Basic histology of the eye
Eyelid:Each eyelid consists of skin, subcutaneous tissue, striated muscle fibers of orbicularis oculi, orbital septum and tarsal plates, smooth muscle and conjunctiva. The skin contains sebaceous glands and small sweat glands.The eyelashes are more numerous in the uppereyelid than in the lower. The sebaceous glands of Zeis open into each follicle.
Histological photograph of eyelid
Conjunctiva:The conjunctiva is made up of an epithelium consisting of stratified columnar cells resting on a lamina propria of loose connective tissue, the submucosa. At the limbus there is a change to stratified squamous nonkeratinised epithelium which is continuous with the corneal epithelium. At thelimbus, the laminapropria forms the papillae. On the posterior edge of the lid margin, the conjunctiva joins the skin. Here the nonkeratinised squamous epithelium of the conjunctiva becomes continuous with the keratinized stratified squamous epithelium of the epidermis. The conjunctival submucosa consists of loose connective tissue comprising of lymphocytes, blood vessels, nerves, smooth muscle and accessory lacrimal glands.
Cornea:It is composed of 5 layers. The superficial layer is composed of stratified squamous epithelium. Bowmans membrane layer is the next layer, which is acellular. The corneal stroma contains collagen fibers and keratinocytes. Descemets membrane is an elastic membrane which lies between the endothelium and stroma. Endothelium contains flat hexagonal cells.
Sclera: Sclera can be divided in to 3 layers:
The episclera: outermost layer consisting of loose connective tissue. It is connected to the fascial sheath of the eyeball(tenon’s capsule) by fine strands of tissue. It has a rich blood supply.
Scleral stroma: This consists of dense fibrous tissue intermingled with fine elastic fibers. Occasional fibrobasts along with melanocytes are seen between the collagen bundles.
Lamina fusca: It is the innermost layer of the sclera. It contains melanocytes which form a thin irregular layer. The lamina has many grooves caused by passage of vessels and nerves. It is separated from the external surface of the choroid by a potential space(perichoroidal space). Few collagen fibers connect the lamina fusca with the choroid.
Iris:It consists of 2 layers; stroma anteriorly and 2 epithelial layers located posteriorly. The iris stroma is a loose fibrocollagenous tissue composed of spindle shaped fibroblasts, blood vessels, nerves and macrophages. At the pupillary margin is the circumferentially arranged smooth muscle of the sphincter muscle of the iris. The posterior epithelium is composed of two layers of cells, the posterior of which is densely pigmented with melanin. The posterior boundary of the iris stroma, peripheral to the sphincter muscle, is demarcated by the dilator muscle.
Ciliary body: It is shaped like a triangle with apex towards the ora serrata posteriorly and base towards iris root anteriorly. The The pars plicata contains about 70 ciliary processes, which are ridges or folds 2, each with a core of stroma and blood vessels and covered by two layers of columnar epithelium.
The pars plana is a posterior flat area 4 mm long. Its stroma is continuous with the choroid, whereas the outer pigmented epithelium of the ciliary body is continuous with that of the retina at the ora serrata.
The ciliary body faces the anterior chamber, posterior chamber, and vitreous cavity and is lined by two neuroepithelial layers, a non-pigmented layer internally and a pigmented layer externally. The outer layer of epithelium is pigmented, but the inner layer, which is in contact with the aqueous is non-pigmented. The nonpigmented epithelial cells secrete the aqueous humor.
Choroid: The choroids is divided into 3 layers: vessel layer(comprising of loose connective tissue with melanocytes and large and medium sized blood vessels), capillary layer(consists of network of capillaries with sac like dilatations) and Bruch’s membrane (consists of basement membrane of endothelium of capillaries of capillary layer, an outer layer of collagen fibers, meshwork of elastic fibers, inner layer of collagen fibers and basement membrane of the pigment epithelium of retina)
Retina: The retina is composed of 10 layers, from outside inward:
Pigment epithelium, rods and cones, external limiting membrane, outer nuclear layer, outer plexiform layer, inner nuclear layer, inner plexiform layer, ganglion cell layer, nerve fiber layer, internal limiting membrane .
The foveola contains only photoreceptors in the centre. The periphery of the foveola contains nerve cells and fibers of inner cell layers of retina.
Optic disc: The optic nerve is covered by 3 layers of meninges and contains nerve fibers along with central retinal artery and vein.
Lens: The lens consists of an elastic capsule (elastic basement membrane enveloping the entire lens, has a homogenous appearance), lens epithelium (cuboidal, lies beneath the capsule and found on the anterior surface of the lens), lens fibers (main mass of the lens and consists of elongated cells)
Terminologies in histopathology:
Hyperkeratosis:
This refers to an increase in the amount of keratin. Clinically, this appears as scale or horn on the surface of the lesion. This can occur in many different lesions both benign or malignant.
Fig:Hyperkeratosis
Parakeratosis:
This term refers to the retention of nuclei within the keratin layer. This sign indicates shortened turn-over of the epidermis.
Fig: Parakeratosis
Fig: hyperkeratosis and parakeratosis with horn cysts
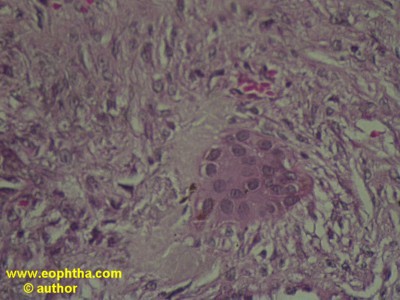
Dyskeratosis:
This term refers to cell keratinization within the epidermis rather than at the surface as is normally the case. An aggregate of such cells forms a keratin pearl or eddy.
Dysplasia:
It is used to describe cells that show aberrant growth and differentiation. It is seen as nuclear hyperchromasia, increased cell size (disordered differentiation) and increased number (aberrant growth). Dysplastic cells lie in a continuum between benign and fully malignant.
Acanthosis:
Acanthosis implies increased thickness of stratum spinosum layer
Acute inflammation:
Acute inflammation is the initial response of the body to harmful stimuli and is achieved by the increased movement of plasma and leukocytes (especially granulocytes ) from the blood into the injured tissues. Histopathologically, plenty of neutrophils, eosinophils and lymphocytes are seen with dilation of blood vessels and tissue edema.
Chronic inflammation:
Prolonged inflammation leads to chronic inflammation, leads to a progressive shift in the type of cells (macrophages and plasma cells) present at the site of inflammation and is characterized by simultaneous destruction and healing of the tissue from the inflammatory process.
Giant cellsare transformed macrophages. There are three main types of giant cells seen in chronic inflammation and each has a typical histopathological feature.
Fig:Giant cell
Langharn's cell: The giant cell has a peripheral ring (horseshoe) of nuclei in the cytoplasm
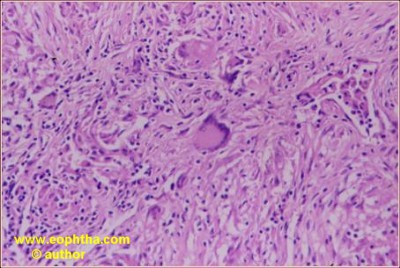
Fig: Langharn giant cells
Foreign body giant cell: The nuclei are centrally placed and overlap each other
Touton's cells:There is a ring of nuclei separating a peripheral clear cytoplasma from an eosinophilic central cytoplasm.
Common pathologies of eye:
Epidermal cyst:
Cyst like structure surrounded by keratinized stratified squamous epithelium. Lumen contains keratin like material. Sometimes foreignbody giant cells are seen
Dermoid cyst:
Cyst like structure surrounded by keratinized stratified squamous epithelium. Lumen may or may not contain keratin like material. The wall usually contains sebaceous glands, sweat glands, hairfollicles etc (structures from the dermis). This feature differentiates a dermoid cyst from an epidermal cyst
Squamous papilloma:
Stratified squamous epithelium shows hyperkeratosis and acanthosis with folds that surround a central fibrovascular core
Fig: squamous papilloma and hyperkeratosis
Chalazion:
Multiple inflammatory cells surrounding clear spaces (result of lipid removed by formalin during processing) with or without foreignbody giant cells
Molluscum contagiosum:
Stratified squamous epithelium shows acanthosis which grow into the dermis to form multiple lobules. Intracytoplasmic inclusion bodies which are eosinophilic at the base which becomes basophilic at the superficial layer are seen. There could be a central cater into which the inclusion bodies discharge their content.
Fig: Molluscum contagiosum
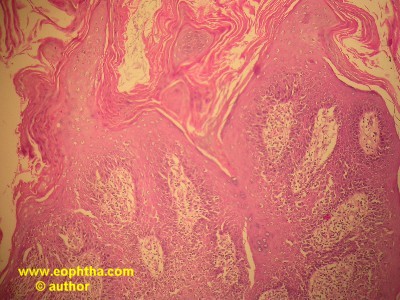
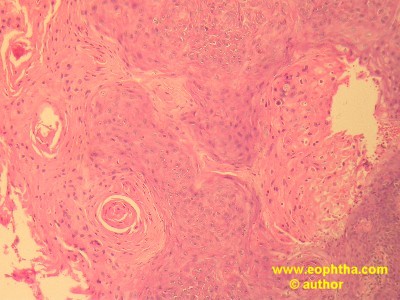
Squamous cell carcinoma:
Hyperplasia of the stratified squamous epithelium. Dysplasia seen. Presence of keratinisation within the cells. Intraepithelial keratin in the shape of a whorl termed as squamous eddies or pearl. The cells are pleomorphic with alteration in the nucleus-cytoplasmic ratio, hyperchromatic and in highpower intercellular bridges are commonly seen. There could be dermal invasion by abnormal cells from the epidermis.
Fig: squamous cell carcinoma and term dysplasia
Basal cell carcinoma:
The tumor cells arise from the basal layer of the epidermis and form dermal nests, cords and islands. These cells are basophilic. The periphery of the nests show a palisading pattern of cells. Mitosis is usually infrequent. Cracking artifact is seen between the lobules.
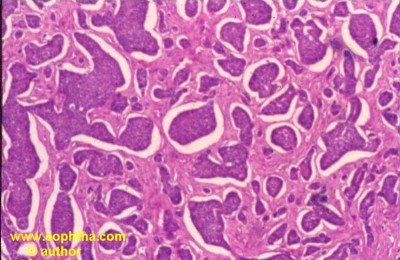
Fig: Basal Cell Carcinoma
Sebaceous cell carcinoma:
The tumor cells are arranged in the dermis in a lobular fashion. Some lobules may show central necrosis. The tumor cells appear vacuolated (due to fat in the cytoplasm removed by alcohol during processing). Mitosis very common. Oil red O and sudan black stain are used for confirmation on frozen sections.
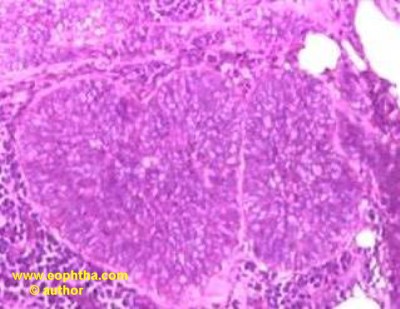
Fig: sebaceous cell carcinoma

Fig: sebaceous cell carcinoma-High magnification
Conjunctival Naevus:
Can be junctional (cells solely located between the epithelium and substantia propria), subepithelial naevus (cells entirely in the subepithelium) and compound naevus ( cells both in the epithelium and in the substantia propria)
Pigmented cells arranged in the form of nests. Loss of maturation is seen towards the base of the tumor. Cyst like spaces may be seen
Ptergygium:Conjunctival epithelium appears thinned out. Elastotic (basophilic) degeneration of the stroma seen in the substantia propria.

Fig: Histological photograph of pterygium
Keratoconus: Saw tooth appearance and disruption of bowman’s membrane. Scarring in the stroma and thinning of the central cornea. Ruptures in descemet’s membrane may be seen. Sometimes iron may be seen in the epithelium (Fleisher’s ring)
Fuchs endothelial dystrophy: Thickening of the descemets membrane with guttata in the endothelial layer (absent endothelial cells). Stromal edema and bullae in the epithelium may be seen. Bowman’s membrane fibrosis may be seen in chronic epithelial edema.
Fig: Fuchs endothelial dystrophy
Granular corneal dystrophy:Discrete red lesions seen in the corneal stroma in slides stained by masson trichrome
Lattice corneal dystrophy: Discrete lesions staining red with congo red are seen in the corneal stroma. These lesions show apple green birefringence and dichroism with polarized light
Macular corneal dystrophy: Diffuse lesions staining pink with PAS and blue with alcian blue are seen in the corneal stroma
Choroidal melanoma:
Pink tumor arising from the choroid
Gross examination would show a mushroom shaped mass with retinal detachment. Spindle A cells contain slender nuclei with delicate chromatin with no mitotic activity. They have a good prognosis. Spindle B cells contain plump nuclei with small but prominent nucleoli and coarse chromatin. Mitotic figures are common.
Epitheloid cells are larger and contain eosinophilic cytoplasm with oval shaped nuclei. The cells are larger and exhibit pleomorphism and increased mitotic activity. Chromatin appears coarse and mitotic figures are abundant. They have a poorer prognosis
Mixed type: Usually the histology reveals a mixture of spindle and epitheloid cells.
Vortex vein invasion is an important prognostic indicator in malignant melanoma
Retinoblastoma:
Basophilic round cell tumor arising from the retina. 3 types of rosettes can be seen:
Flexner wintersteiner rosettes: Clusters of basophilic round tumor cells arranged around a central lumen. Nuclei are displaced away from lumen. Specific for retinoblastoma
Homer Wright rosettes: radial arrangement of cells around a central tangle of fibrils. Not specific for retinoblastoma
Fleurettes: There is photoreceptor differentiation.
Other histopathological features:
-
Clumping of DNA around blood vessels
-
Necrosis and calcification
-
Optic nerve and extrascleral invasion are important prognostic markers.
How to send a specimen for histopathological examination?
One needs to send a clearly labeled specimen immersed completely in the appropriate fixative to the histopathological lab with the following information:
-
Identifying information (name, address, sex, age, physician’s name)
-
Precise location from which the material was obtained
-
A pertinent history (duration of lesion, visual acuity, information of previous surgery and review of previous pathology slides)
-
Clinical diagnosis (as it may alter the specimen handling in the laboratory)
-
Preoperative photographs may help the pathologist orient the lesion
-
If neoplasm , suspected, margins should be identified with different length or colour of sutures rather than painting the margins with dyes.
-
While handling conjunctival tissue, which has the tendency to curl, spread the conjunctiva onto a flat, absorbent surface such as the paper wrapping for gloves. Allow the conjunctival tissue to become adherent to the surface for approximately 20-30 seconds. When the tissue is adherent to its support, float the supporting surface and tissue onto formalin with the tissue surface facing up. Do not pin the specimen to a surface as the pins may rust and deposit iron on the specimen creating confusion. Also do not smear the specimen on a tongue depressor as it will not adhere to this surface easily.
-
A discussion with the pathologist prior to the surgery is often beneficial, so that the appropriate fixative, appropriate technique of transfer to the lab and a proper diagnostic technique is available for your patient’s specimen.
What are the fixatives used in the histopathology lab?
The commonly used tissue fixative is 10% neutral buffered formalin and this is satisfactory for most purposes in ophthalmic pathology. The recommended volume of tissue to fixative is 1:10. The tissue sample is submerged completely in the fixative and not adherent to the wall of the specimen jar well above the level of the solution. For fixing a globe, the entire eye should be at least covered by the solution. One should not inject the fixative into the eye or cut holes into the eye as these may cause artifacts. Immersion of the globe in formalin will permit good fixation within 48 hours.
However 10% neutral buffered formalin is not a universal fixative.
-
Some crystalline substances such as urate are soluble in formalin and hence has to be fixed and processed in a water free environment such as absolute alcohol.
-
Specimens for electron microscopy and those which have to be stored for a long time for future studies are preferably fixed in fresh 2% glutaraldehyde(Cidex). A filter paper may be put over the solution. The specimens in glutaraldehyde must be transported immediately to the laboratory.
-
Some pathologists prefer a mercury based fixative (B5) for lymphoid lesions
-
For Immunopathology techniques and for frozen sections, fresh tissues are required. They have to be shifted immediately to the pathology laboratory and should not be fixed in formalin
When in doubt, about the proper fixative type, consult the pathology laboratory before commencing the surgery.
What types of specimens received in ocular pathology lab?
They include Conjunctival tissues, corneal buttons, skin and lid biopsies, lacrimal gland and orbital lesions, iris, ciliary body and retinal tissues, enucleated globe and eviscerated intraocular contents, optic nerve lesions, cytology of ocular surface lesions (skin and conjunctiva), corneal scrapings and intraocular fluids. Fine needle aspiration biopsy of orbital and intraocular tumors and explanted intraocular lenses.
What are the routine stains used in histopathology lab?
The routine stains used in the histopathology lab are
-
Haematoxylin and Eosin (H & E)
-
Periodic acid-Schiff (PAS)
What are the special stains used in histopathology lab?
Special stains used in the lab include:
-
Those to detect specific substances
-
Those to detect micro-organisms
Special stains to detect specific substances include:
No |
Type of special stain |
Substance detected |
Colour of substance |
Indicated in |
|
1 |
Alcian blue |
Mucopolysaccharide |
Blue |
Macular dystrophy |
|
2 |
Colloidal iron |
Mucopolysaccharide |
Blue |
Macular dystrophy |
|
3 |
Masson Trichrome |
Hyaline material |
Red |
Granular dystrophy |
|
4 |
Congo red |
Amyloid |
Red |
Lattice dystrophy |
|
5 |
Van Gieson |
Elastic fibers |
Grey |
Elastic tissue |
|
6 |
Oil Red O |
Lipid |
Red |
Fat within the cells |
|
7 |
Alizarin Red |
Calcium |
Red |
Band keratopathy |
|
8 |
Von Kossa |
Calcium |
Black or brown black |
Band keratopathy |
|
9 |
Perl’s Prussian blue |
Iron |
Blue |
Iron in the epithelium in keratoconus & Iron Intraocular foreign body |
|
10 |
Fontana Masson |
Melanin and argentaffin cells |
Melanin pigments in malignant melanoma & |
What are the stains used to find micro-organisms?
|
Microbe |
Stain used |
Colour |
|
1 |
Bacteria |
|
|
|
2 |
Fungi |
|
|
|
3 |
Mycobacteria Nocardia |
|
Red Red |
|
4 |
Chlamydia |
|
Blue purple inclusion bodies |
|
5 |
Acanthamoeba |
|
|
What is the interpretation of H&E stain?
Haematoxylin is a basic dye and has an affinity to bind to acidic structures (like nuclei, ribosomes and rough endoplasmic reticulum) and stains them purplish blue. These structures are thus called basophilic
Eosin on the otherhand is an acidic eye and has an affinity to bind to basic structures (like cytoplasmic proteins) and stains them red or pink. These structures are thus called eosinophilic. In summary, H&E stains nuclei blue and cytoplasm pink or red.
What is the purpose of doing PAS stain?
This stain is versatile and has been used to stain many structures including glycogen, mucin, mucoprotein, glycoprotein, as well as fungi. PAS is useful for outlining tissue structures including basement membranes, capsules, blood vessels, etc. As it stains many structures, this can give rise to a high background. It is very sensitive, but specificity depends upon interpretation.
Interpretate the Ziehl-Neelsen Stain?
The Ziehl-Neelsen stain, also known as the acid-fast stain, was first described by Franz Ziehl and Friedrich Neelsen. It is used to identify acid-fast organisms, mainly Mycobacteria. Modifications of this stain can also be used to stain few other bacteria like Nocardia and brucella. The reagents used are Ziehl-Neelsen carbolfuchsin, acid alcohol and methylene blue.
Prinicple: The lipoid capsule of the acid fast organisms takes up carbolfuchsin and resists decolourisation with a dilute acid rinse. It is of such high molecular weight that successful penetration by the aqueous based staining solutions like methylene blue is prevented. The acid fast organisms stain red colour while non acid fast organisms stain blue colour
Interpretate the Alizarin Red Stain?
Alizarinis an organic compound that is historically important as a prominent dye. It is an anthraquinone originally derived from the root of the madder plant. Alizarin red is used to detect the presence of calcific deposition by cells of an osteogenic lineage. Alizarin red S combines with calcium ions in a chelation process to form bright red lake.
Interpretate the Grocott hexamine methenamine silver (GMS)stain?
This stain, often abbreviated as "GMS", is used to stain for fungi and forPneumocystis carinii. The cell walls of these organisms are stained, so the organisms are stained gray to black on a green background.
Interpretate the Grams stain?
Gram staining (or Gram's method) is an empirical method of differentiating bacterial species into two large groups (Gram-positive and Gram-negative) based on the chemical and physical properties of their cell walls.
Gram-positive bacteria have a thick mesh-like cell wall made of peptidoglycan (50-90% of cell wall), which stain purple and Gram-negative bacteria have a thinner layer (10% of cell wall), which stain pink.
Principle:There are four basic steps of the Gram stain, which include applying a primary stain (crystal violet) to a heat-fixed smear of a bacterial culture, followed by the addition of amordant(Gram's iodine), rapid decolorization with alcohol or acetone, andcounterstainingwith safranin or basic fuchsin.
Crystal violet (CV) dissociates in aqueous solutions into CV+ and chloride (Cl – ) ions. These ions penetrate through the cell wall and cell membrane of both Gram-positive and Gram-negative cells. The CV+ ion interacts with negatively charged components of bacterial cells and stains the cells purple. Iodine (I – or I3 – ) interacts with CV+ and forms large complexes of crystal violet and iodine (CV – I) within the inner and outer layers of the cell. When a decolorizer such as alcohol or acetone is added, it interacts with the lipids of the cell membrane, a gram-negative cell will lose its outer membrane and the peptidoglycan layer is left exposed. The CV – I complexes are washed from the Gram-negative cell along with the outer membrane. In contrast, a Gram-positive cell becomes dehydrated from an ethanol treatment. The large CV – I complexes become trapped within the Gram-positive cell due to the multilayered nature of its peptidoglycan. After decolorization, the Gram-positive cell remains purple and the Gram-negative cell loses its purple color. Counterstain, which is usually positively-charged safranin or basic fuchsin, is applied last to give decolorized Gram-negative bacteria a pink or red color.
Interpretation: Gram positive bacteria stain blue or black while Gram negative bacteria stain red or pink