“Never let good crises go to waste.” - - Winston Churchill
The Lockdowns are back, as the cities are once again bracing for a steep influx of patients suffering from or suspected to be infected from the novel coronavirus (COVID-19), owing to the soaring second wave of COVID-19. We as practicing ophthalmologists, need to keep our guard up now, more than ever. The need of the hour is the safety for our health, safety of the health of our health care workers and the patient’s health who visit our hospitals; along with simultaneously delivering high quality productive patient care. This drives the need for devising, effective and innovative safety strategies during the COVID-19 crises (Figure 1).
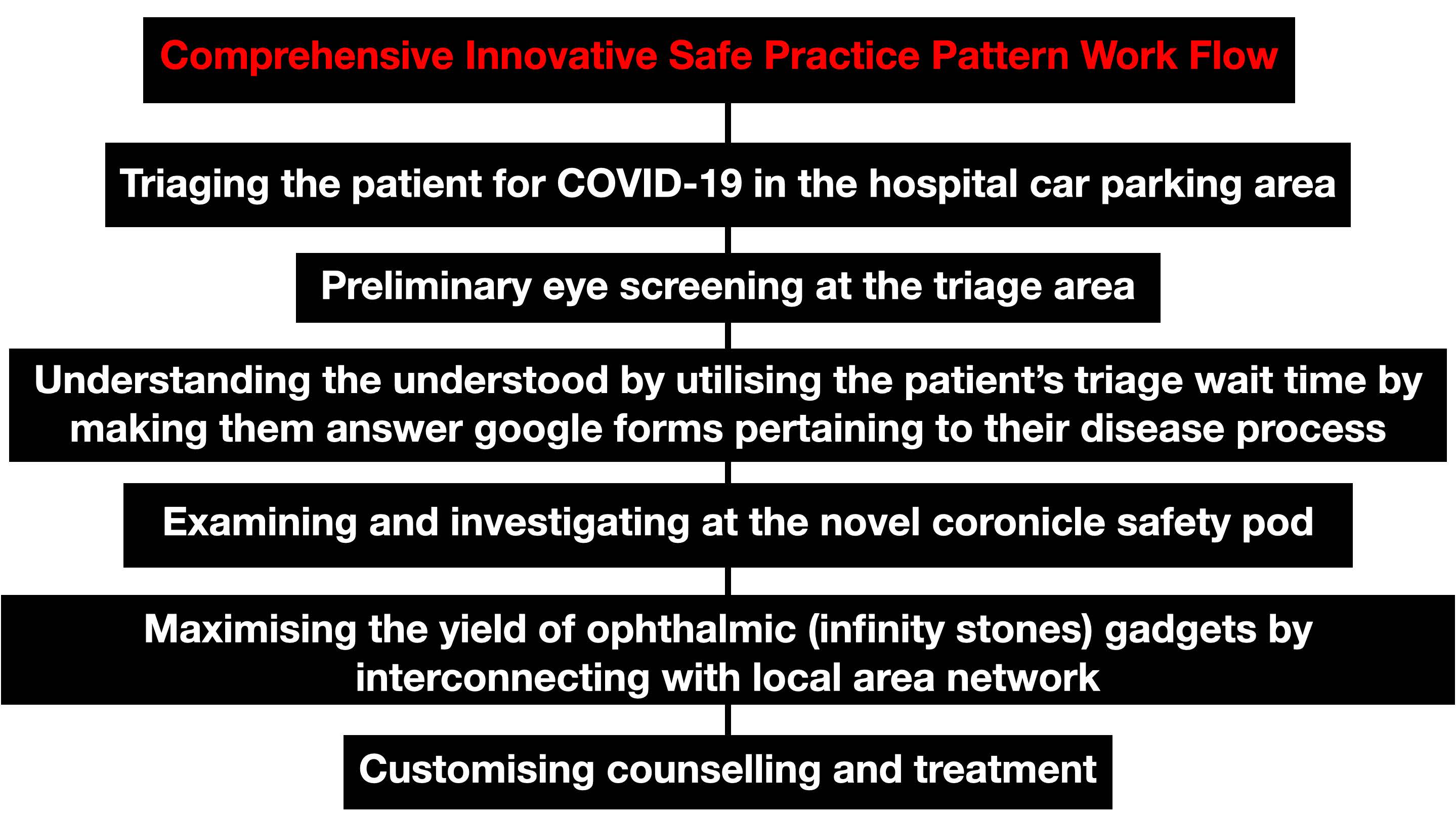
Utilization of hospital car parking area for COVID-19 triage
Triaging has become a mandatory part of our pandemic practice, but the dearth of available space for triaging needs to be addressed. The sprint is on as eye care professionals to make up for a woeful dearth of available hospital space, for triaging all outpatient department (OPD) patients. One such triaging strategy to ensure optimal screening for COVID-19 would be is to convert the hospital parking lot into a triaging zone.

We propose a novel cost-effective means of accommodating a triaging strategy in the underground hospital car parking garage present outside the hospital premises (Figure 2).[1] As the existing hospital parking garages are experiencing declines; due to the limitations of visiting inpatients, hospital parking structures may be suitable for non-parking purposes, like sorting out and classifying outpatients to determine the priority of need and proper place of treatment. In this regard, we developed an underground car parking triage standard operating protocol for screening possible COVID-19 patients for temperature, pulse oximeter measurement and obtain a COVID-19 consent form.[2]
All OPD patients are received in the car parking garage present outside the hospital premises. Upon arrival, they are asked to inform health-care providers if they have any symptoms of respiratory illness. Multiple audio-visual alerts through television are provided on proper donning of face masks and social distancing. Once body temperature and pulse oximetry are assessed and if within normal limits, the patient's uncorrected visual acuity is tested, followed by a preliminary examination and then allowed to enter into the hospital. The triage area is cleaned at least twice a day with special focus on frequently touched surfaces. Disinfection is done with 0.1% (1000 ppm) chlorine or 70% alcohol for surfaces that do not tolerate chlorine. For large blood and body fluid spills, 0.5% (5000 ppm) chlorine is utilised.[3] Also to avoid droplet transmission due to air-conditioning, usage of these devices is avoided and we propose using natural cross ventilation to supply fresh air.[4] Once this mandatory check point is cleared, the patient is allowed admission into the hospital for the final ophthalmic check-up at the novel cubicle created to prevent corona transmission.
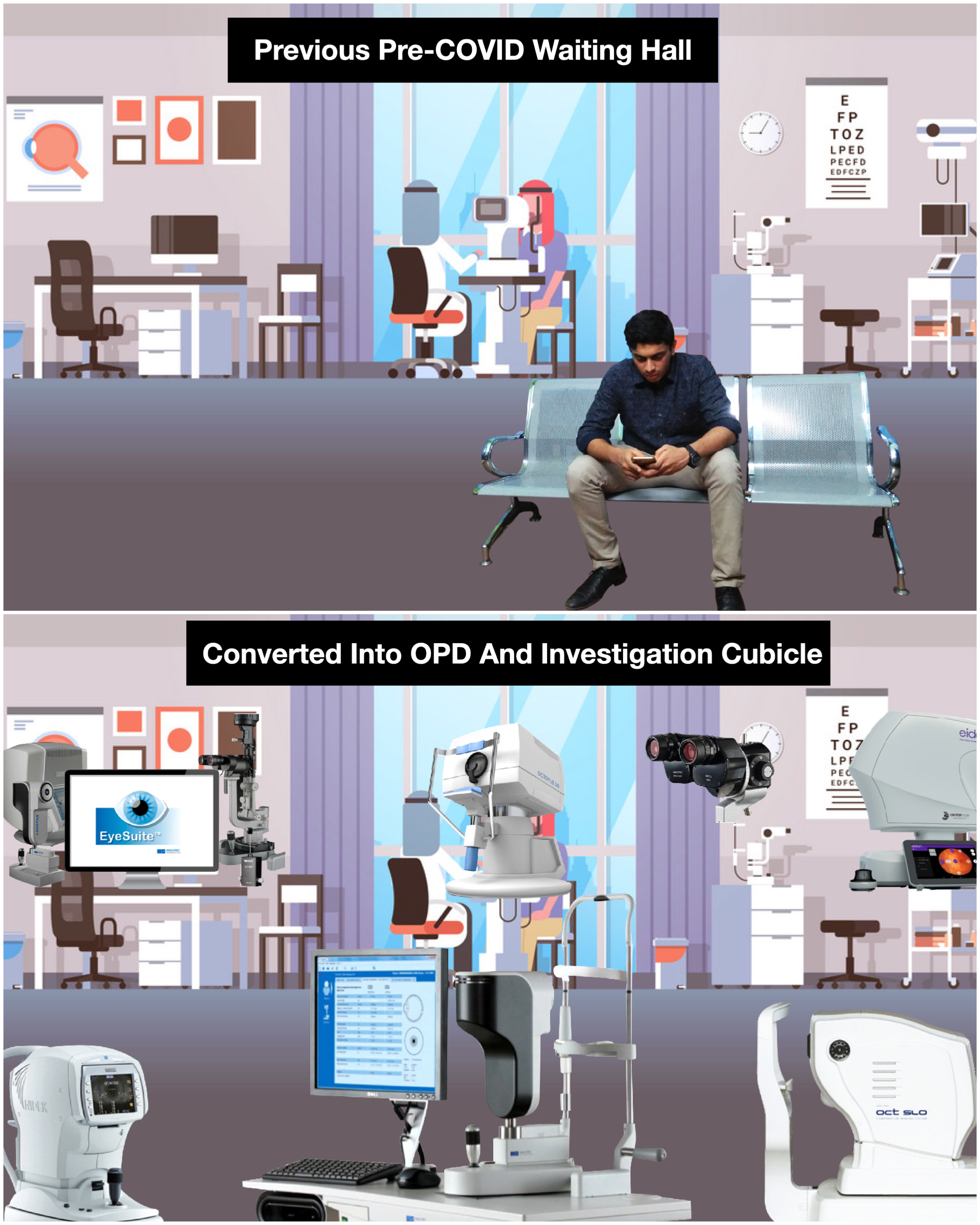

The Novel Coronicle Bubble - For Slit Lamp Examination and Ophthalmic Investigations
The coronicle (Corona + Cubicle) bubble provides us with an armamentarium of technology required to evaluate and manage all ophthalmic cases (Figure 3&4). Assembling this cubicle required 8 mm acrylic sheets and aluminium beading. The dimensions of the cubicle are 16*16 feet. Social distancing with minimum of three feet between equipments was incorporated while installing all the ophthalmic machines within the cubicle. This cubicle encompasses two slit-lamps, two electronic medical record (EMR) systems and one each of auto-refractometer, lensometer, confocal fundus capture device, spectral-domain optical coherence tomography (OCT), optical biometer, manual keratometer, corneal topographer and non-contact tonometer which are screen mirrored via a local area network (LAN) on the computer desktop present near the slit lamp. Additionally, each equipment has been fitted with an acrylic sheet of size 26.5 x 17.5 inches to provide a second layer of protection.[5] This cubicle was constructed keeping in mind the need for faster patient evaluation and disposal, and restricting the patient movement within the hospital premises, thus reducing the effective area utilised, contributing towards optimal surface sanitisation.
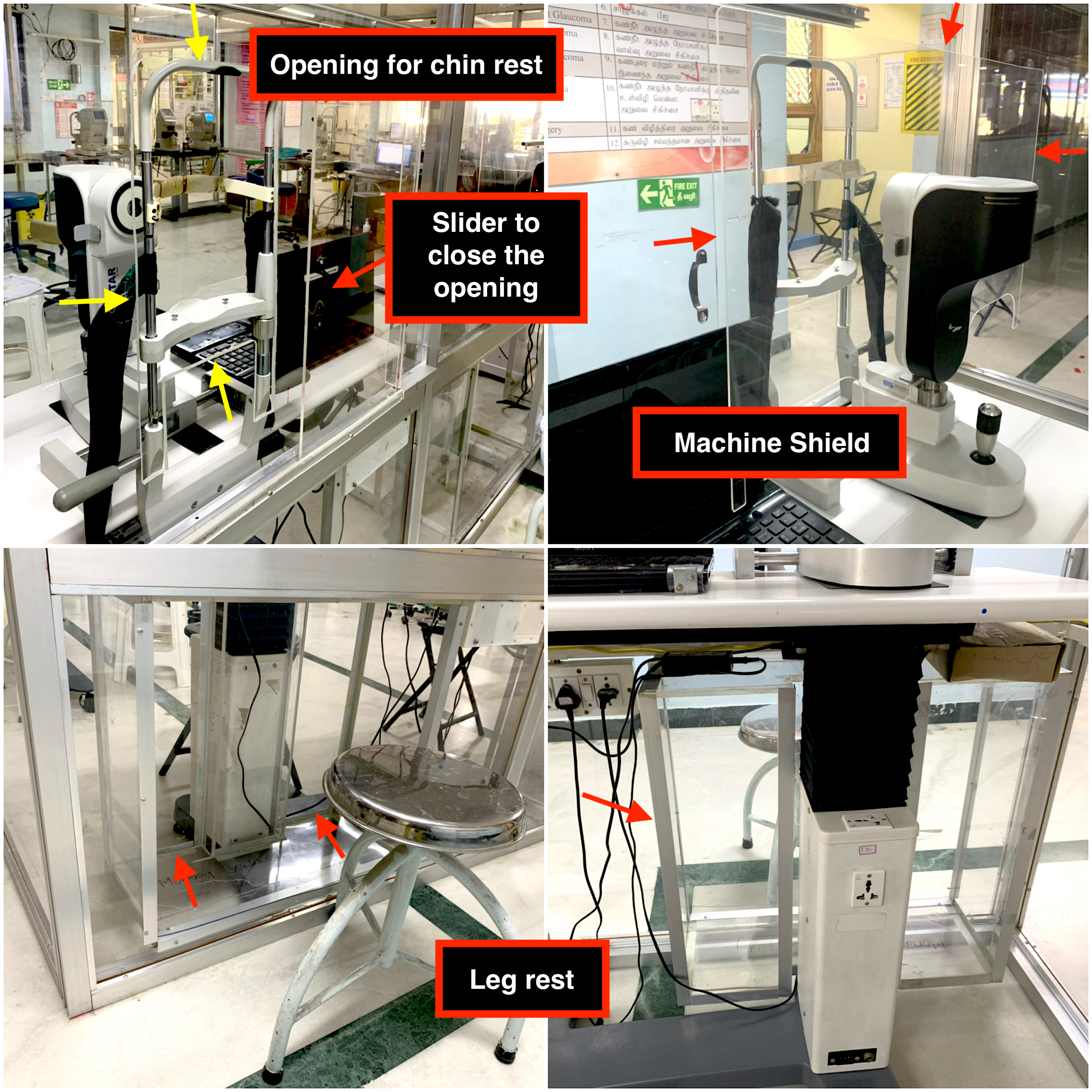
This innovative cubicle has been designed to provide ideal patient positioning with an acrylic groove below for accommodating the patient's feet, while the investigative test is underway (Figure 5). A well planned and customised opening has been made in front of each equipment for patient head and chin placement. In-between patients; the entire surface of the head rest opening and chin rest is sterilised using 70% isopropyl alcohol, and left to dry for 3 minutes.[6] A sliding acrylic door is provided to close the opening of the cubicle during times of disuse.
This cubicle has helped instil confidence and negate the rising panic among the doctors, hospital staff as well as the patient’s receiving treatment.
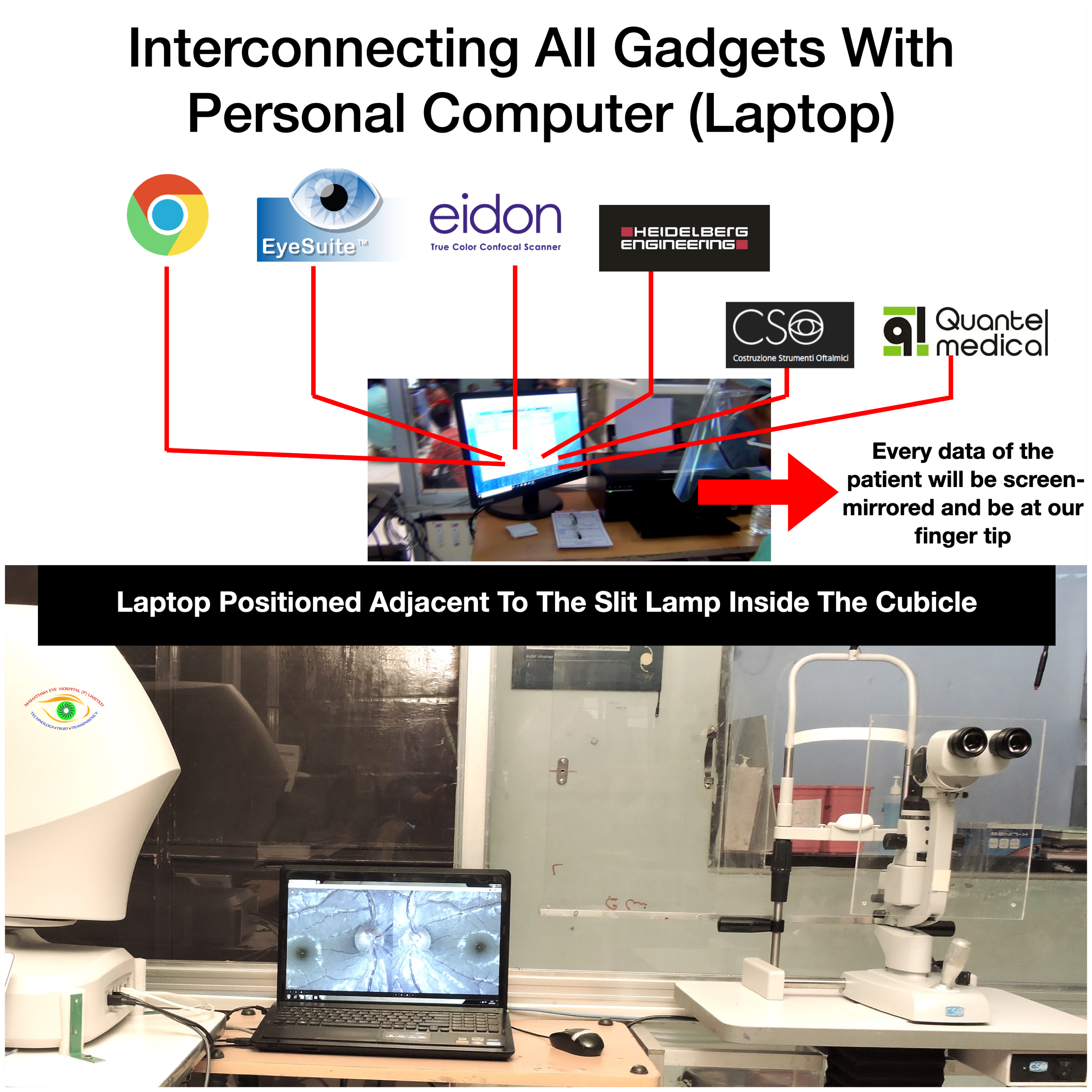
The Inception of Local Area Network in Ophthalmology For Interconnecting the Ophthalmic Infinity Stones (Machines)
Claiming the six infinity stones and interconnecting them in the gauntlet (in Marvel Cinematic Universe) gives the wielder tremendous power. Similarly in this pandemic, we have interconnected all the ophthalmic gadgets (fundus photography, optical coherence tomography, corneal topography, visual field analyzer, optical biometry, web browser and EMR) to the personal computer (PC) by LAN inside the coronicle (Figure 6).[7] For machines where LAN is not an option, interconnectivity can be achieved using a Wi-Fi network.[8] This is called WLAN (Wireless Local Access Network).
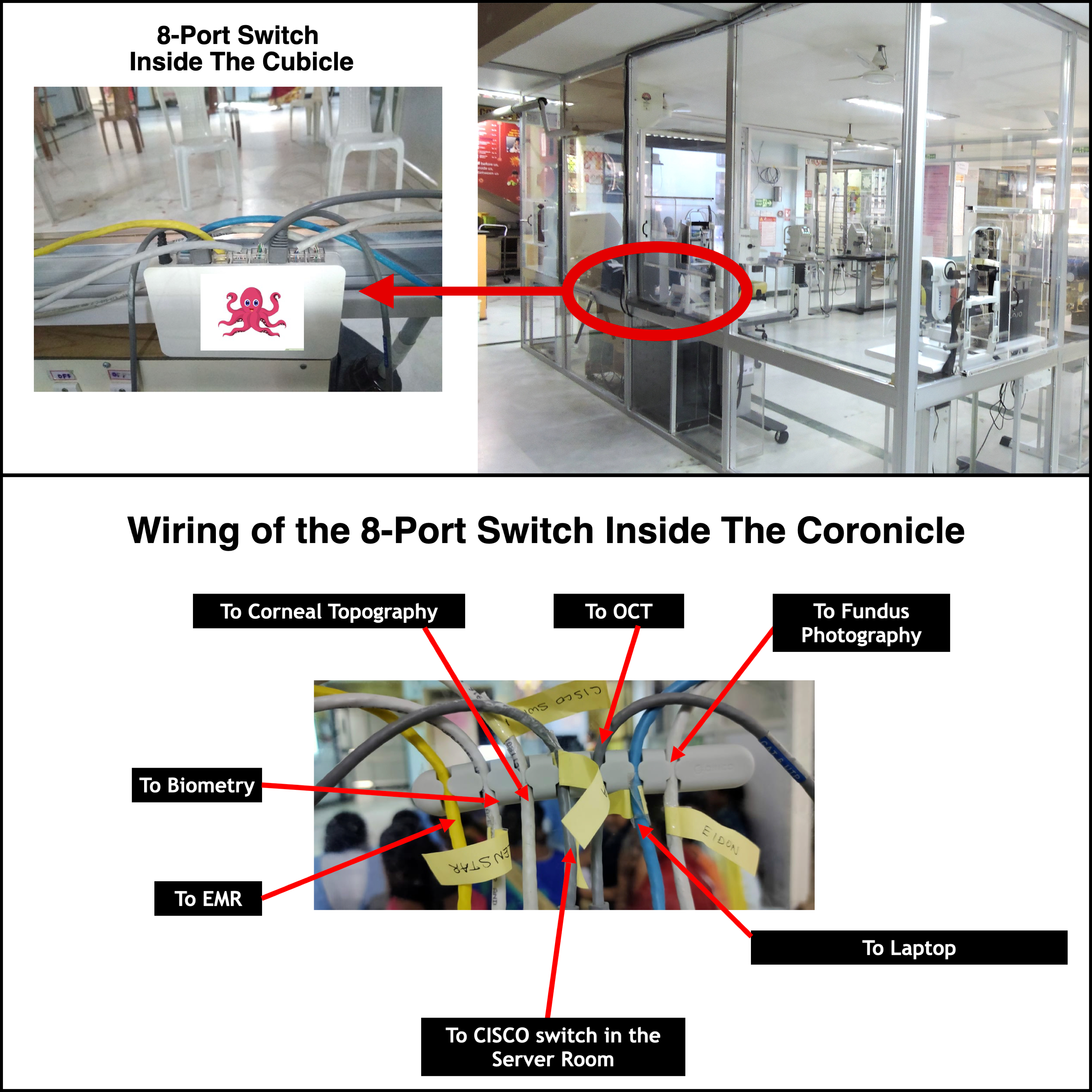
Setting Up The LAN Framework With The Octopus (Eight-port Switch) For Screen Mirroring
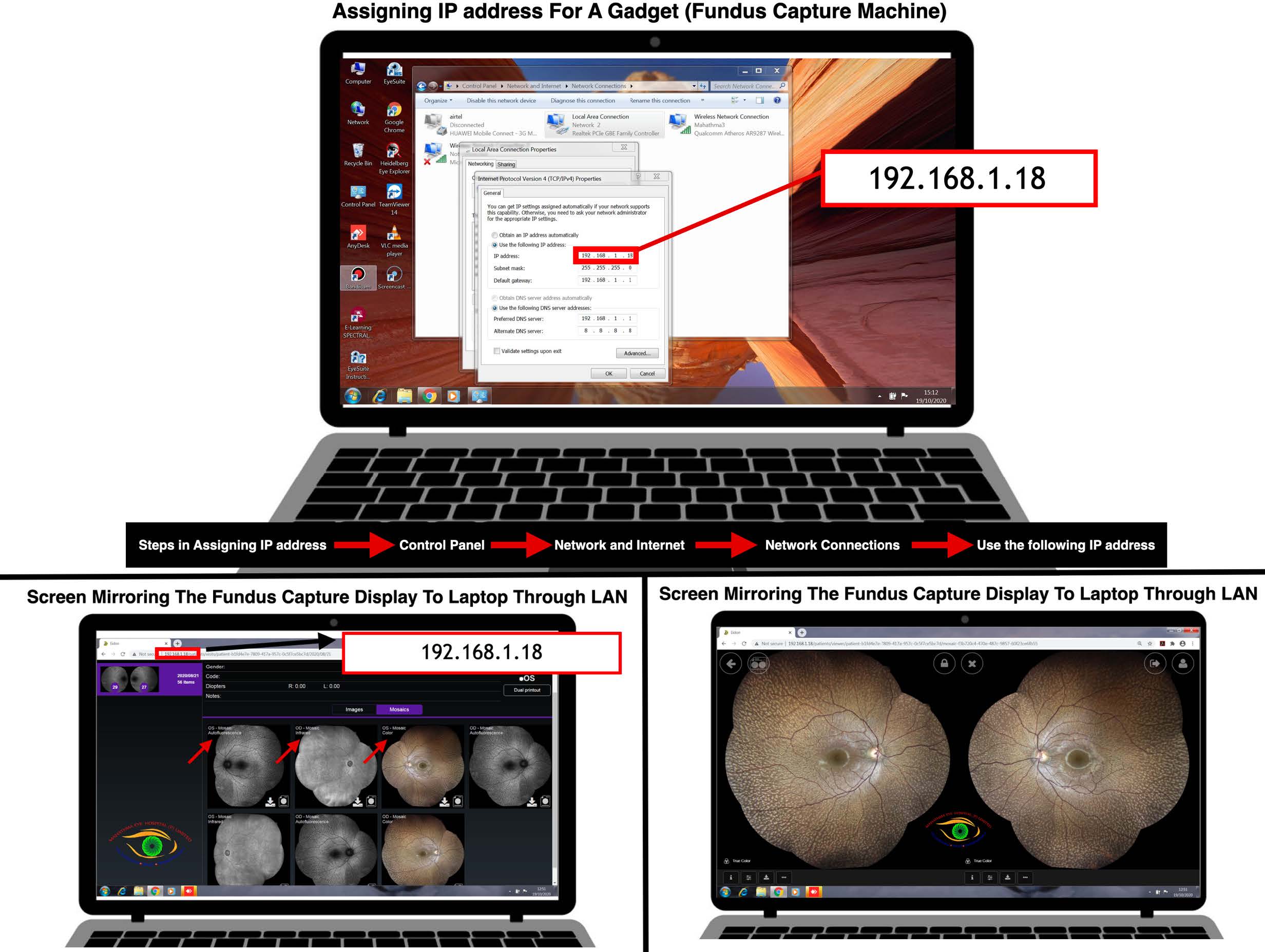
The LAN networking is established by an eight-port switch present inside the coronicle which finally relays to the CISCO (Commercial and Industry Security Corporation Switch) switch present outside the coronicle (Figure 7). CISCO enables the devices connected with it to share information and communicate with each other connected on the same network within the building. It also connects wireless access points, printers and servers on the same network for additional facilities. A working example of setting up a LAN connection, assigning an IP (internet protocol) address and screen mirroring is as follows. IP address can be assigned by following these simple steps (Control Panel->Network and Internet->Network Connections->Use the following IP address) (Figure 8). Each ophthalmic machine will have a unique IP address assigned. Once the IP address is assigned for a particular machine, the same address is entered in the web browser of the PC desktop placed near the doctor's slit lamp for activating the screen sharing relay display from the machine.[7]
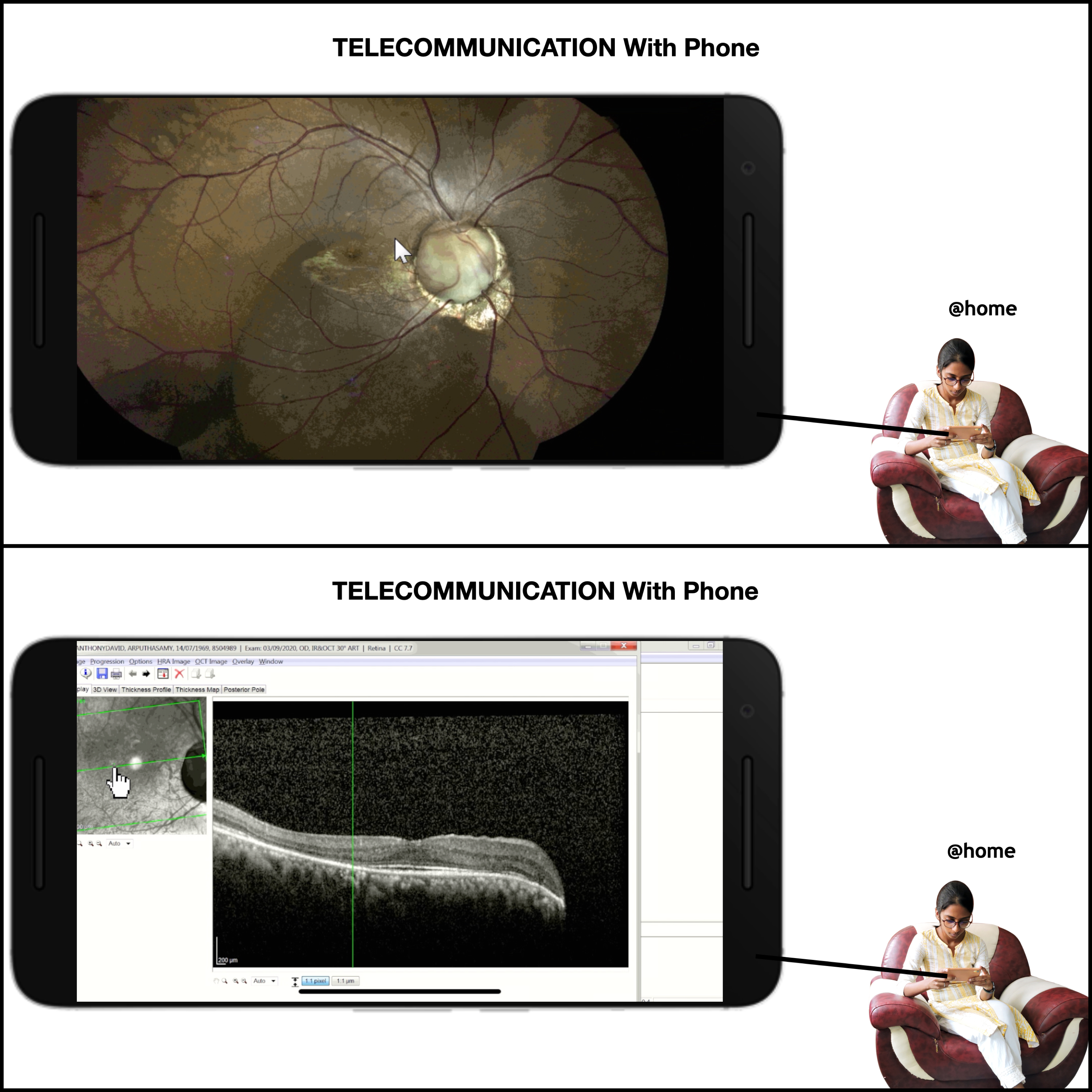
Role Of LAN In Telemedicine
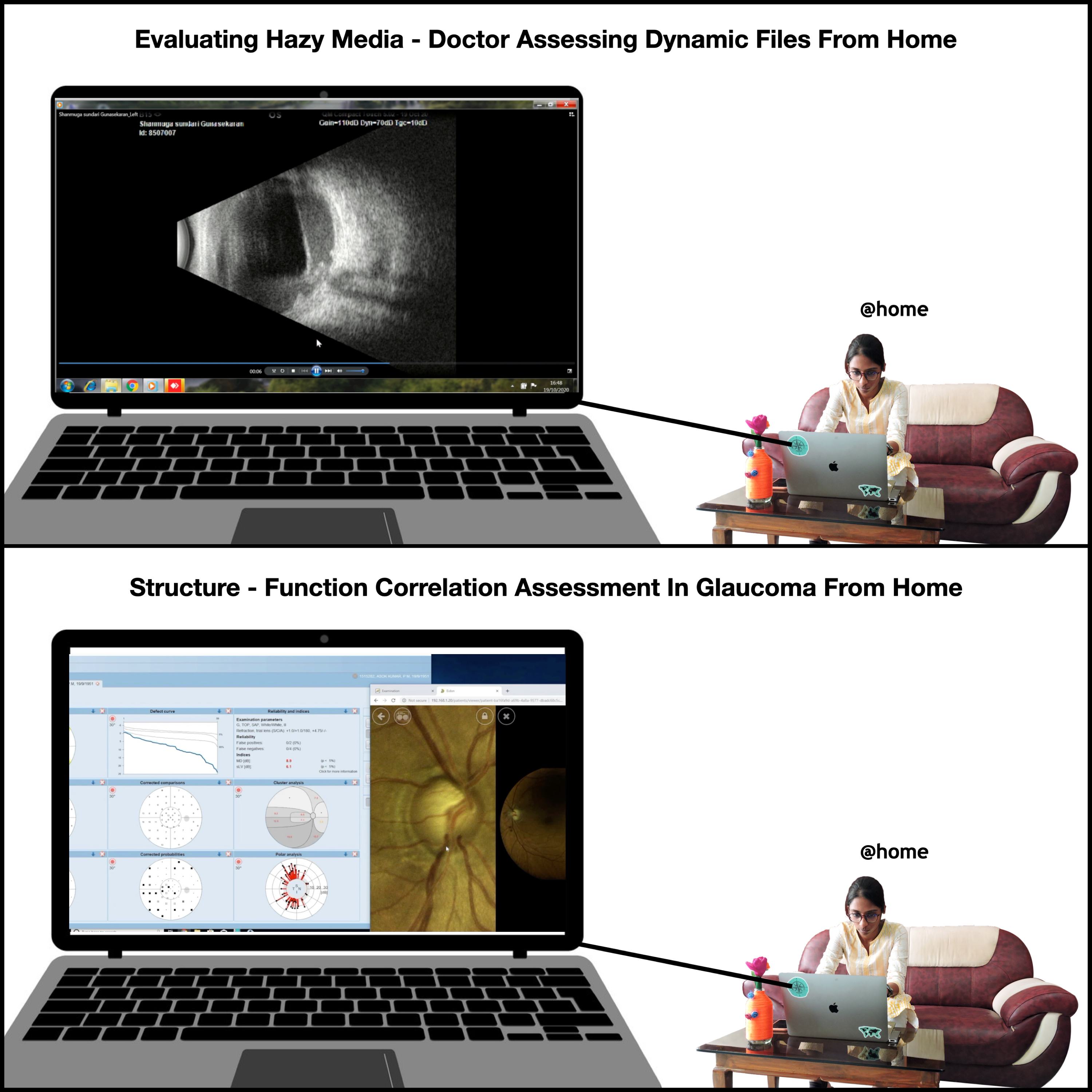
Connecting with remote desktop access tools are the most preferred and effective means for telecommunication using LAN. The five best desktop access tools available are TeamViewer, SolarWinds Take Control (Free trial), AnyDesk, Chrome Remote Desktop and Microsoft Remote Desktop. For eye care practitioners considering telecommunication using LAN, remote desktop access tools can be used in addition to the mandatory web interface tool for LAN which connects the device in your work place.[7]
Advantages Of LAN Over Electronic Medical Records (EMR)
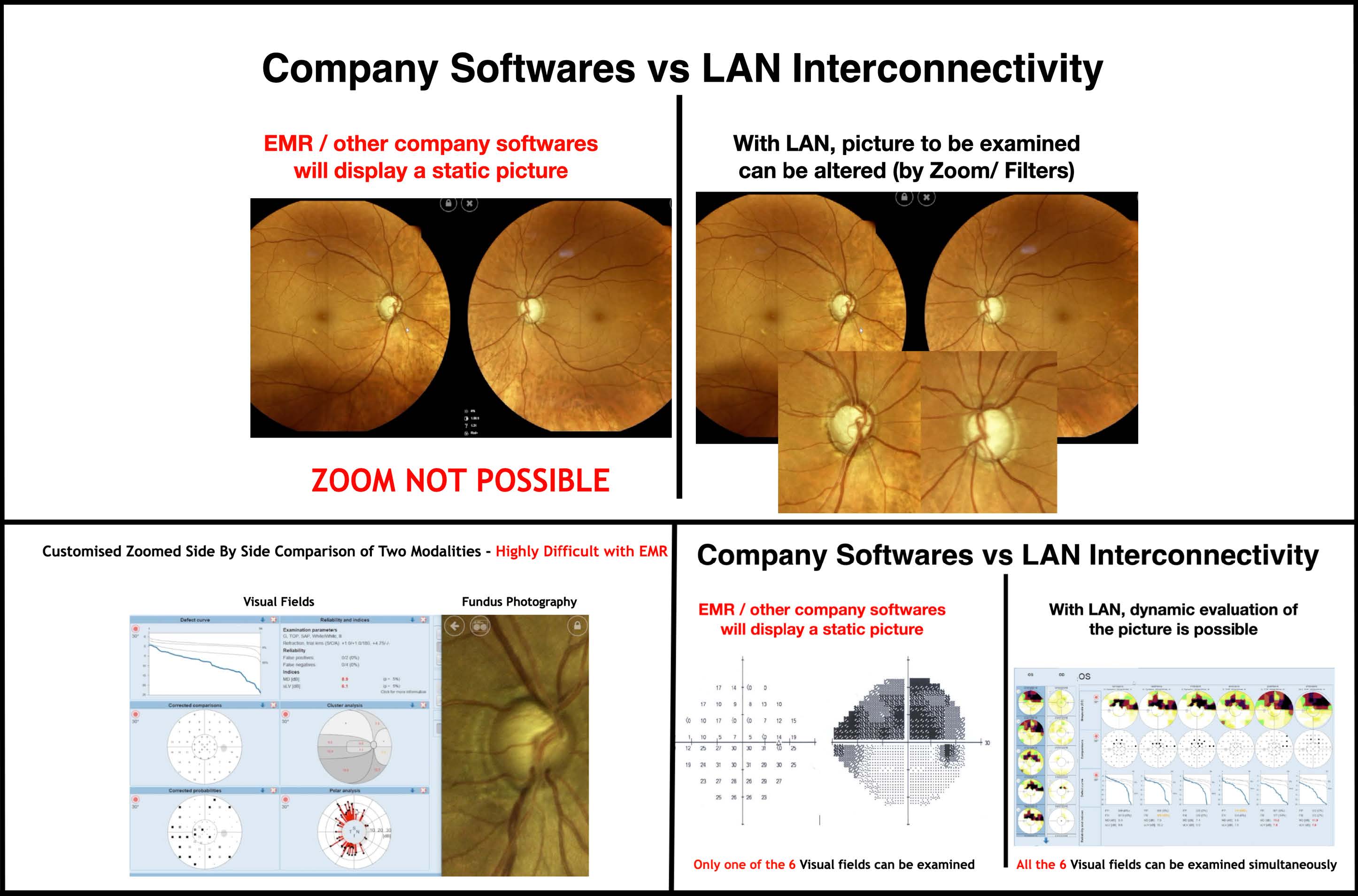
LAN has an innate edge over EMR softwares. This is because EMR softwares have fixed frame modules whereas the LAN display provides dynamic facilities such as zoom and multiple frames (Figure 9). Also, the data of every patient can be viewed immediately, once the patient has completed the evaluation. They can be compared, side by side with their previous baseline and other investigations in multiple sections (Figure 10&11). This serves as a smart time-saver (i.e.) doctor’s walking time to the investigative machine is reduced and patients can be counselled effectively by showing their own images. Finally, the patient's soft copy can be mailed or sent to their phone directly (from the machine through Bluetooth), so they will have the best copy for future reference. By going green, multiple paper handling can be reduced, avoiding aerosol mediated infection, during the pandemic.[7]
Understanding The Understood To Customise Health Care Delivery During COVID Crises With Integrated Information System
The one drawback of the coronicle was that the physical barrier hindered doctor-patient verbal communication. Hence, a do-it-yourself tool was implemented into the workflow pattern, to gather quantified information from the OPD patients, during their triage wait time and used the same data to make incremental improvements in practice delivery. Google forms with specific questionnaires and pictures containing items related to disease knowledge, awareness, investigations, management and compliance were provided to the patient’s mobile phones once they register in the OPD; and were made to answer the Google forms during their waiting time (Figure 12).[9]
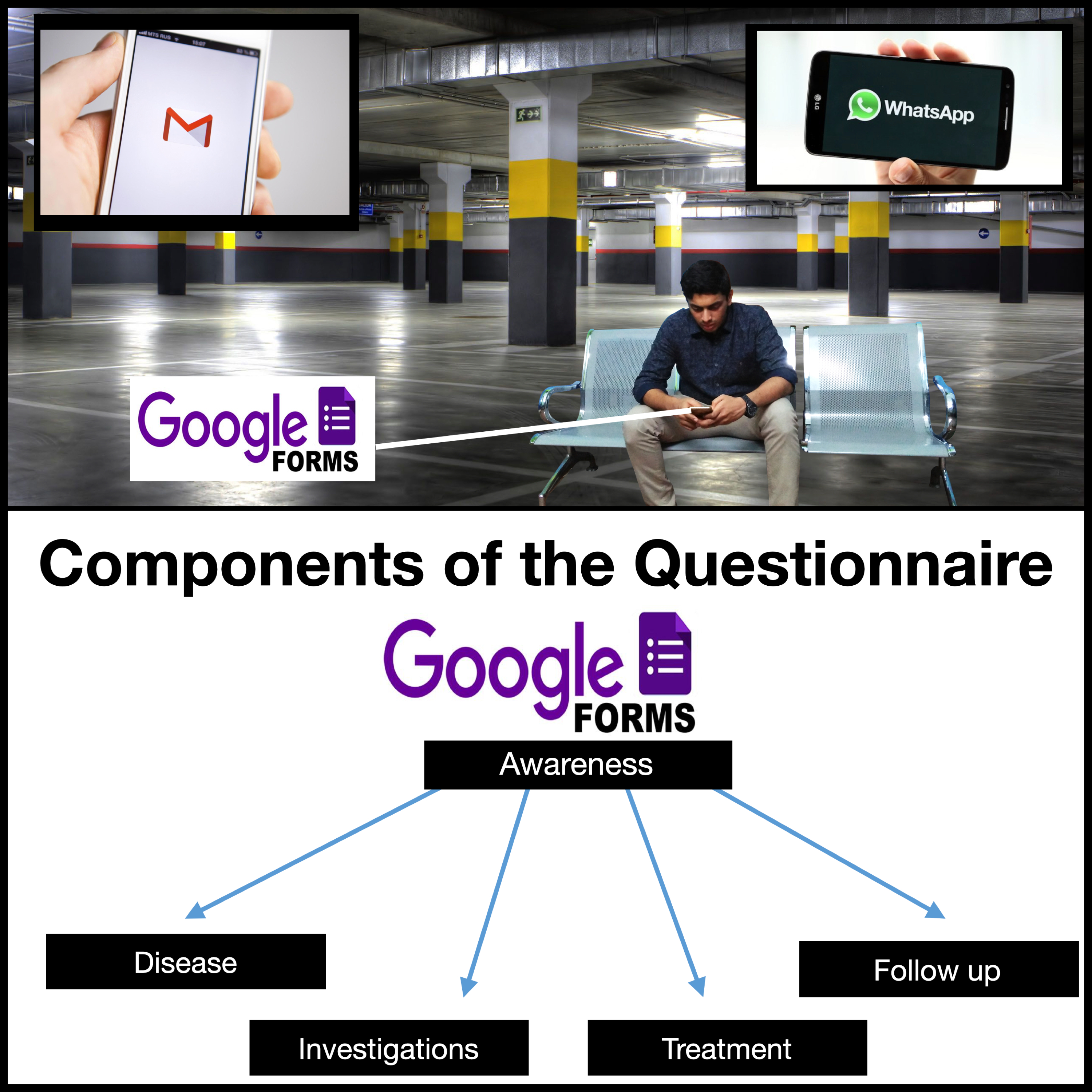
Their knowledge assessment regarding their specific disease will be done automatically once they have completed the survey and results were automatically generated to the doctor’s personal computer inside the coronicle, so that practice delivery can be customised according to the patient’s knowledge about the disease process (Figure 13). Understanding, how much the patient has understood will not only make them feel special and awe of our services but also throw light, in which specific category we need to strengthen the counselling for that individual, rather than a diffuse briefing that may not yield fruitful results.[9]
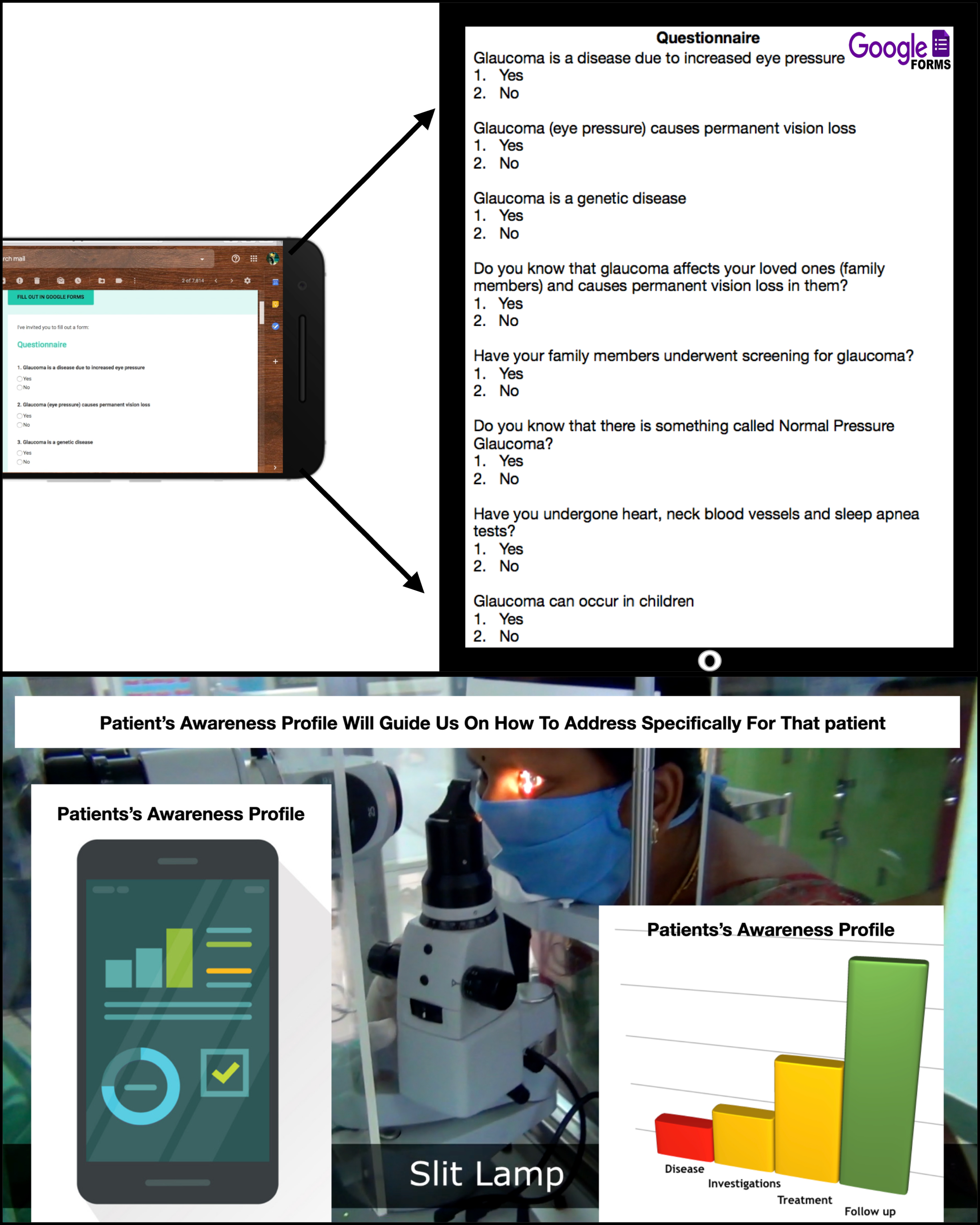
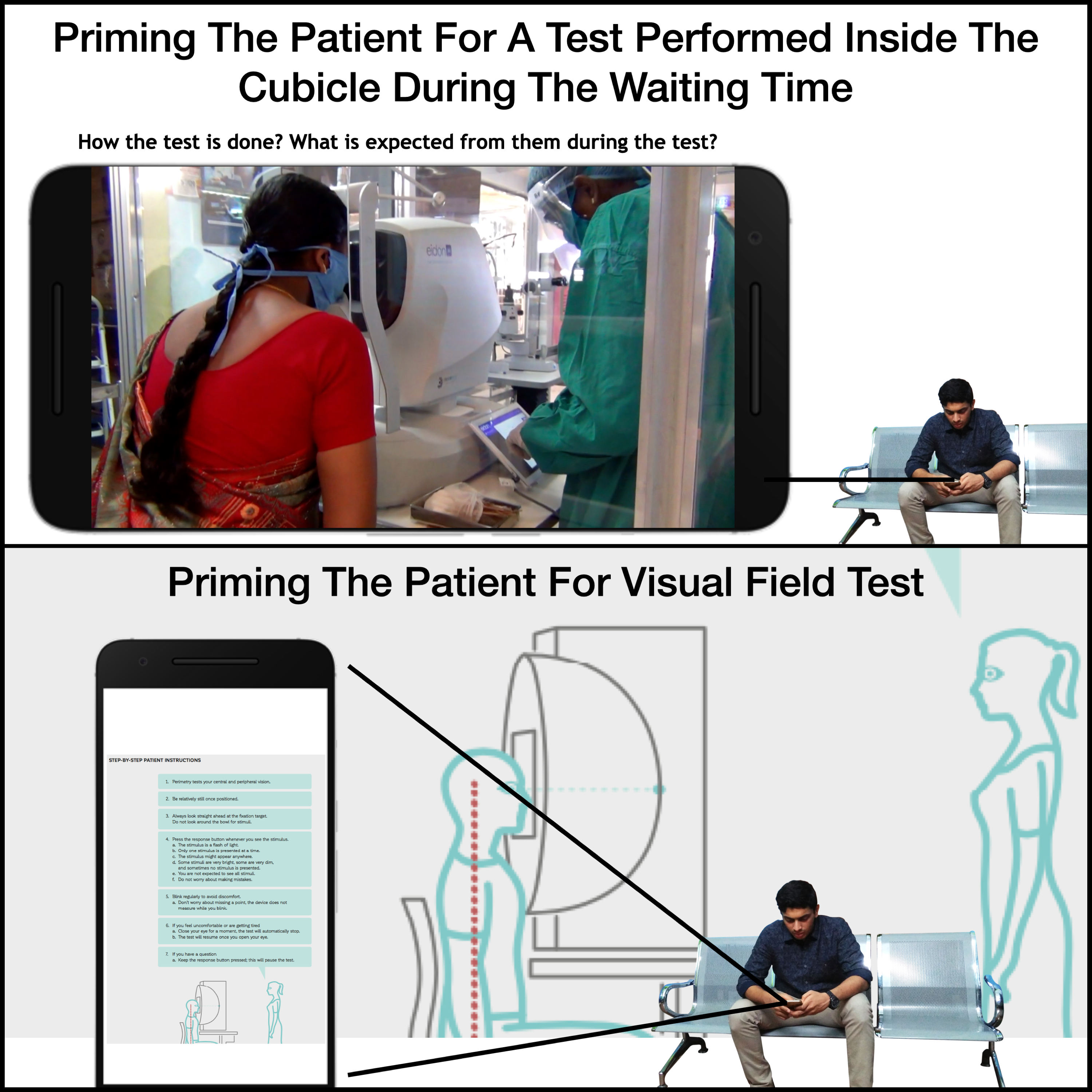
An additional feature of this tool is; it primes the patients during the waiting time with the do's and don'ts before an investigation for smooth performance of the examination (Figure 14). Furthermore, there will be an auto-generated SMS/email to the patient’s phone for their next investigation due/next review due, highlighting the need to analyze the disease's stability; serving as a vigilant medium.
Economics Factor
Costing of CISCO server with the switch is approximately one lakh rupees, costing of eight-port switch is approximately 5000 rupees and wiring required to achieve the LAN network may cost approximately 5000 rupees depending upon the area covered. Still, it is relatively cost-effective compared to an EMR.[7]
For sending the google forms and understanding the understood, all that is needed is a smart phone. In this era of smart phones; for 1.3 billion Indian population, there are at-least 1.8 billion mobile phones being used with 92.03 connections per 100 citizens. Among them, roughly half (49.7%) of the mobile phone users are smart phone users.[9]
Conclusion
According to our knowledge, there are no publications in literature depicting these comprehensive, novel and holistic practice pattern. We ophthalmologists who face additional difficulties due to the close proximity of evaluation and various entity of diagnostic procedures that have now become mandatory for an eclectic setup can avoid the proximity of evaluation with the help of LAN; and can customise patient care by understanding the understood with integrated information system, during these tough times of the pandemic.
References:
- Ramesh PV, Ramesh SV, Ramesh MK, Rajasekaran R. Utilization of hospital car parking garage for COVID-19 triage and screening in a high-volume tertiary eye care center. TNOA J Ophthalmic Sci Res 2021;59:114-6.
- Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol 2020;68:711-24.
- Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020;104:246-51.
- Experts suggest fresh air, ventilation may avert Coronavirus infection - ET HealthWorld [Internet]. ETHealthworld.com. Available from: https://health.economictimes.indiatimes.com/ news/diagnostics/experts-suggest-fresh-air-ventilation-may-avert-coronavirus-infection/ 74078415. [Last accessed on 2020 Aug 03].
- Liu J, Wang AY, Ing EB. Efficacy of Slit Lamp Breath Shields. Am J Ophthalmol. 2020 Oct 1;218:120–7.
- How To Clean Effectively For COVID-19 Using What’s Readily Available [Internet]. [cited 2020 Aug 5]. Available from: https://www.contecinc.com/articles/how-to-clean-covid-19
- Ramesh PV, Parthasarthi S, Ramesh SV, Rajasekaran R, Ramesh MK. Interconnecting ophthalmic gadgets (infinity stones) at finger tips (personal computer desktop) with local area network for safe and effective practice during COVID-19 crises. Indian J Ophthalmol. 2021;69(2):449-452.
- Riha C. How wireless LANs can enhance the clinical environment. Biomed Instrum Technol 2004. 2005;(Suppl):45–8.
- Ramesh PV, Parthasarathi S, Ramesh SV, Rajasekaran R, Ramesh MK. Innovative utilization of patient's triage with integrated information system during COVID crisis. Kerala J Ophthalmol 2021;33:87-90.

