence indicates that ranibizumab initiation with three monthly injections of 0.5mg is optimal, providing the greatest visual acuity gain. After the initiation phase, the strongest evidence is for continued monthly treatment. As this is frequently not feasible, a flexible approach which requires monthly monitoring to capture signs of active disease and reinstate treatment without delay may be followed.
Surgical interventions for CNVM:
-
Pars plana vitrectomy to clear breakthrough vitreous haemorrhage.
-
Pneumatic displacement of submacular haemorrhage.
-
Submacular surgery to remove CNVM scar tissue.
-
Macular rotation to place healthier pigment epithelium at the fovea.
-
RPE pigment transplantation.
Supportive therapy:
Where the central vision is very poor, low vision aids may be advised.
References:
- Clinical Ophthalmology (5Th edition ) by J J Kanski
- Retina and Vitreous volume,Basic and Clinical Science Course ,American Academy of Ophthalmology;2007-2008edition.
- British Journal of Ophthalmology 2009: Ranibizumab in neovascular age –related macular degeneration :evidence from clinical trials.