1. Epidemiology of Intraocular Lymphoma:
Intraocular Lymphoma is a rare malignancy accounting for 0.01% of ophthalmic conditions. The term includes primary intraocular lymphoma (PIOL) with or without primary central nervous system lymphoma (PCNSL). 1 Majority of the patients with lymphoma are over 50 years of age. 2
2. Presentations and Potential for Misdiagnosis of Intraocular Lymphoma:
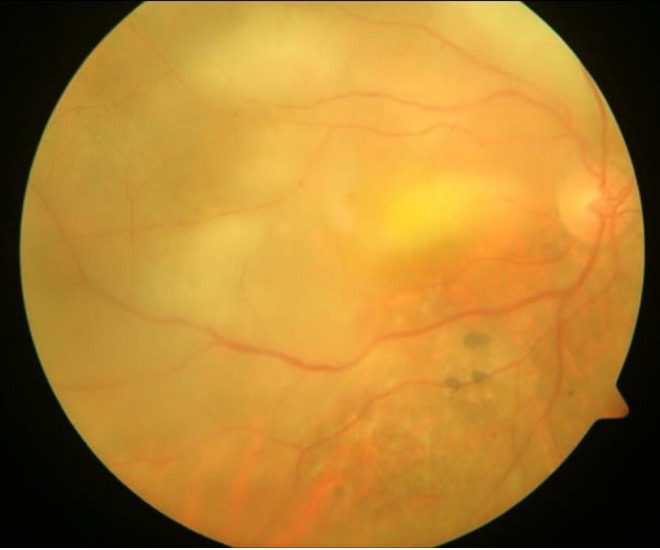
PIOL has varied presentations; but most commonly, it masquerades as intermediate and/or posterior uveitis; seen mostly as subretinal yellowish creamy lesions with an associated leopard skin type of retinal hyperpigmentation (Figure 1). 3
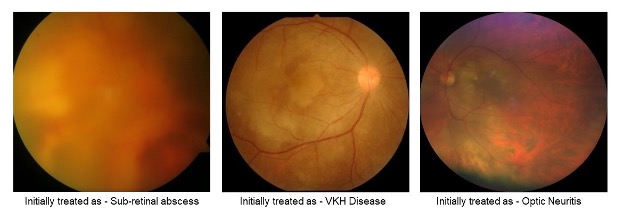
It usually originates from vitreoretina, thus known as primary vitreoretinal lymphoma (PVRL) or from uveal tissue and also the optic nerve. 4 In our experience it has masqueraded and been initially treated as “Tubercular sub-retinal abscess”, “VKH disease”, “Optic neuritis” and “Viral retinitis” 5 (Figure 2). Other researchers have reported patients with masquerading presentations for more than 2 years. 6,7
3. Laterality of Primary Ocular Disease:
PIOL is known to begin as monocular disease, with more than half of the patients progressing to binocular disease. This progression to the other eye is likely to be due to the destruction of blood-eye barrier. It occurs mainly in the elderly; who may have a weakened immune system and mutation accumulation. 4
4. Role of the ophthalmologist – using the eye as a window to the brain:
The disease when untreated is lethal; necessitating rapid and accurate diagnosis to increase survival, by diagnosing the disease prior to central nervous system (CNS) involvement. 1,3 This gives the ophthalmologist the responsibility to use the eye as a window to the brain or the body and suspect / diagnose disease prior to its spread. While giving a diagnosis of intraocular lymphoma, it is important to specify whether CNS is involved, as such involvement worsens the prognosis.
5. Symptoms and Signs of Intraocular Lymphoma – What not to Miss:
The leading three symptoms of PIOL patients are blurred vision, decreased vision acuity and floaters; the most common signs are vitreous opacities, fine keratic precipitates and retinal or subretinal infiltration. These are due to aggressive destruction of the retinal photosensitive structure by invading lymphoma cells. PIOL can also present as stellate keratic precipitates. 8
6. Retinal imaging for intraocular lymphoma – how does it help:
In Ocular Coherence Tomogram (OCT) scans, hyper-reflective foci in posterior vitreous, combined with retinal hyperreflectivity, subretinal lesions and intra-RPE lesions, representing the functional abnormality and structural interruption caused by the infiltration of lymphoma cells in different layers of the retina are seen. 9 OCT is thus a non-invasive method to document progress of PIOL once diagnosis is made and the patient is on treatment. 9 In a Fundus Fluorescein Angiogram (FFA); FFA/FAF reverse, defined as high autofluorescence spot on Fundus Autofluorescence (FAF) corresponding to a low autofluorescence spot without leakage in this region on FFA is described as the most frequent finding. 8
7. Lymphomatosis Cerebri – An atypical radiological sign of CNS lymphoma:
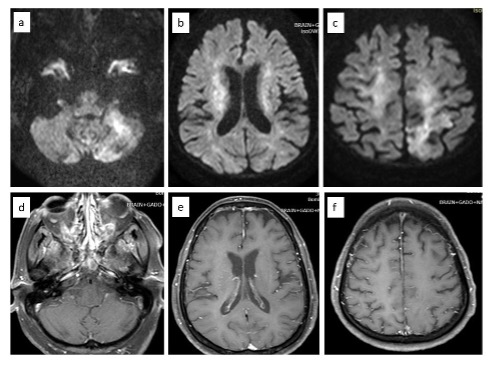
PCNSL may present as diffuse, nonenhancing infiltrative lesions. This rare variant is termed lymphomatosis cerebri (LC). LC (Figure 3) is a misdiagnosed entity associated with a diagnostic delay. MRI with of bilateral hemispheric involvement and CSF pleocytosis should alert a clinician of this diagnosis. 10
8. Challenges in Diagnosis of Intraocular Lymphoma by Vitreous Biopsy:
Diagnosis of PIOL can be best established by cytologic examination of the vitreous specimen through vitreous biopsy. 2 However as seen in our series 5, vitreous biopsy may be negative on multiple occasions because the lymphoma cells are fragile and easily degenerate in the vitreous. While observing lymphoma cells in cytological examination directly is still the gold standard with the highest specificity; the sensitivity is only around 80%. 8 Hence, multiple biopsies from different sites may at times be needed. 7 The analysis of MYD88 L265P mutation in the vitreous is reliable and efficient in the diagnosis of PIOL. 11
9. Analysis of the Aqueous Humor to the Rescue:
Aqueous humor tests come to our rescue due to minimal trauma and valid positive rate compared to vitreous fluid. The most promising test on the aqueous specimen is IL10/IL6 ratio >1 with a positive rate near 98% in PIOL patients. The positive rate of IL10>50pg/ml is also as high as 94%. 12 IL10 is expressed by malignant tumor cells, inhibiting various immune-related cell populations to achieve immune escape, while the rise of IL6 occurred in inflammation indicated stronger immune response. Thus, the levels of IL10 and IL6 have a great potential to distinguish PIOL from uveitis. This has led some authors to suggest that for patients with clinical manifestations and imaging characteristics supporting PIOL, the aqueous humor test should be the first choice for confirming the diagnosis and a diagnostic PPV should be reserved for later. 8
10. Treatment of intraocular lymphoma - Ophthalmologist in sync with an Oncologist:
The treatment is local therapy which can be radiotherapy to the eye or intracameral / intravitreal agents like (methotrexate and rituximab) or as systemic therapy which can be external beam radiotherapy or systemic chemotherapy. In unilateral cases, intravitreal methotrexate has been used in the dosage of 400 µg/0.1cc twice weekly for 4 weeks, followed by 1 weekly for 4 weeks, followed by 1 monthly for 12 months. It is used as a primary therapy as an alternative to radiotherapy or for cases of relapse. 13 Clinical remission is found to be achieved after mean of 6.4 +/- 3.4 injections. 14 Intravitreal rituximab is used in the dosage of 1mg /0.1 ml in cases which are unresponsive or cannot tolerate methotrexate. 15 In cases of systemic involvement or CNS lymphoma, systemic chemotherapy needs to be resorted to in conjunction with an oncologist.
The eye indeed is a window to the brain or the body for an ophthalmologist to suspect / diagnose intraocular lymphoma; a disorder masquerading as intraocular inflammation; prior to its CNS spread. All clinicians should recognize and inform their patients that PIOL can occur and manifest as PCNSL; even when the multiple vitreous biopsies and CSF analysis shows negative cytology. 5, 7, 8
References:
- Chan C-C, Buggage RR, Nussenblatt RB. Intraocular lymphoma. Curr Opin Ophthalmol 2002;13(6):411–8.
- Sen HN, Bodaghi B, Le Hoang P, Nussenblatt R. Primary Intraocular Lymphoma: Diagnosis and Differential Diagnosis. Ocul Immunol Inflamm 2009;17(3):133–41.
- Davis JL. Intraocular lymphoma: a clinical perspective. Eye Lond Engl 2013;27(2):153–62.
- Touhami S, Audo I, Terrada C, Gaudric A, LeHoang P, Touitou V, et al. Neoplasia and Intraocular Inflammation: From Masquerade Syndromes to Immunotherapy-Induced Uveitis. Prog Retin Eye Res (2019) 72:100761.
- Moreker MR, Patel RB, Khadilkar SV, Jaggi S, Dudani A, Patel K, Pardasani V. Intraocular Lymphoma - Lessons Learned by an Ophthalmologist. Bombay Hosp J 2022;64(2):1-5.
- Coupland SE, Bechrakis NE, Anastassiou G, Foerster AM, Heiligenhaus A, Pleyer U, et al. Evaluation of Vitrectomy Specimens and Chorioretinal Biopsies in the Diagnosis of Primary Intraocular Lymphoma in Patients with Masquerade Syndrome. Graefes Arch Clin Exp Ophthalmol (2003) 241 (10):860–70.
- Dutta Majumder P, Moreker MR, Khadilkar SV, Bhosale B, Khetan V. A case of non-Hodgkin lymphoma diagnosed after 35-month of initial presentation as recurrent vitritis with multiple negative biopsies. Oman J Ophthalmol 2022;15:212-4.
- Zhao XY, Cheng TT, Meng LH, Zhang WF, Chen YX. Clinical Features, Diagnosis, Management and Prognosis of Primary Intraocular Lymphoma. Front Oncol. 2022 Feb 3;12:808511.
- Zhao H, Wang X, Mao Y, Peng X. Longitudinal Observation of OCT Imaging is a Valuable Tool to Monitor Primary Vitreoretinal Lymphoma Treated with Intravitreal Injections of Methotrexate. BMC Ophthalmol (2020) 20 (1):10.
- Izquierdo C, Velasco R, Vidal N, Sánchez JJ, Argyriou AA, Besora S, Graus F, Bruna J. Lymphomatosis cerebri: a rare form of primary central nervous system lymphoma. Analysis of 7 cases and systematic review of the literature. Neuro Oncol. 2016 May;18(5):707-15.
- Narasimhan, S., Joshi, M., Parameswaran, S., Rishi, P., Khetan, V., Ganesan, S., Biswas, J., Sundaram, N., Sreenivasan, J., Verma, S., Krishnamurthy, V., & Subramanian, K. (2020). MYD88 L265P mutation in intraocular lymphoma: A potential diagnostic marker. Indian journal of ophthalmology, 68(10).
- Cassoux N, Giron A, Bodaghi B, Tran TH, Baudet S, Davy F, et al. IL-10 Measurement in Aqueous Humor for Screening Patients with Suspicion of Primary Intraocular Lymphoma. Invest Ophthalmol Vis Sci (2007) 48 (7):3253–9.
- De Smet MD, Vancs VS, Kohler D et al. Intravitreal chemotherapy for the treatment of recurrent intraocular lymphoma. Br J Ophthalmol 83: 448-451.
- Frenkel S, Hendler K, Siegal T et al. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10years of experience . Br J Ophthalmol 92: 383-388.
- Venkatesh R, Bavaharan B, Mahendradas P, Yadav NK. Primary vitreoretinal lymphoma: prevalence, impact, and management challenges. Clin Ophthalmol. 2019 Feb 14;13:353-364.


