Oculoplastic surgery, despite being a niche surgical branch, encompasses a variety of procedures involving the nasolacrimal apparatus, orbit and eyelids. Having evolved into a speciality only in the last 6-7 decades, it also includes fields such as trauma, oncology and oculofacial aesthetics, which make it fascinating as well as challenging1.
Just as in most ophthalmic sub-specialities, Oculoplastics has a steep learning curve for most of the surgical interventions and each case is vastly different from the next. Here are our Ten Pearls that should help the beginner Oculoplastics consultant, fellow or fellowship aspirant to hone their skills in a more systematic manner:
1. Documentation and history taking:
One of the most essential skills in an oculoplastic practice is uniform and accurate pre- and post-operative documentation. It is important from a legal as well as an academic standpoint, to take patient photographs as well as measurements of the specimen that have been obtained intraoperatively. It is necessary to have a good quality camera (and video camera for surgical videography) with appropriate light sources to obtain high-definition images. Good before and after photographs can help patients understand their disease process better as well as the surgical results2. Prior to documentation, it is essential to have the consent of the patient or caregivers so that the material may be used for academic purposes.

Taking a good history can help diagnose several conditions in the clinic as well as help in further management. A common example is that of smoking in thyroid eye disease. It is essential to advise patients with thyroid-related ophthalmopathy to quit smoking in order to prevent worsening and help in the regression of active disease.
2. Counselling skills and preoperative planning :
The next step to plan surgery is properly counselling the patient. This not only involves explaining the details of the procedure and the cost but every aspect of the pre- and post-operative factors and outcomes. Convincing a patient that particular surgery is necessary is easier when the patient feels the need for it or if they have already consulted elsewhere and have been advised the same. It is necessary to keep these factors in mind and gauge them as you converse with the patient. Judging the psyche of the patient is especially important in elective procedures such as blepharoplasties and filler injections. It may be best to avoid such procedures in highly demanding or anxious clients. Explaining post-operative outcomes and giving the patient realistic expectations is a huge part of oculoplastic surgery. In a ptosis surgery, explaining lagophthalmos, asymmetry in down-gaze and lid fold is crucial to avoid an unhappy patient post-operatively. It helps to pictorially describe these situations in order for the patient to be very clear and reassured after surgery. More importantly, prior to orbit surgery, providing information on the possibility of vision loss and motility restriction is necessary. These particulars should be clearly mentioned in the consent form that is tailored based on the type of surgery.

Planning the procedure in the operation theatre should be done in a sitting position as far as possible, especially in ptosis surgery and blepharoplasty, as this takes into account the effect of gravity and helps give better post-operative results.
3. Thorough Knowledge of Anatomy and Allied structures:
The first and foremost requirement before embarking on a surgical journey in Oculoplastics is to have an in-depth picture of the anatomical landmarks and vital structures that may be encountered in each procedure. For example, in orbital floor fracture repairs and lower lid blepharoplasty, the inferior oblique is a structure that one commonly encounters and should not be severed to the extent possible3,4. Having an idea of the surface marking of important neurovascular bundles can help prevent paresis, hypoaesthesia and unforeseen haemorrhage and hematomas. Another example is that of the boundaries of the dacryocystorhinostomy ostium. Knowing the endpoints and extent help the surgeon decide at which point the osteotomy can be deemed adequate. This mental picture of the anatomy while operating helps the surgeon to stretch their boundaries and give the best possible results.

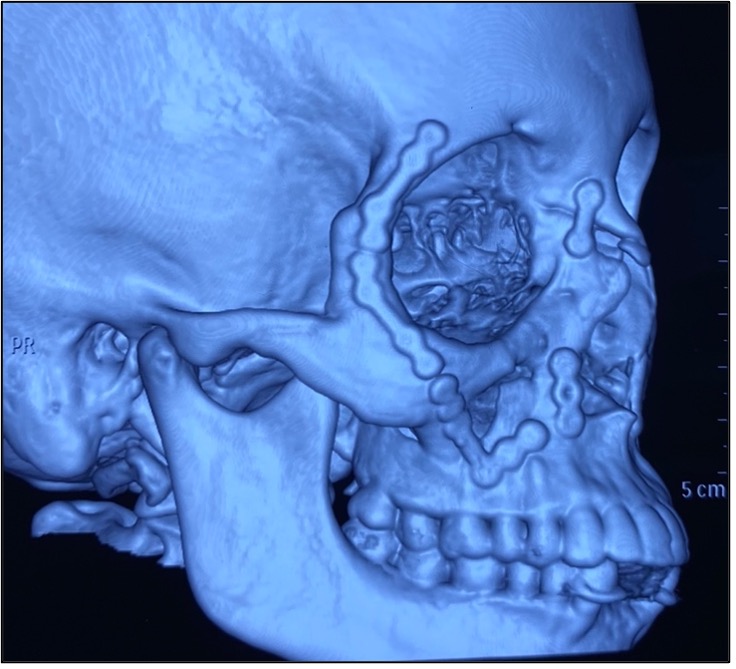
4. Ability to interpret imaging:
Deciding whether or not to plan surgery for a patient is largely dependent on the surgeon’s interpretation of the imaging findings. Oculoplastic surgeons heavily rely on MRIs and CT scans routinely. Other investigations such as MR Angiography and MR Venography are indicated in certain vascular conditions. 5 Dacryocystography and dacryoscintigraphy have been used to diagnose certain nasolacrimal conditions. CT scans with contrast, bone windows along with 3D reconstructions are almost always enough to diagnose most basic traumatic and neoplastic conditions. Asking for the right cuts (axial, coronal, sagittal) and imaging the right areas (eg. Including the brain or sinuses) is of utmost importance to diagnose and plan appropriate treatment.
5. Tissue handling:
While opening and repairing surgical incisions or traumatic wounds, it is important to dissect meticulously to prevent the creation of unsightly wounds or eyelid retraction. It is necessary to have a good hold on sutures and suturing techniques as well, in order to give the most aesthetic incision closures and outcomes. Starting from making an adequately sized incision to give the best exposure, putting traction sutures when and wherever necessary, to knowing which instrument is best in any given situation is also a part of handling the tissue appropriately. The periocular tissues have unique anatomy and it is important that we respect every aspect of it6.

6. Mastering the use of instruments and proper anaesthesia:
The first and foremost step to operating skilfully is knowing how to handle each and every instrument in your armamentarium. This includes the use of surgical loupes with a headlight, as most oculoplastic surgeons have reported that it improves patient care and learning how to use it needs to be incorporated into the residency7. Learning how to position ones chair, table and microscope/loupe is also important from the point of view of ergonomics. Improper balancing of these angles can result in cervical and lumbar issues which can prove detrimental in the long term.
Equally important is deciding what type of anaesthesia is required in a particular condition. This is decided based on the age of the patient, surgery to be performed and whether bone removal procedures are planned or not. For example, if a patient needs excision of an eyelid cyst, local anaesthesia is sufficient, however, if the patient needs a dacryocystorhinostomy, they would do better with sedation along with local anaesthetic infiltration. Patients who have been planned for orbital decompression or orbitotomies requiring the manipulation of the bone are best operated on under general anaesthesia. In certain procedures such as levator surgeries under local anaesthesia or orbital tumour excisions, it is important to infiltrate just the right amount of anaesthesia so as to not cut off the motor function of the levator muscle and not dilate the pupil, as these need to be assessed intraoperatively.
7. Harvesting flaps and grafts:
This is one of the most commonly encountered situations in an oculoplastic surgeon’s career as many procedures require certain flaps and grafts to restore function and fill defects. These include lid reconstructions such as the Cutler-Beard, Hughes tarsoconjunctival advancement, Tenzel flap, periosteal flap and full-thickness skin grafts most commonly from the retroauricular region based on the percentage of the defect left behind after resection of tumor with safe margins. Grafts for ocular surface and eyelid related conditions include mucous membrane and hard palate grafts. Fascia lata grafts are used for mainly bilateral congenital ptosis surgery, especially in blepharophimosis. Each graft or flap is different and needs to be handled as per its unique specifications. It is important to note that combining two grafts to fill a defect is not possible, however, an advancement flap can be interposed between two free grafts8.

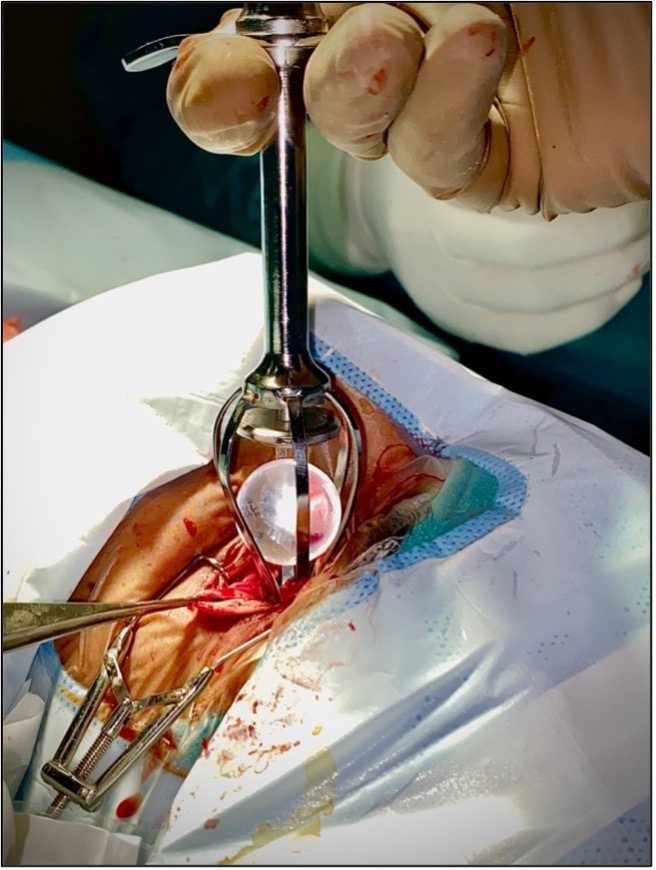
8. Step-by-step approach to orbital surgeries:
During fellowship training, one of the toughest scenarios encountered is orbital surgery. It is also one of the most difficult procedures to teach. For this, the best way for a resident to learn is by having a step-by-step approach to the surgery. Starting from planning the right anatomical approach based on imaging, giving the correct incision, learning how to dissect down to the extraconal or intraconal region, handling the periosteum, cutting bone with a chisel and hammer or a pneumatic drill, teasing out the tumor with dissection or a cryo probe and finally achieving good hemostasis and closing, these are all to be learned one at a time by assisting multiple procedures. Residents must keep a log of the procedure they performed on that day and focus on the next step to be done in another case. This pragmatic approach goes a long way in completing ones surgical training before performing cases solo.

9. Managing complications and asking for help:
Complications are a part and parcel of every surgeon’s career and it is imperative that one knows when to ask for help. It is not possible to be able to manage all complications by oneself in the early stages of one’s surgical career. Thus, when a complication arises or when a complicated case comes your way that is out of your scope, the best way to handle it is by referring to a more senior person or ask a senior to assist you. In oculoplastic surgery, complications are most commonly encountered post-operatively rather than intra-operatively and one always has time to plan and decide on the best possible course for the patient. This is one of the key steps in becoming a safe and sound practitioner.

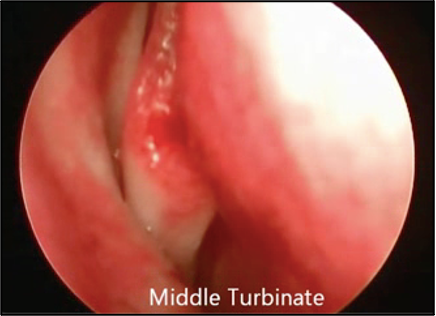
10. Learning from other specialties:
Being a relatively new field, Oculoplastics borrows from several other specialties such as Plastic Surgery, Otorhinolaryngology, Surgical Oncology, Maxillofacial surgery and Dermatology. When possible, it is best to involve a colleague from a related sub-speciality when planning a procedure that is out of the scope of our knowledge. In probing-intubations and endoscopic endonasal DCR surgeries, it is best to learn from an ENT surgeon how to perform a good endoscopy and identify structures correctly. One may even go so far as to learn how to perform a septoplasty if needed prior to DCR9.
There are multiple fellowship programs offered in Oculoplastics across the country, however, they are limited in comparison to anterior segment and posterior segment fellowships. It is important to select and apply for the right one based on the fellowship preceptors and faculty mentors who would best fulfil your needs as per your plans for future practice10.
Reference:
1. Saleh GM, Athanasiadis I, Collin JRO. Training and Oculoplastics: Past, Present and Future. Orbit. 2013;32(2):111-116. doi:10.3109/01676830.2013.764448
2. Nair AG. The Role of Photography in Oculofacial Aesthetics. In: Gupta A, Tahiliani P, eds. Orbit and Oculoplastics. Current Practices in Ophthalmology. Springer Singapore; 2019:1-9. doi:10.1007/978-981-13-8538-4_1
3. Mehta S, Belliveau MJ, Oestreicher JH. Oculoplastic Surgery. Clinics in Plastic Surgery. 2013;40(4):631-651. doi:10.1016/j.cps.2013.08.005
4. Tooley AA, Levine B, Godfrey KJ, Lisman RD, Tran AQ, Sherman JE. Inferior Oblique Entrapment After Orbital Fracture With Transection and Repair. Craniomaxillofacial Trauma & Reconstruction. 2020;13(3):211-214. doi:10.1177/1943387520928652
5. Cetinkaya A. Update on imaging techniques in oculoplastics. Saudi Journal of Ophthalmology. 2012;26(4):357-364. doi:10.1016/j.sjopt.2012.08.005
6. &Na; Manual of Oculoplastic Surgery, Fourth Edition: Plastic and Reconstructive Surgery. 2011;128(3):805-806. doi:10.1097/PRS.0b013e318225c826
7. Wei C, Wu AY. Surgical loupe usage among oculoplastic surgeons in North America. Canadian Journal of Ophthalmology. 2018;53(2):139-144. doi:10.1016/j.jcjo.2017.08.011
8. Hayano SM, Whipple KM, Korn BS, Kikkawa DO. Principles of Periocular Reconstruction following Excision of Cutaneous Malignancy. Journal of Skin Cancer. 2012;2012:1-6. doi:10.1155/2012/438502
9. Kamal S, Ali M, Nair A. Outcomes of endoscopic dacryocystorhinostomy: Experience of a fellowship trainee at a tertiary care center. Indian J Ophthalmol. 2016;64(9):648. doi:10.4103/0301-4738.194340
10. Meyer DR, Dewan MA. Fellowship Selection Criteria in Ophthalmic Plastic and Reconstructive Surgery. Ophthalmic Plastic & Reconstructive Surgery. 2010;26(5):357-359. doi:10.1097/IOP.0b013e3181c9fe14

