Introduction
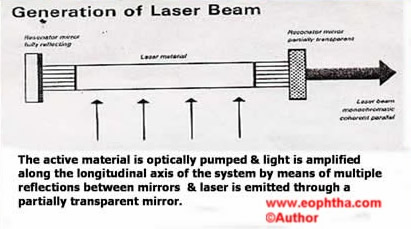
‘LASER’ is acronym for “Light Amplification by Stimulated Emission Radiation.” This describes the emission process by which an intense beam of electromagnetic radiation is generated
Basic Properties of Laser
Always monochromatic (one wavelength)
Collimated (all photons run parallel) & focused to a small point
Coherent (always in same phase)
Highest possible speed
Physics
Certain substances have property tolasei.e, absorb energy in one form & emit a new form of energy. On pumping these lasing substances electrons are transfered from a lower orbit to higher orbit(Bohr’s theory)
Excited atoms in turndecay backto their original orbit of lower energy, emitting photons (packets of energy)
Thisemissioncan bespontaneous or induced (stimulated)
Photocoagulation (PHC)
- Photothermal reaction
- Temperature elevation 10 to 20 deg C
- Protein denaturation
- Pigment dependent
- Argon, krypton dye, diode, frequency double Nd Yag
Tissue effects
Induces moderate sterile inflammation- Creates bio adhesion
Collagen shrinkage (Beneficial)
Membrane shrinkage (Harmful effect)
Ocular pigment absorption characteristics
Melanin – Entire visible range, 300 to 1300 nm
Hemoglobin – Blue & Green range 480 – 520 nm
Xanthophyll – Blue 488 nm
Hence, when treating macular areaavoid blue lasersto avoidinadvertent damagetomacula. Argon green, doubled frequencies NdYag, 577dye are lasers of choice for macular photocoagulation
Laser delivery systems
- Slit lamp
- Laser indirect ophthalmoscope (LIO)
- Endo laser
Chorioretinal burn intensity classification
- Light – barely visible retinal blanching
- Mild – faint white retinal burn
- Moderate – opaque dirty white retinal burn
- Heavy – dense white retinal burn
Prerequisites for retinal PHC
Informed consent
Dilated pupil 4mm
Anaesthesia-Topical / retrobulbar
Fundus contact lens / 3 or 4 mirror contact lens/ panfudoscopic lenses
Panfundoscopic contact lenses most commonly used
- Rodenstock panfundoscope
- Mainster wide field
- Goldmann 3 mirror
|
Contact lens |
Spot size on retina (μm) |
|
Spot selector set at 200μm |
|
|
Goldmann 3 mirror |
216 |
|
Rodenstock panfundus |
286 |
|
Mainster wide field |
294 |
Pan retinal photocoagulation (PRP)
Indications
- Proliferative diabetic retinopathy (PDR)
- Retinal vascular obstructions (CRVO)
- Retinal vasculitis
- Ocular ischemic syndrome
Laser parameters
Spot size 200-500 microns
Duration 0.2 to 0.5 seconds
Power 140 – 200 mW depending on media clarity. Aim is to create a moderate intensity burn. Each burn should be at least 1 burn width apart. 900 burns are required for each half of the retina. Total of 1800 to 2200 burns for complete treatment PRP
The technique (slit-lamp delivery)
Under topical anaesthesia, place lens by asking patient to look up at the same time retracting lower lid. Once lens is placed, focus to obtain clear view of retina.
Treatment completed in 2 sessions. Inferior half of retina is treated in first session (because if vitreous hemorrhage occurs then it would be difficult to do inferior half) and then superior half after 15 days.
Temporally start 3000 microns away form the foveal center (Figure 1).
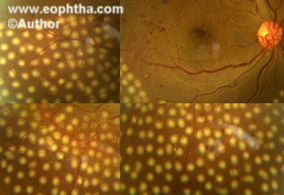
Figure 1: Fundus photo of RE showing the temporal extent of PRP laser
Nasally do not go closer than 500 microns along the margin of the optic disc (Figure 2)
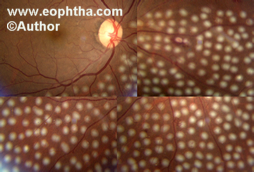
Figure 2: Fundus picture of RE showing nasal extent of PRP laser.
Laser indirect ophthalmoscope (LIO) delivery
Indications
Media opacities like dense cataracts, vitreous hemorrhage
Treat peripheral areas like retinal holes /tears
Patients who cannot sit for long duration (morbid)
Parameters used is similar to that of slit lamp delivery system except higher power may be required in dense media opacities
Endolaserin direct laser inside the eye with an endolaser probe during parsplana vitrectomy.
Scatter photo coagulation is 360 degree PRP given with each burn should be at least 2 burn width apart. Total of 800 to 1000 burns are required for complete scatter PRP (Figure 3)
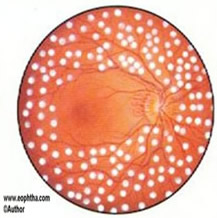
Figure 3: Scatter laser PRP.
Indications
Very severe NPDR (when the other eye has already got advanced PDR)
Early PDR
Focal/grid photocoagulation
Indications
Clinically significant macular edema (CSME)
Pin point leaks in central serous chorioretinopathy (CSCR)
Branch retinal vein occlusions (BRVO)
Laser parameters
Spot size 50-100 microns
Duration 0.1 seconds
Power 50-100 mW to blanch RPE / microaneurysms (light to mild intensity)
Focal laser is done for focal maculopathy. The laser is given directly to the microaneursyms situated between 500 to 3000 microns from fovea. This stops leakage by direct closure of microaneursyms by vascular thrombosis –direct focal treatmentfor focal maculopathy (Figure 3). If vision is less than 6/9 with persistent edema and good peri foveolar network on FFA then focal laser upto 300 microns from fovea can be considered. The spot size should be reduced to 50 microns and duration to 0.05 second.
Gridpattern of laser is given for diffuse diabetic macular edema. The laser is applied to edematous areas avoiding foveal avascular zone (FAZ), around 500 microns from fovea. The spacing should be one burn width apart. It can be given in papillomacular bundle also but it should remain 500 microns from the disc (Figure 4).
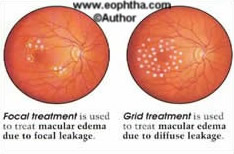
Figure 4: Shows focal and grid laser.
Modified grid is when grid laser is given only in the edematous area in a grid form (Figure 5).

Figure 5: Fundus picture of RE & LE showing modified grid laser.
Content on this page requires a newer version of Adobe Flash Player.
Video 2 shows technique of focal laser.
What is PASCAL laser?
PASCAL (Pattern Scan Laser) Photocoagulator1 is the latest laser machine. It is a semi-automated pattern generation technique that allows the rapid delivery of 532 nanometer laser pulses in a predetermined sequence. (Figure 6)
Advantages:
- Very fast and more efficient than standard single shot
- Improved comfort:Patients are likely to experience less discomfort and therefore have more tolerance for the procedure. Full 360 degrees PRP can be done in a single sitting
- Advanced precision: Macular Grid treatment provides an improved margin of safety and dosimetry control when compared with single shot treatments. Unlike the irregular pattern placement obtained in single shot photocoagulation, PASCAL delivers even pattern burns.
- Ease of use: The PASCAL method of photocoagulation is similar to single shot photocoagulation, therefore physician training is minimal.
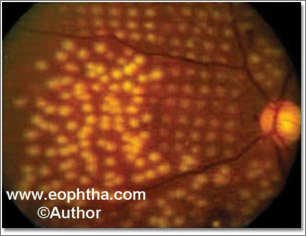
Figure 6: Burns on the left side of the fundus photograph were the result of conventional, single spot photocoagulation; arrayed burns on the right are obtained with the Pascal method of photocoagulation.
For more information on PASCAL with clinical videos visithttp://www.optimedica.com/Pascal-Method/
References
- Classification and treatment of Diabetic Retinopathy: diabetic maculopathy In: AMP Hamilton, MW Ulbig, P Polkinghorne, editors.Management of Diabetic Retinopathy. 1st Indian edition reprint 2003 Jaypee Brothers medical publishers Pvt Ltd New Delhi; 2003;
- YK Dastur (1994) The rationale of argon green laser photocoagulation for diabetic maculopathy OPHTHALMOLOGY Vol 40,13-17
- Rosenblatt RJ, Benson WJ. Diabetic Retinopathy. In: Yanoff M, ed.Opthalmology. 2nd ed. St. Louis, MO: Mosby; 2004;877-887.
- Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. The Early Treatment Diabetic Retinopathy Study Research Group. Int Ophthalmol Clin. 1987 Winter;27(4):254-64.
Photodynamic therapy (PDT)
Principle
To injectphotosensitizer (verteporfin dye)1 intravenously, followed byirradiationof the photosensitized tissue bynonthermal lightat an absorption peak of the photosensitizer dye.
The excited photosensitizer generates singlet oxygen or other reactive intermediates, which selectively2,3 damages cellular components, including cellular membranes.
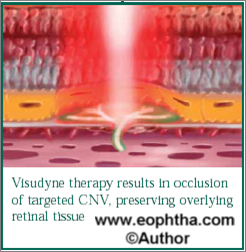
Mechanism of action
Selective uptake of verteporfin by neovascular membrane + Selective area of laser light application
= Localised generation of singlet oxygen & free radicals
= Endothelial cell damage
= angio occlusion of CNVM avoiding overlying retina
Indications4
- Choroidal neovascular membrane (CNVM) secondary to wet age related macular degeneration (ARMD) (upto 5400 mic in size)
- CNVM due to polypoidal choroidal vasculopathy (PCV)
- CNVM due to myopic degeneration
- Idiopathic CNVM
- CNVM secondary to choroiditis and retinochoroiditis, angioid streaks, central serous chorioretinopathy, retinal angiomatous proliferation, parafoveal telangiectasia
- Others such as choroidal hemangioma, retinal hamartoma, choroidal melanoma, chronic central serous chorioretinopathy, angiomatous lesions secondary to systemic diseases.
Technique
- Written informed consent
- Fundus flourescein angiography is done (NOT Less than 72 hours old)
- Late venous phase frames are selected where the entire nevascular membrane fills up & greatest linear diameter (GLD) of lesion is calculated.
- Laser spot size = GLD + 1000microns. Dose of verteporfin= 6mg/m2
- Nomogram is available for dose calculation based on body mass index (BMI).
- Reconstitute each vial of Visudyne with 7 ml of sterile water for injection to provide 7.5 ml containing 2 mg/ml. Reconstituted Visudyne must be protected from light and used within 4 hours. It is an opaque dark green solution.
- The volume of reconstituted Visudyne required to achieve the desired dose of 6 mg/m2 body surface area is withdrawn from the vial and diluted with 5% dextrose for injection to make a total infusion volume of 30 ml. (eg if dose is 4.5 ml then the drug is diluted with 25.5 ml of 5% dextrose). After dilution, protect from light and use within a maximum of 4 hours.
- This 30 ml is then infused slowly over 10 minutes with the help of an infusion pump with anaesthesiologist stand by, in a dark room
- 5 minutes after the infusion is over, laser of 689 nm is applied for 83 seconds (both eyes can be treated in same session)
- Patient is kept in dark room for 48 hours and discharged
- Patient advised to avoid direct sun light exposure for 15 days to prevent photosensitization reactions
- Patient is informed about discoloration of urine, tears and sweat
- Retreatment after 3 months if needed
Complications
Photosensitivity reactions
Adverse events at the injection site (such as pain, edema, hemorrhage, or inflammation)
If extravasation occurs, protect the site from light
Transient visual disturbances
Nowadays combination treatment of PDT with anti VEGF injections (given 48 hours after PDT) is the standard of care. PDT as a monotherapy is not been done.
References
- Aveline, B, Hasan, T, Redmond, RW (1994) Photophysical and photosensitizing properties of benzoporphyrin derivative monoacid ring A (BPD-MA)Photochem Photobiol59,328-335
- Schmidt–Erfurth, U, Hasan, T, Gragoudas, E, Michaud, N, Flotte, TJ, Birngruber, R. (1994) Vascular targeting in photodynamic occlusion of subretinal vesselsOphthalmology101,1953-1961
- Miller, JW, Walsh, AW, Kramer, M, et al (1995) Photodynamic therapy of experimental choroidal neovascularization using lipoprotein-delivered benzoporphyrinArch Ophthalmol113,810-818
- SivaprasadSobha; HykinPhil. The role of photodynamic therapy in ophthalmology British journal of hospital medicine 2006 vol 67 ,647-650

