History of Present Illness:
A 60-year old male patient presented with recurrent episodes of watering and foreign body sensation of both eyes for 8 years. He gave no history of redness or discharge from the eyes. There was no history of spontaneous eversion of the eyelids. He was treated conservatively with lubricants but had no relief of symptoms. He complained of snoring during sleep with associated daytime somnolence.
Past Ocular History:
No history of ocular trauma or surgery in the past.
Past Medical History/ History of Medication:
He was diagnosed with Rheumatoid arthritis 1.5 years ago and hypertension for which he is on treatment.
Family History:
No significant family history
Review of Systems/Systemic Examination:
Systemic examination was within normal limits. All vitals were within normal limits.
OCULAR EXAMINATION
Best Corrected Visual Acuity (Snellen)
Right eye (OD): 6/6P, N6
Left eye (OS): 6/6, N6
Ocular Motility/Alignment: Hirshberg corneal reflex- Orthophoric, EOM-Full, free and painless in all gazes
Intraocular Pressure (Applanation tonometry)
OD: 17 mm HgOS: 17 mm Hg
Pupils: OU: Round regular and reacting to light
Confrontation visual fields: full
External examination (Fig 1):
|
OD |
OS |
|
|
Lids/Lashes |
Lash Ptosis+ |
Lash Ptosis+ |
|
Brow Ptosis |
Present |
Present |
|
Frontalis Overaction |
Present |
Present |
|
Dermatochalasis |
Present |
Present |
|
Lower Lid Fat Prolapse |
Present |
Present |
|
Lid Laxity Test: |
||
|
Lid Distraction |
Present |
Present |
|
Snap Back Test |
Poor |
Poor |
|
Horizontal Lid Laxity |
Present |
Present |
|
Medial Canthal Tendon Laxity |
Present |
Present |
|
Lateral Canthal Tendon Laxity |
Present |
Present |
|
Lacrimal Gland Prolapse |
Present |
Absent |
Slit Lamp Examination
|
Conjunctiva |
Papillae+ |
Papillae+ |
|
Cornea |
Diffuse SPK |
No SPK |
|
Iris |
Normal |
Normal |
|
AC |
VH 4, Quiet |
VH4, Quiet |
|
Lens |
NS2 |
NS2 |
Dilated Fundus examination
|
Vitreous |
Normal |
Normal |
|
Disc |
Normal |
Normal |
|
Macula |
Normal |
Normal |
|
Vessels |
Normal |
Normal |
|
Periphery |
Normal |
Normal |
Ancillary Investigations:
Sleep study:
- Frequent episodes of snoring, apnoea, and hypopnea were noted with associated minimal oxygen desaturation
- Apnoea Hypopnea Index (AHI):27.2
He was diagnosed to have moderate sleep apnoea by the sleep disorder specialist. He was advised sleep hygiene measures, weight loss and continuous positive airway pressure (CPAP)
Dry eye workup:
Tear meniscal height (TMH) OU decreased
Schirmer’s test: OU-25mm
Tear breakup time (TBUT): OD-10 sec, OS- 8 sec
Differential Diagnosis:
1. Involutional ptosis
2. Involutional entropion
Diagnosis:
Floppy eyelid syndrome
Clinical Course of the condition:
The patient underwent right eye upper eyelid entropion correction (anterior lamellar repositioning) with horizontal lid shortening (Lateral Tarsal Strip) under local anesthesia. Post the procedure the mild entropion and lash ptosis was well corrected. He was symptomatically better and was following the treatment as advised by the sleep specialist.
DISCUSSION
Floppy eyelid syndrome (FES) is an acquired degenerative condition of the tarsal plates. It was first described by Culbertson and Ostler in 1981. The classical feature of FES is the presence of very elastic, lax, rubbery, and easily eversible upper eyelids on mild traction. Eversion of the eyelids with chafing against the pillow during sleep results in chronic papillary conjunctivitis and punctuate keratopathy in these patients. The symptoms are lateralized to the preferential sleeping side of the patient or tend to be bilateral in patients who sleep face down with their lids everted against the pillow.
Typically described in obese, middle-aged men, the other common clinical findings include blepharoptosis, meibomian gland dysfunction, entropion, lash ptosis, and superficial punctate keratitis. A strong association has been reported to exist between FES and Obstructive Sleep Apnoea (OSA). OSA is a potentially fatal condition characterized by apnoea/hypopnoea spells during sleep, which, if untreated, can lead to life-threatening systemic complications.
Pathophysiology
The exact etiology and pathogenesis of FES has not been elucidated to date and the vast majority of histopathologic studies of eyelid biopsy specimens have shown nonspecific features of chronic inflammation and meibomian gland disorder. Netland et al were the first to report reduced elastin content of the tarsal plates as a possible etiological factor causing this enigmatic eyelid disorder. Various theories have been postulated; the most commonly accepted are those concerning mechanical injury and ischemia.
1. Mechanical injury caused by rubbing of the everted lids during sleep results in irritation and subsequent papillary inflammation. Constant eye rubbing worsens the inflammation setting up a vicious cycle.
2. Poor apposition of the lax lids to the globe results in tear fluid abnormalities and meibomian gland dysfunction.
3. Ischemic damage caused by systemic hypoxia and pressure-induced lid ischemia on eversion of eyelids followed by reperfusion oxidation injury leading to degenerative changes in the tarsus.
4. Genetic abnormalities in collagen and elastin content.
5. Recent studies have suggested that a decrease in tarsal elastin content, ultrastructural abnormalities in elastin, and increased production of elastin degrading enzymes such as matrix metalloproteinase (MMP) 2,7,9,12 and neutrophil elastase are responsible for the reduced tarsal elasticity and stability in FES.
Clinical Features
FES is most commonly seen in middle-aged men, however, it has also been reported in young men and women. The presenting features in FES are numerous and non-specific, the most common being watering, irritation, foreign body sensation, itching, droopy eyes, and mucous discharge on waking up. Some patients may complain of spontaneous lid eversion during sleep noticed on waking up.
Ocular features:
1. Eyelids and conjunctiva:
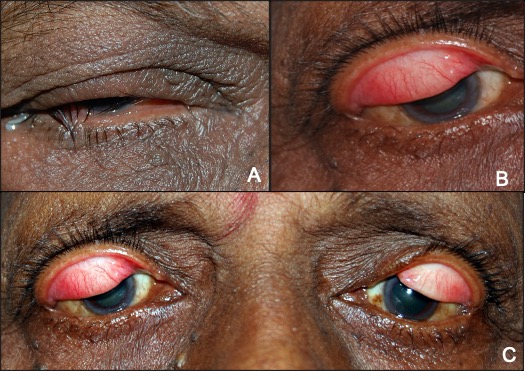
Increased laxity of the eyelids is a hallmark feature of FES. The tarsal plates are soft and can be folded upon themselves and demonstrate increased upward excursion on vertical traction. Blepharoptosis and dermatochalasis are common associations. Ptosis is most commonly aponeurotic, characterized by absent or increased upper eyelid crease height. Most patients with FES have an underlying meibomian gland dysfunction and tear fluid abnormality which worsens the ocular surface irritation. Recently, an increased incidence of upper eyelid lashes ptosis has been reported in patients with FES. Nocturnal eversion of the eyelids causes overriding of the pretarsal orbicularis oculi and skin over the lid margins and downward misdirection of the lashes. Another mechanism is purported to be the lack of support of lash follicles due to the abnormal tarsus. The presence of lash ptosis should alert the treating ophthalmologist to look for eyelid laxity. (Fig 2A)

A definitive feature seen universally in all patients of FES is chronic papillary conjunctivitis. The severity of conjunctivitis is directly proportional to the degree of eyelid laxity. (Fig 2B) Significant improvement has been demonstrated following eyelid tightening procedures.
2. Cornea:
The main corneal manifestation is punctate epithelial keratopathy. Prolonged nocturnal eversion, if untreated, can lead to chronic keratoconjunctivitis, corneal neovascularization, scarring, and recurrent corneal erosions. Severe cases can develop ulcerative keratitis and corneal perforations.
An association between FES and Keratoconus (KC) has also been established. Constant eye rubbing has been postulated to be the cause of KC as both FES and KC were found to be localized to the preferential sleeping side of the patient
Eyelid laxity can be documented by certain simple clinical tests.
Horizontal eyelid laxity (distraction test):
The lid is pulled away from the globe. Displacement of more than 10 mm is abnormal and confirms an increased horizontal laxity. (Fig 3 A and B)

Snap Back Test:
The lid is gently pulled away from the globe and the pace of returning to the normal position is observed.
Normal – snaps back immediately
Mild – slow return
Moderate – return to normal position with a blink
Severe – incomplete return even after a blink
Vertical lid pull:
Upward traction is applied to the pretarsal skin in the vertical direction. The normal excursion of the upper lid margin is 5 to 10 mm. Patients with floppy eyelid have an excursion of 15 to 25 mm. (Fig 3 C and D)
Lateral Canthal Tendon Laxity:
Normally the lateral canthus has an angular appearance. Rounding of the lateral canthus and medial displacement of lateral canthus more than 2 mm indicates laxity.
Ancillary Investigation
A consistent association of Obstructive Sleep Apnoea with Floppy Eyelid Syndrome has been reported. OSA patients can develop multiple episodes of apnoea/ hypopnea spells during sleep due to partial or complete collapse of the pharynx. The number of apnoea–hypopnea episodes per hour of sleep is calculated and called the Apnoea-hypopnea index (AHI). Obstructive sleep apnoea syndrome is present if AHI is greater than 5, with mild being 5 – 14, moderate 15 – 30, and severe > 30. The resultant sleep disturbance results in increased daytime somnolence, headache, and lethargy. Repetitive sympathetic activation due to arousal from sleep leads to cardiac arrhythmias and systemic hypertension. Early detection and treatment are critical due to the increased risk of pulmonary hypertension, cor – pulmonale, and cardiac arrhythmias associated with untreated cases.
Treatment
Medical:
Most patients can be managed conservatively.
- The use of lubricating eye drops during the day and lubricating gel at bedtime helps to stabilize the tear film.
- Nocturnal eye shields to protect the eyelids from rubbing against the pillow which helps to break the vicious cycle.
- Taping of the eyelids, topical steroids, lid hygiene measures to treat blepharitis, and punctal plugs to prevent dry eye are other effective methods of treatment.
- It is imperative to take a history of snoring, daytime somnolence, and lethargy and refer patients to a sleep disorder specialist if history is positive.
Surgical management:
Can be tried in patients unresponsive to medical management. Most procedures consist of horizontal lid shortening.
- Full-thickness wedge excision: This consists of excision of a full-thickness pentagon of the eyelid at the junction of medial two-thirds and lateral one thirds. It is a highly effective procedure. Studies have reported an improvement in conjunctival symptoms and improvement in ptosis following surgery.
- The lateral tarsal strip technique involves creating a periosteal flap to which the fashioned tarsal strip is sutured.
- Other procedures include medial and lateral canthal tendon plication, lateral tarsorrhaphy, and ptosis correction.
Floppy Eyelid Syndrome |
|
|
Etiology:
|
Signs
|
|
Clinical Features
|
Differentials
|
|
Investigations
|
Treatment
|
References:
1. Culbertson WW, Ostler HB. The floppy eyelid syndrome. Am J Ophthalmol. 1981; 92:568–75. 2. Ezra DG, Beaconsfield M, Collin R. Floppy Eyelid Syndrome: Stretching the Limits. SurvOphthalmol. 2010; 55:35–46. 3. Yeung AM, Ashfaq I, Ghosh YK, Kyprianou I, Ahluwalia HS. Floppy eyelid syndrome: the coventry experience. Orbit. 2014; 33:399–405. 4. Diaper CJM. Wake up to floppy eyelid syndrome. Br J Ophthalmol. 2013; 97:1363–4. 5. Schlotzerschrehardt U, Stojkovic M, Hofmannrummelt C, et al. The Pathogenesis of Floppy Eyelid SyndromeInvolvement of matrix metalloproteinases in elastic fiber degradation. Ophthalmology. 2005; 112:694–704. 6. Netland PA, Sugrue SP, Albert DM, Shore JW. Histopathologic features of the floppy eyelid syndrome. Involvement of tarsal elastin. Ophthalmology. 1994; 101:174–81. 7. Snell RS, Lemp MA. Clinical Anatomy of the Eye. Wiley; 1997. 436 p. 8. Yanoff M, Duker JS, Augsburger JJ. Ophthalmology. Elsevier Health Sciences; 2009. 1551 p. 9. McNab AA. Floppy eyelid syndrome and obstructive sleep apnea. Ophthal Plast Reconstr
Surg. 1997; 13:98–114. 10.Van den Bosch WA, Lemij HG. The lax eyelid syndrome. Br J Ophthalmol. 1994; 78:666–70. 11. Medel R, Alonso T, Vela JI, et al. Conjunctival cytology in floppy eyelid syndrome: objective assessment of the outcome of surgery. Br J Ophthalmol. 2009; 93:513–7. 12. Langford JD, Linberg JV. A new physical finding in floppy eyelid syndrome. Ophthalmology. 1998; 105:165–9. 13. Donnenfeld ED, Perry HD, Gibralter RP, et al. Keratoconus associated with floppy eyelidsyndrome. Ophthalmology. 1991; 98:1674–8. 14. Das A, Radhakrishnan A. Teaching NeuroImages: Floppy eyelids in obstructive sleep apnea syndrome. Neurology. 2011; 77:e130–1. 15. Ezra DG, Beaconsfield M, Sira M, Bunce C, et al. Long-term Outcomes of Surgical Approaches to the Treatment of Floppy Eyelid Syndrome. Ophthalmology. 2010; 117:839–46.

