Optical Coherence Tomography (OCT) is a quick, non-invasive, reproducible, and optical analog of ultrasound imaging which is as good as in vivo viewing of individual retinal layers histologically. In today’s practice, OCT is indisputably an essential diagnostic tool for every retinal surgeon. And so correct interpretation of OCT scans helps us in understanding the disease pathologically which in turn aids in prognosticating and making treatment decisions.
How to quickly read a macular OCT?
An OCT image gives you layer by layer information of retinal tissue. So if we segment the OCT image into 5 layer-wise sub-segments, it becomes very easy to read and interpret the retinal pathology. And also just by looking at the diseased/damaged retinal layer, we can identify probable clinical disease.
These5 OCT sub-segments can be used for quick interpretation of macular OCT scans.
1: VR (Vitreo-Retinal) Interface
2: Inner Retina
3: Outer retina
4: RPE/ BRUCHS MEMBRANE
5: Choroid
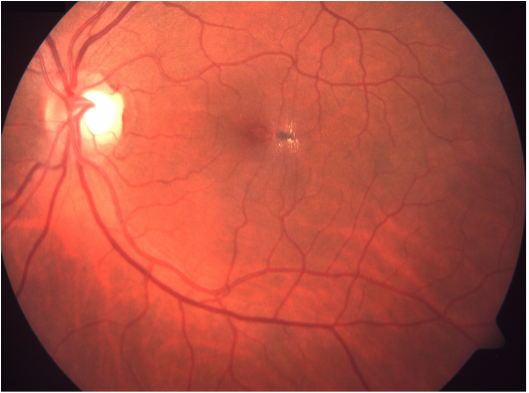
Let us first review the normal macular OCT.
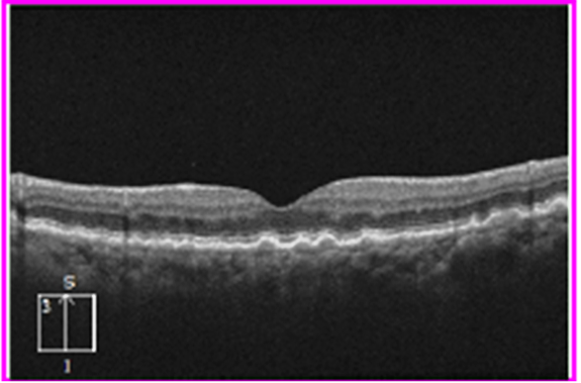
THIS IS HOW THE NORMAL MACULAR SCAN LOOKS LIKE.
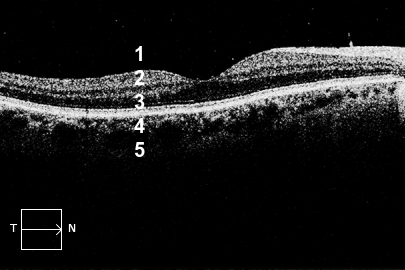
Henceforth in order to read and interpret a macular OCT scan rapidly, we must keep in mind the normal appearance of these 5 sub-segments.
A thumb rule before interpreting any OCT image is to be aware of the background clinical history and fundus photo of the same eye of which you are going to interpret the OCT image.
My personal advice would be to be a good clinician first i.e. examine the patients in detail, try interpreting the clinical fundus photos before you jump in to read and interpret the OCT scans. Always correlate your OCT interpretation or for that matter any diagnostic imaging to your clinical examination findings.
Now let's see some examples of abnormal macular OCTs of common retinal diseases and interpret them by sub-segmenting them.
1. Vitreoretinal Interface
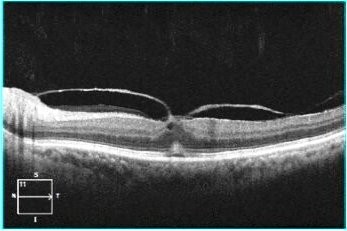
Here we can easily appreciate a hyper-reflective layer in the sub-segment number 1 which is attached at fovea viz. VR interface gives us a clue to the possible clinical diagnosis of vitreo-macular traction (VMT).
(P.S. there are some other subtle abnormalities in this OCT image of VMT like cystic changes in the inner retina and the neurosensory detachment in deeper layers which we will discuss once we go through each of the 5 sub-segments).
Let’s learn to read one more similar OCT image.
In this image, you can see a hyperreflective membrane in VR interface Sub-Segment which is exerting traction to the underneath retinal layers suggesting an Epiretinal membrane (ERM).
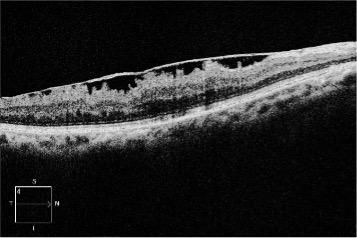
2. Inner Retina
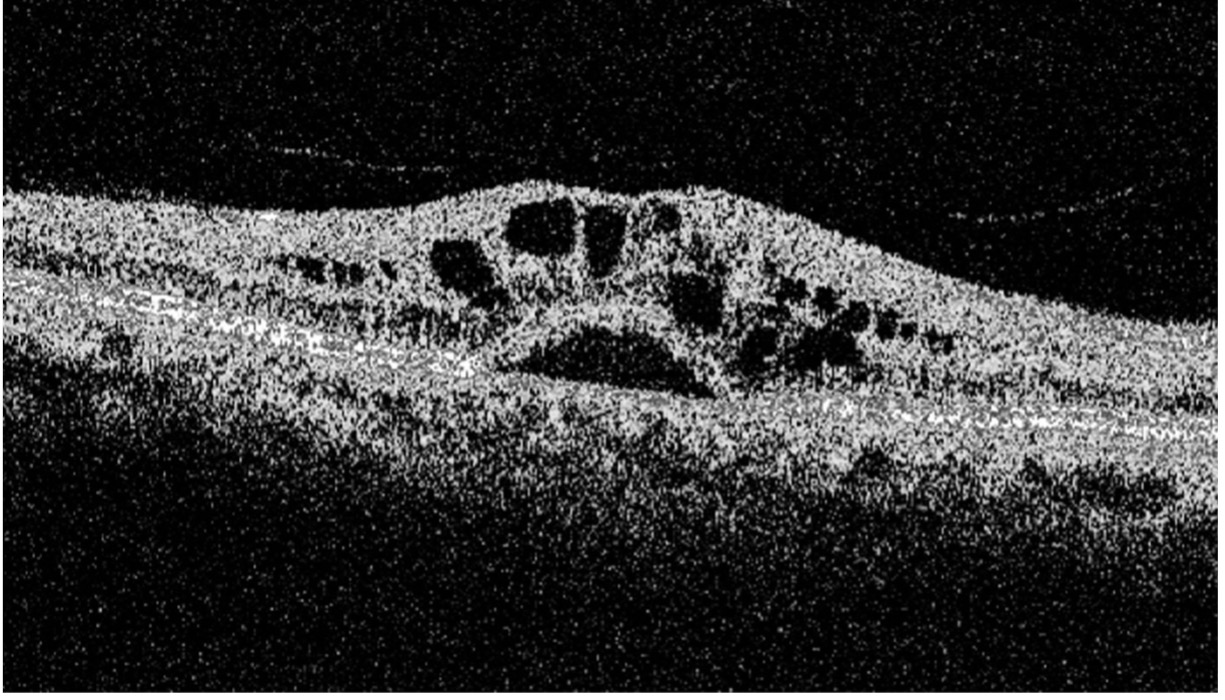
This OCT image shows hyporeflective cavitatory spaces in the inner retina (sub-segment number 2). The rest of the OCT image including the deeper layers of the retina is appearing normal.
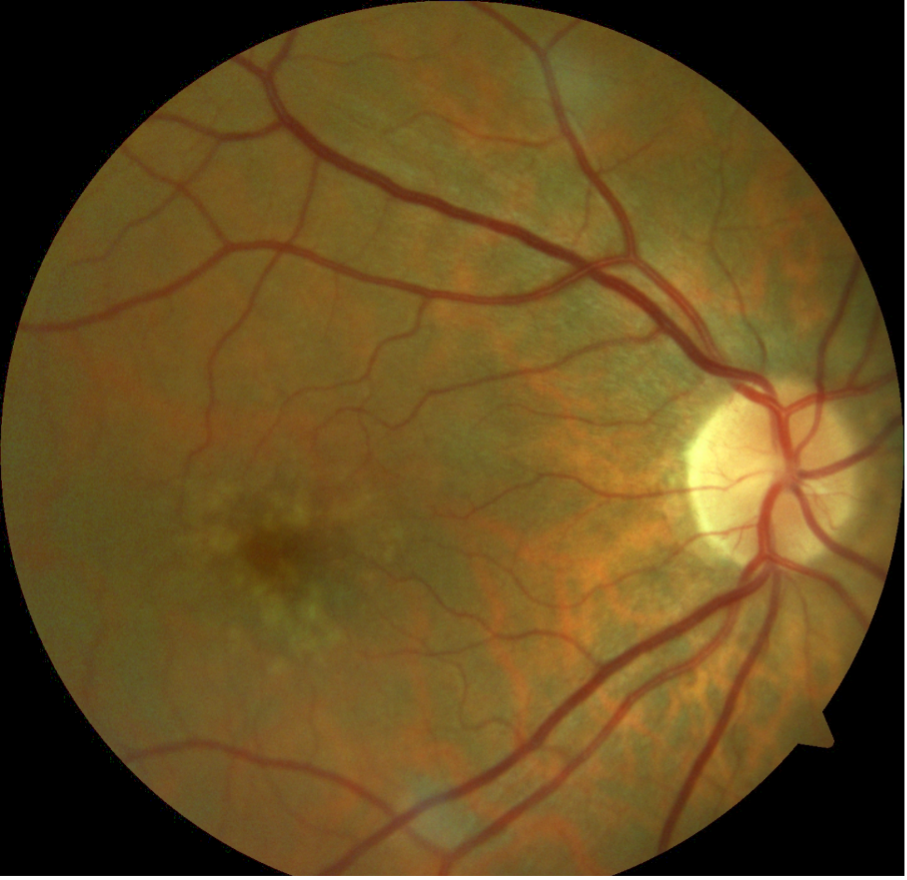
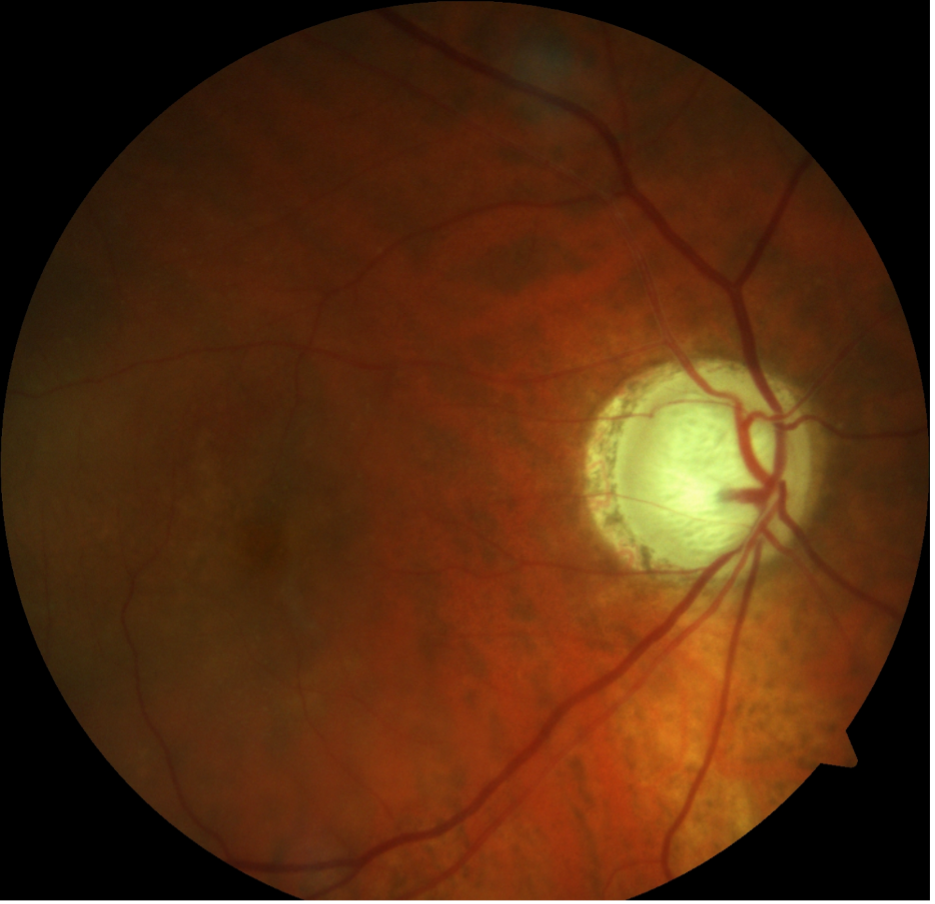
Before commenting on the diagnosis it is wise to retrospectively analyze the fundus photo of this eye.
This fundus picture is grossly showing pigmentary changes with yellow coloured deposits over temporal part of macula along with straitening of retinal vessels around it suggesting a possible clinical condition of macular telangiectasia type 2 (MACTEL).
3. Outer Retina
Here is an OCT image of a 61-year-old gentleman who underwent cataract surgery 3 weeks back.
Here we see multiple cystic spaces in the intraretinal architecture (Sub-Segment 3). Also, note the bump above the RPE line of the neurosensory detachment of retinal layers above RPE. This OCT image is a classic representation of Pseudophakic CME.
(Reminder always correlates clinical history also before making a diagnosis.)
Let's look at one more very common clinical case. Here is an OCT image of a 55-year-old patient with systemic diabetes and has been treated for diabetic retinopathy.
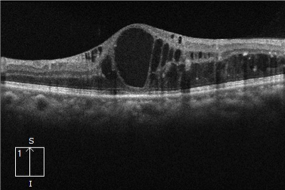
Here you can see gross hyporeflective cystic spaces throughout the retina (ie both inner retina and outer retinal layers sub-segments 2 & 3 are involved). Also, note the hyper-reflective aggregations and dots in the outer retina (sub-segment 3) representing hard exudates clinically.
Like I said earlier if we get acquainted with the clinical fundus image beforehand reading the OCT scans, it becomes simple to correlate the abnormalities on OCT scans and the diagnosis of the disease also becomes a simpler task.
Here is the clinical fundus image of the above patient.
The fundus image is a classic example of nonproliferative diabetic retinopathy with CSME. The ring of hard exudates is surrounding the fovea and the macular area is scattered with superficial and dot blot hemorrhages. Beyond macula, you can appreciate background retinopathy changes of microaneurysms, hemorrhages, and hard exudates suggesting moderate to severe grade of NPDR.
Now you will agree with me that reading OCT is far easy once you have the clinical fundus photo in the background. And additional information which we get on OCT is that CSME is involving the center of macula viz. Fovea. This small bit of information is very important to take a clinical decision of modality of treatment intravitreal injection or laser therapy.
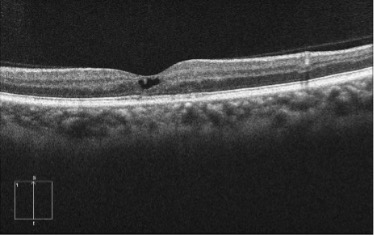
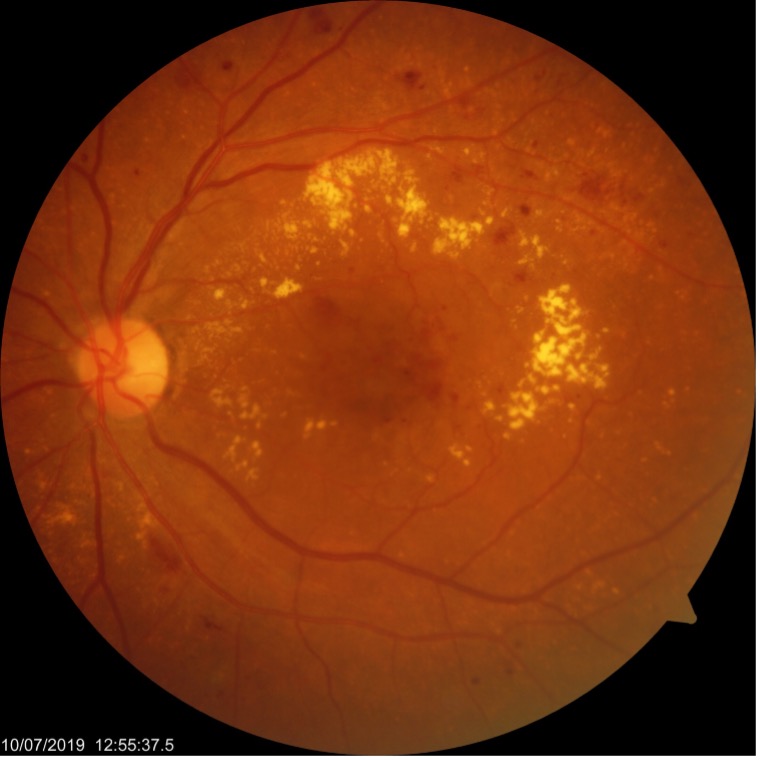
4: Retinal Pigment Epithelium
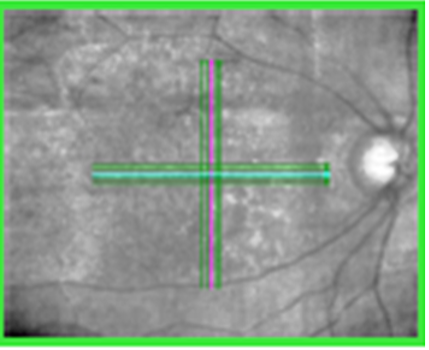
Normally the RPE layer is a straight line. Here you can notice bumpy or irregular RPE layer. These bumps have a high reflective border and moderate reflectivity internally suggesting solid deposits beneath the RPE. After clinical correlation, we come to a diagnosis of drusen suggesting Dry AMD. Below is the clinical fundus image of this same eye.
Sometimes when you don’t have a fundus image to co-relate, the OCT machine can also provide an infrared image of the posterior pole. Just by having a look at the OCT infrared image also you can get a clue of the clinical picture. The OCT infrared image appears like this. You can easily appreciate hyperluscent spots clinically correlating to drusen.
5. Choroid (Layer Underneath the RPE)
Let’s read and interpret this last OCT scan.
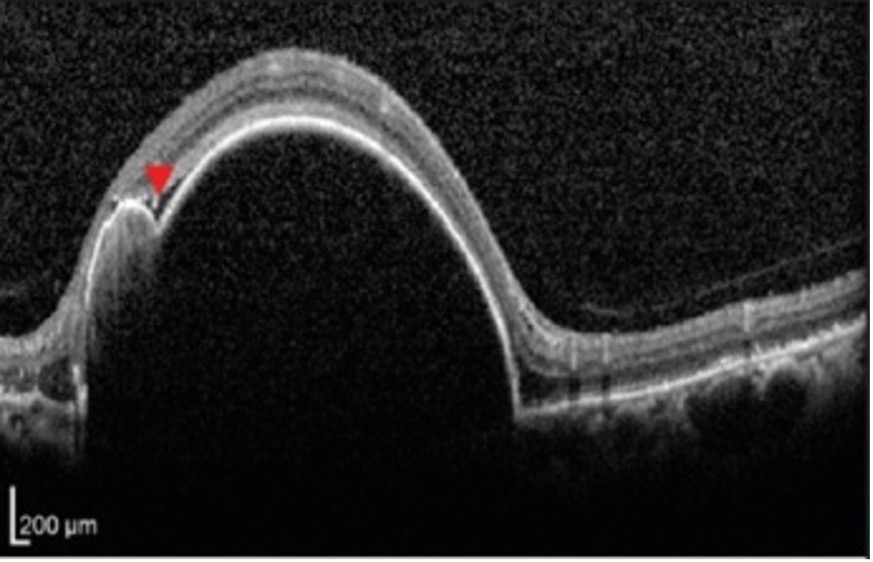
Here there is a gross elevation of RPE (hyper-reflective line bordering retina and choroid). And also note there is an irregularity in RPE elevation with a second bump (a notch) marked by an arrowhead. This tells us that the basic pathology is located below the retina viz choroid and by correlating this OCT image with the clinical fundus we interpret this huge bump to a notched ped and so we derive a differential diagnosis of PCV.
The last sub-segment choroid is better appreciated with newer generations of OCT machines with enhance depth imaging and swept-source technology.
In summary, whenever we read a macular OCT printout if we grossly lookout for these 5 sub-segments we can easily get a rough idea of probable clinical disease. I would like to end the summary of this write by repeating this important sentence again, “Whatever you see on an OCT image has to be correlated WITH clinical history and OTHER diagnostic IMAGING MODALITIES LIKE FUNDUS PHOTO, FLUORESCEIN ANGIOGRAMS OR INDOCYANIN ANGIOGRAMS WHICHEVER ARE AVAILABLE TO YOU before you draw your clinical diagnosis and treatment regimen”.
