Introduction
Rhegmatogenous retinal detachment (RRD) although rare, it is a serious ophthalmic condition that can lead to significant loss of vision or blindness without timely and appropriate management. It has been nearly a century (1918) since Jules Gonin demonstrated the importance of localizing and sealing retinal breaks, a procedure termed ignipuncture.1 Scleral buckling techniques, introduced by Custodis2 and refined by Schepens and later Robert Machemer’s pars plana vitrectomy, revolutionized repair of RRDs. Pneumatic retinopexy introduced in the mid 1980s allowed treatment of retinal detachments as an outpatient procedure in selected retinal detachments 3 Above techniques either alone or in combination has resulted in surgical success rates close to 90%.
For most surgeons, choice of surgical procedure for primary retinal detachment will depend on the individual clinical situation combined with each surgeon's experience; bias and comfort level with a particular procedure. Recent advances in surgical instrumentation, wide angle visualization, and the use of various intra-operative tamponade agents have made vitrectomy procedures safer and preferred treatment by the surgeons. There is less exposure to scleral buckling for vitreo-retinal surgeons in training and younger surgeons may ultimately prefer vitrectomy as a first choice for repair of retinal detachments. Scleral buckling however still has relevance to this day, but without a randomized clinical trial comparing the 3 modalities, and in various clinical scenarios, definitive answer as to which procedure is superior will be impossible.
Basic Rationale of repair of RRD
The regardless of the procedure chosen, the surgery aims to identify and close all the retinal breaks with minimum iatrogenic damage. Break closure in retinal detachment would involve two steps. First, is to bring the edges of the retinal break into contact with the underlying RPE which is achieved either by bringing the eye wall closer to the detached retina (a scleral buckle) or by pushing the detached retina toward the RPE (intraocular tamponade with a gas/PFCL(expand) bubble). The second step would be to create a strong chorio-retinal adhesion around the breaks; this may be accomplished with cryotherapy, laser photocoagulation or diathermy.

Figure 1a : High Myopia with Inferior RD

Figure 1b: High Myopia with Inferior RD
This review will try to find answers to some of the common situations in retinal detachment treatment
Asymptomatic retinal detachment
Management of asymptomatic retinal detachments usually identified on routine clinical examination range from conservative observation to prophylactic surgery. Vrabec et al, 4 Byer et al 5 and Cohen et al 6 suggest a conservative management. These authors recommend that asymptomatic RRDs in selected cases may be safely observed for many years with routine examinations and appropriate patient education on symptoms of retinal detachment. Vrabec et al4 demonstrated, demarcation laser photocoagulation of shallow, macula-sparing, RRD without associated PVR to be a reasonable alternative to surgical repair.
However, in a case series by Greven et al 7, asymptomatic RRD patients undergoing scleral buckle had good anatomic and functional results. They advocate that surgical management should be considered for asymptomatic RRD
Scleral Buckling:
Scleral buckles usually are made of solid silicone and silicone sponges. They can either be used as explants or as implants. Explants are the most commonly done procedure where the buckle is sutured to the sclera while in the implant technique they are placed in the bed of the dissected sclera. Scleral explant procedure was initially described by Custodis 2 which Lincoff later modified 8 while the implant method was popularised by Schepens 9. Both the above techniques have the following steps in common
-
conjunctival peritomy and tenotomy
-
Isolation of the recti muscles.
-
Localisation of breaks with IDO
-
Retinopexy with Cryotherapy /diathermy
-
Suture placement / scleral bed dissection and placement of buckle is then performed.
-
Subretinal fluid drainage is done based on surgeon preference and case based need.
-
Break buckle relation and adjustment of buckle height,
-
Careful monitoring of central retinal artery perfusion is done ( AC Paracentesis done if required)
-
Finalisation of buckle and encirclage
-
Closure of the conjunctiva
Contentious issues in Scleral buckling.
A. Cryotherapy vs laser photocoagulation
In a randomised clinical trial by Lira et al 39 in eighty six patients with uncomplicated retinal detachment, both techniques of retinopexy were shown to have satisfactory anatomical and functional success. Laserpexy offered faster visual acuity recuperation with fewer postoperative complications but required a second intervention and was costlier than cryotherapy. They opined that laserpexy to be a successful alternative to cryopexy in creating chorioretinal adhesion for scleral buckle surgery
B. Need for drainage of subretinal fluid?
Drainage of subretinal fluid is one of the debatable issues in scleral buckling. As this step is almost a blind procedure it is not free from potential complications that include choriodal hemorrhage, retinal incarceration and intraocular infection. Drainage in scleral buckling surgery is usually done in bullous detachments to visualise the breaks, to make space to allow a large scleral indent without significant increase in intraocular pressure. Hiltonet al.10 compared drainage vs. non drainage in a randomised controlled trial of 120 consecutive patients undergoing scleral buckling procedures. He found no significant difference in the primary success rate (87% in the drainage groupv82% in the non-drainage group), final flattening rate (97% in both groups) or visual acuity outcome between the two groups. Decision on whether to drain subretinal fluid was assigned at random preoperatively and all surgeries were done by a single surgeon. It can be concluded that drainage of subretinal fluid is not an absolute necessity and is indicated only in specific situations.
C. Which is the best method of drainage?
Various methods of drainage have been described:
-
Scleral cut-down and choroidal puncture with diathermy,
-
Scleral cut-down and the choroidal puncture by argon laser via an indirect ophthalmoscope or endoprobe.
-
Needle drain where the sclera and choroid are punctured in one stab with a 3 mm suture needle
-
Needle drainage with 26/27 g needle
Three trials have prospectively compared needle and laser drainage. Ibanezet al. 11 in a randomised study of 175 patients comparing laser drainage choroidotomy using an endoprobe, or needle drainage found no significant difference in the complication rate between the two groups (13%v16%). However, Das and Jalali 12 reported an increased complication rate in the needle drainage group (4/25) than in the laser group however no statistical analysis was provided. Randomised prospective, controlled trial comparing suture needle drainage with argon laser drainage by Aylwardet al13 Argon laser drainage was associated with a lower rate of clinically significant subretinal haemorrhage (4·3%v28·3.%, respectively)and a higher rate (98%) of adequate drainage, compared with suture needle drainage (85%), even though larger sclerostomy created by the argon laser drain was larger it was not associated with any increase in the rate of retinal incarceration. Azad et al 14 compared modified needle drainage with conventional drainage of subretinal fluid (SRF) as described by Schepens in surgery for primary rhegmatogenous retinal detachment. They found the Conventional Drainage group had, more serious SRF drainage complications and opined modified needle drainage is a safe and effective procedure for SRF drainage
Sub-retinal haemorrhage is the dreaded complication and is problematic if it tracks back under the macula. Most retina specialists practice favours the expediency of a needle drain when the macula is attached and the submacular space is closed, while the safer laser drain is preferred when the macula is off. In case of total retinal detachments undergoing buckling, drainage on the nasal side would reduce chances of sub-retinal bleed tracking under the macula in the event of such a complication.
Three trials have prospectively compared needle and laser drainage. Ibanezet al. 11 in a randomised study of 175 patients comparing laser drainage choroidotomy using an endoprobe, or needle drainage found no significant difference in the complication rate between the two groups (13%v16%). However, Das and Jalali 12 reported an increased complication rate in the needle drainage group (4/25) than in the laser group however no statistical analysis was provided. Randomised prospective, controlled trial comparing suture needle drainage with argon laser drainage by Aylwardet al13 Argon laser drainage was associated with a lower rate of clinically significant subretinal haemorrhage (4·3%v28·3.%, respectively)and a higher rate (98%) of adequate drainage, compared with suture needle drainage (85%), even though larger sclerostomy created by the argon laser drain was larger it was not associated with any increase in the rate of retinal incarceration. Azad et al 14 compared modified needle drainage with conventional drainage of subretinal fluid (SRF) as described by Schepens in surgery for primary rhegmatogenous retinal detachment. They found the Conventional Drainage group had, more serious SRF drainage complications and opined modified needle drainage is a safe and effective procedure for SRF drainage
Sub-retinal haemorrhage is the dreaded complication and is problematic if it tracks back under the macula. Most retina specialists practice favours the expediency of a needle drain when the macula is attached and the submacular space is closed, while the safer laser drain is preferred when the macula is off. In case of total retinal detachments undergoing buckling, drainage on the nasal side would reduce chances of sub-retinal bleed tracking under the macula in the event of such a complication.
Pneumatic retinopexy
Pneumatic retinopexy has the major advantage of being an outpatient procedure. The technique was recommended in the management of RD caused by a single break, no larger than one clock hour and located within the superior eight hours of the ocular fundus, or by a group of small retinal breaks within one clock hour, in the absence of grade C or D PVR and uncontrolled glaucoma. Some selected cases with multiple retinal breaks located more than 30° apart can also treated with this technique.
Perfluoropropane (C3F8) and sulfur hexafluoride (SF6) are the most commonly used gases for pneumatic retinopexy. It involves cryopexy of retinal breaks if possible, followed by injection of an intravitreal gas bubble and postoperative positioning to allow the gas bubble to act as a tamponade for the retinal break. If cryopexy is not performed, laser photocoagulation is applied to the retinal breaks after they have been flattened with intraocular gas.
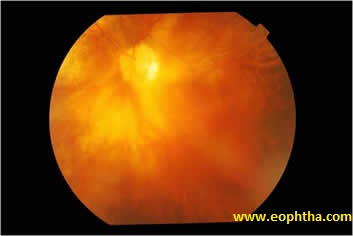
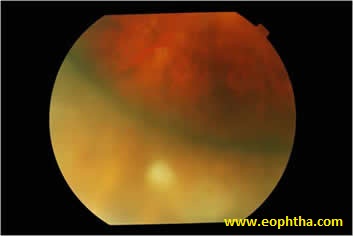
Figure 1c, d: Inferior RD in a patient with High myopia managed successfully with scleral buckling
Complications:Complications of pneumatic retinopexy in the treatment include
-
New retinal break formation in 4–26% of cases,
-
development of new retinal detachment in 15–24% of cases,
-
delayed subretinal fluid absorption in 4–21%,
-
chronic macular detachment in 4.1%,
-
PVR in 3–24%, macular pucker in 2–9%,
-
subretinal gas in about 2%, and
-
endophalmitis in 1% of cases.
Other rare complications include supra-choroidal gas, extension of the retinal detachment, macular hole formation, and entrapment of gas in the pre-vitreous space anterior chamber 15
In a comprehensive review by Clement et al 16 the updated average surgical outcomes for the 4,138 eyes in the 21-year period revealed a single-operation successes(74.4%), final operation successes (96.1%), new retinal breaks (11.7%), and proliferative vitreoretinopathy (5.2%).
Pneumatic retinopexy is an effective procedure. Since the success rate is only marginally less than scleral buckling, it is a viable alternative and is of great use in patients unfit for surgery.
Contentious issues in Pneumatic retinopexy
Question: Is scleral buckling/vitrectomy better than pneumatic retinopexy ?
PR Vs Scleral Buckling
Several controlled trials have evaluated the results The Retinal Detachment Study Group conducted a multi-centre trial and compared pneumatic retinopexy with scleral buckling. They reported results at six months 17, and at 2 years 18; there was no significant difference in either first time (82%v73%) or final (98%v99%) reattachment rate for scleral buckling and pneumatic retinopexy, respectively. Pneumatic retinopexy group had better visual outcomes. Mulverhillet al.19 in small randomised study of 20 consecutive patients, who met inclusion criteria, to be treated either by scleral buckling or pneumatic retinopexy. Retinal flattening was achieved in one operation in 90% of the pneumatic retinopexies and 100% of the scleral buckles. Visual outcome was comparable between the two groups. However, in a meta-analysis of pneumatic retinopexy compared to primary scleral buckling procedures, scleral buckling was found to have a higher primary success rate than pneumatic retinopexy.20
PR vs. Vitrectomy
Pneumatic retinopexy, was found to have a comparable success rate to vitrectomy with cryotherapy and gas in a prospective randomised controlled trial of 120 cases in 1987.21 However it is not desirable to extrapolate this study findings to present day as the technique of vitrectomy was still evolving at that time.
Is pseudophakia a relative contraindication for Pneumatic retinopexy ?
Multiple clinical studies have demonstrated the lower success rate of pneumatic retinopexy in repairing pseudophakic detachments compared with phakic ones, with a range of success from 45% to 80%. 22 This has led Tornambe to recommend 360° peripheral laser at the time of pneumatic retinopexy in pseudophakic detachments, placing several laser rows posterior to the vitreous base. This lower success rate might be due to the higher difficulty in detecting pseudophakic breaks. 17,18 The retinal detachment study group found that most aphakic and pseudophakic eyes that initially failed to pneumatic retinopexy ultimately reattached with fairly good vision, hence recommended the use of pneumatic retinopexy independently to whether the eye was phakic or aphakic/pseudophakic. 17,18 However for many clinicians, pseudophakia still remains a relative contraindication to pneumatic retinopexy.
Primary pars plana vitrectomy (with or without sclera buckling)
Vitrectomy is usually indicated in patients with PVR greater than grade C1, giant retinal tears, posterior breaks, multiple breaks at multiple levels, in patients of iridofundal coloboma with RD.
Over the past decade, more and more surgeons have been advocating pars plana vitrectomy for the primary management of retinal detachments probably due to the vitreo-retinal training patterns and better technology in vitrectomy machinery and wide angle visualization.
Technique involves a standard 3-port pars plana vitrectomy with removal of the juxta basal vitreous. During this process, retinal breaks are identified, freed of vitreous traction and marked. Internal subretinal fluid drainage is then performed by one of 3 techniques: either through the causative anterior breaks using perfluorocarbon liquids or through one of the causative anterior breaks using a cannulated extrusion during fluid–air exchange or through a posteriorly created retinotomy during fluid–air exchange. The breaks are then treated with endolaser, either through perfluorocarbon liquids or under air. Some surgeons will only treat the identified retinal breaks, whereas some other will perform 360° peripheral laser, placing several rows posterior to the vitreous base. The air is finally exchanged for a long-acting gas/ silicone oil. The patient has to maintain position postoperatively. One of the major advantages of vitrectomy over scleral buckling is the greater ability of visualizing retinal breaks with the combined use of wide-angle viewing systems and scleral depression. Retinal break detection is also possible with the help of perfluorocarbon liquids and the Schlieren phenomenon. Many retinal breaks undetectable by ophthalmoscopic examination can thus be found during pars plana vitrectomy. The risks of hemorrhage and retinal incarceration associated with external subretinal fluid drainage are not encountered with endodrainage during vitrectomy.
Other significant advantages of vitrectomy over scleral buckling include the
-
absence of refractive shift,
-
clearance of vitreous hemorrhage/ vitreous floaters,
-
less postoperative pain,
-
lower risk of postoperative diplopia, and
-
Lowered risk of infection.
Removal of the vitreous potentially present in the anterior segment and around the intraocular lens might also be beneficial for postoperative visual recovery.
Disadvantages of pars plana vitrectomy over scleral buckling include a more
-
the requirement for postoperative positioning, and the inability to engage in air travel when gas is used for intraocular tamponade
-
costly surgery, especially if perfluorocarbon liquids are used,
-
the risk of postoperative intraocular lens displacement,
-
Complications:
Intraoperative complications include iatrogenic breaks, optic capture, and retinal haemorrhage.
Postoperative complications include cellophane maculopathy, cystoid macular edema, PVR. Some have also suggested that compartmentalization of fluid against the retinal surface might potentially increase the risk of epiretinal membrane formation.
Factors Determining Anatomical and Functional Success
Several factors appear to have an influence in the anatomical and functional recovery after vitreo-retinal surgery in PRD.
Higher reattachment rates have been achieved in cases in which the macula was attached pre-operatively. Similarly, patients with less extensive RDs appear to have better anatomical outcomes after vitreo-retinal surgery.
The presence of PVR at presentation appears to be one of the most important factors determining the anatomical outcome in PRD, with higher redetachment rates in those cases in which PVR is present.
Poor presenting vision and longer duration of symptoms before presentation, the presence of preoperative choroidal detachment, vitreous hemorrhage, large retinal breaks (≥ 1 clock hour), or breaks located posterior to the equator and
The occurrence of intra-operative hemorrhage appear to also be variables predictive of poor anatomical success. (23)
The length of history of the RD (time between the occurrence of RD and the surgical repair) appears to have a major influence in the functional results obtained after surgery. The shorter the history of visual loss, the better the visual recovery following surgery.
Girard 24, 25 found that the presence of anterior chamber reaction and preoperative PVR of grade B or greater were also associated with a poor visual outcome following surgery.
As per the results of the SPR (Sclera buckling vs Primary Vitrectomy in Retinal Detachment) study, 26 a prospective randomized clinical trial comparing scleral buckling surgery (SB) and primary pars plana vitrectomy (PPV) in rhegmatogenous retinal detachments of medium complexity, primary vitrectomy combined with scleral buckling surgery is recommended for the treatment of rhegmatogenous retinal detachment in pseudophakic and aphakic patients. It should be noted that these results do not apply to localized detachments with a single break and patients with proliferative vitreoretinopathy (PVR) grade B or higher and giant tears were excluded from the study.
Figure2. RD with posterior PVR
Figure 3 A RD with significant vitreous haze
Figure 3 B: RD with significant vitreous haze managed with vitrectomy+silicone oil
Figure 4a : Giant retinal detachment
Figure 4b: GRT with rolled flap and bare choroid
Figure 4c: GRT managed with vitrectomy with silicone oil
Contentious issues in Vitrectomy:
1. Optimal intraocular tamponade agent in the surgical management of PVR
The Silicone Study group analysed the efficacy and complications of intraocular gas and silicone oil tamponade in patients with severe PVR and reported its results in a series of publications.27–37 Silicone oil and C3F8 gas were similar in visual acuity and anatomical outcomes. No difference was found in keratopathy rates and persistent hypotony was more common in C3F8 treated eyes (P< 0·05).
2. Need for scleral buckle / encircling band with vitrectomy
In a prospective, nonrandomized, comparative study in pseudophakic patients Stangos et al 40 did not find any additional benefit of encircling band.
3. 20G vs 23G vs 25G
In a comparison of 20- and 25-gauge vitrectomy for primary repair of rhegmatogenous retinal detachment Kobayashi et al38 reported good anatomic and functional results with 25-gauge vitrectomy and the outcomes were comparable with 20-gauge vitrectomy. Similarly in a comparative study Lewis et al 41 found 20-, 23-, and 25-gauge instruments to be equally effective for primary repair of pseudophakic rhegmatogenous retinal detachment.
Conclusions:
Rhegmatogenous retinal detachment (RRD) can have multiple anatomic presentations. An individualized approach to repair of RRD is necessary for optimal results than following a single stereotyped procedure. Scleral buckling can be a valuable component for repair of retinal detachments as it supports both the existing tears and the vitreous base. However, the use of scleral buckling has decreased in recent years due to the success of vitrectomy alone and the avoidance of complications associated with scleral buckle that include buckle erosion and strabismus.
Based on available evidence the following the principles in management of rhegmatogenous RDs
Phakic RRD is best treated by scleral buckling alone,(figure 1 a-d) unless other problems, such as proliferative vitreoretinopathy(figure 2) opaque media, (figure 3 a,b) blood in the vitreous, , or GRT(figure4 a,b,c) (figure posterior tear, necessitate vitrectomy as well.
Pseudophakic RRD is treated with vitrectomy combined with/without scleral buckling.
Pneumatic retinopexy is reserved for only very simple RRDs.
Some Common representative situations and management options are described in the table below.
Clinical situation
Pneumatic retinopexy
Scleral buckling
Primary vitrectomy
Superior Quadrantic detachment with one peripheral break.
First choice
excellent candidate
for PR, in the absence of contraindicationsFirst choice
segmental scleral buckle placed radially,
if the tear lies under a vertically acting muscle, a segmental circumferential buckle of solid silicone may be preferableSecond choice
Can be considered as first choice if there is significant traction on the edges of the breaks especially in pseudophakics
Total detachment with one break.
Can be considered as First choice
if the tear is in the upper eight clock-hours & patient positioning possibleFirst choice with /without drainage
Especially if the break is the lower 4 clock hours
Encircling band may be needed in the presence of other retinal lesions/traction/early PVRSecond choice
Can be considered as first choice if there is significant traction on the edges of the breaks especially in pseudophakics
Detachment with multiple breaks at same distance from ora
Usually not an option unless
all open breaks are within a 1-2 clock-hoursCan be considered as First choice usually with drainage
Encircling band recommendedCan be considered as first choice especially in pseudophakics
Detachment with multiple breaks at different distances from ora.
Usually not an option
broad buckle grooved silicone implant is employed
First choice
“Aphakic detachment” with multiple small ora breaks.
Usually not an option
Buckling with encircling band Can be considered as First choice
First choice
Encircling band &
A 360-degree
peripheral laser photocoagulation is often applied.Macula off Detachment with peripheral break and pseudomacular hole
As per situation 2,3,4
As per situation 2,3,4
As per situation 2,3,4
Macula off Detachment with peripheral break and macular hole
Can be considered but second surgery may be required for macular hole
First choice
ILM peeling can be consideredDetachment due to macular break
generally seen in association with high myopiaCan be considered
Challenging surgery, good results reported by some surgeons implant may be
sutured to the sclera of the posterior pole.First choice
May require Heavy silicone oil for tamponadeDetachment with retinal dialysis.
First choice:drainage optional
Detachment with giant break.(more than 3 clock hours)
Not an option
Check reports
First choice with or without a low, encircling scleral buckle
PFCL needed to flatten retinaDetachment with no apparent break.
Rule out secondary
retinal detachmentNot considered
Contiguous cryotherapy is applied in one or two rows starting
just posterior to the ora in all detached quadrants.Can be considered as first choice as breaks can be identified with use of PFCL that causes the subretinal fl uid to exit the subretinal space via the break(s),
Staining the subretinal fluid with Trypan blue can also be tried for better visualisationDetachment with outer-layer break in retinoschisis
Not considered
outer-layer breaks should be carefully treated with cryotherapy
and closed with scleral bucklingvitrectomy for those cases in which outer-layer breaks
are far posterior and their buckling would be difficultDetachment with PVR.
Usually not considered
high encircling buckle for Grade C1 or C2 PVR
grade C3 or greater, vitrectomy is recommended and is the mainstay of treatment
References:
1. Gonin J. Le Decollement de la retine. Pathogenie-traitment. Lausanne, Switzerland: Libraire Payot;1934.2. Custodis E. Bedeutet die plombenaufnahung auf die sklera einen fortschritt in der operatven behandlung der netzhautablosung. Ber Dtsch Ophthalmol Ges. 1953;58:102.
3. Hilton GF, Grizzard WS. Pneumatic retinopexy. A two-step outpatient operation without conjunctival incision. Ophthalmology. 1986;93:626-641
4. Vrabec TR, Baumal CR: Demarcation laser photocoagulation of selected macula-sparing rhegmatogenous retinal detachments. Ophthalmology 107:1063--7, 2000
5. Byer NE: Subclinical retinal detachment resulting from asymptomatic retinal breaks: prognosis for progression and regression. Ophthalmology 108:1499--503, discussion 1503--4, 2001
6. Cohen SM: Natural history of asymptomatic clinical retinal detachments. Am J Ophthalmol 139:777--9, 2005
7. Greven CM, Wall AB, Slusher MM: Anatomic and visual results in asymptomatic clinical rhegmatogenous retinal detachment repaired by scleral buckling. Am J Ophthalmol 128:618--20, 1999
8. Lincoff HA, Baras I, McLean J. Modifications to the Custodis procedure for retinal detachment. Arch Ophthamlol. 1965;73:160
9. Schepens CL, Okamura ID, Brockhurst RJ. The scleral buckling procedures. I: surgical techniques and management. Arch Ophthalmol. 1957;58:797-811.
10. Hilton GF, Grizzard WS, Avins L et al. The drainage of subretinal fluid. A randomized controlled clinincal trial. Retina 1981;1:271–80.
11. Ibanez HE, Bloom SM, Olk RJ et al. External argon laser choroidotomy versus needle drainage technique in primary scleral buckle procedures. A prospective randomised study. Ophthalmology 1994;14:348–50.
12. Das TP, Jalali S. Laser-aided external drainage of subretinal fluid: prospective randomized comparison with needle drainage. Ophthalmic Surg 1994;25:236–9.
13. Aylward GW, Orr G, Scwhartz SD, Leaver PK. Prospective ,randomised, controlled trial comparing suture needle drainage and argon laser drainage of subretinal fluid. Br J Ophthalmol 1995;79:724–7.
14 Azad R, Kumar A, Sharma YR, Rajpal. Modified needle drainage. A safe and efficient technique of subretinal fluid drainage in scleral buckling procedure. Indian J Ophthalmol. 2004 Sep;52(3):211-4.
15. Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol 2003 and 48:467-87.
16. Clement K. Chan, Steven G. Lin, Asha S.D. Nuthi, David M. Salib, Surv Ophthalmol 53:443--478, 2008.
17. Tornambe PE, Hilton GF, The Retinal Detachment Study Group. Pneumatic retinopexy. A multicenter randomized controlled trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1989;96:772–84.
18. Tornambe PE, Hilton GF, Brinton DA et al. Pneumatic retinopexy. A two-year follow-up study of the multi-center clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1991;98:1115–23.
19. Mulverhill A, Fulcher T, Datta V, Acheson R. Pneumatic retinopexy versus scleral buckling: a randomised controlled trial. Ir J Med Sci 1996;165:274–7.
20. Sharma S. Meta-analysis of clinical trials comparing scleral buckling surgery to pneumatic retinopexy. Evidence-based Eye Care 2002; 3:125–8
21. Van Effenterre G, Haut J, Larricart P, Abi-Rached J, Vachet JM. Gas tamponade as a single technique in the treatment of retinal detachment: is vitrectomy needed? Graefe’s Arch Clin Exp Ophthalmol 1987;225:254–8
22. William H. Ross, et al: Pneumatic retinopexy, scleral buckling, and vitrectomy surgery in the management of pseudophakic retinal detachments, 2008, Can J Ophthalmol and 43:65-72.
23. Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol 2003 and 48:467-87.
24. Girard P, Gaudric A, Lequoy O, et al: Pseudophakic retinal detachment. Ophthalmologica 203:30-7, 1991.
25. Girard P, Karpouzas I: Pseudophakic retinal detachment: Anatomic and visual results. Graefes Arch Clin Exp Ophthalmol 233:324-30, 1995
26. Heinrich Heimann, et al. Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment. A prospective randomised multicentre clinical study. Ophthalmology 2007 and 114:2142-2154.
27. Azen SP, Boone DC, Barlow W et al. and The Silicone Study Group. Methods, statistical features, and baseline results of a standardized, multicentered ophthalmologic surgical trial: The Silicone Study. Control Clin Trials 1991;12:438–55.
28. The Silicone Study Group. Vitrectomy with silicone oil or sulphur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 1. Arch Ophthalmol 1992;110:770–9.
29. The Silicone Study Group. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol 1992;110:780–92.
30. McCuen BW, Azen SP, Stern W et al. and The Silicone Study Group. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy. Silicone Study Report 3. Retina 1993;13:279–84.
31. Blumenkranz MS, Azen SP, Aaberg T et al. and The Silicone Study Group. Relaxing retinotomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy. Silicone Study Report 5. Am J Ophthalmol 1993;116:557–64
32. Hutton WL, Azen SP, Blumenkranz MS et al. for The Silicone Study Group. The effects of silicone oil removal. Silicone Study Report 6. Arch Ophthalmol 1994;112:778–85.
33. Abrams GW, Azen SP, Barr CC et al. and The Silicone Study Group.The incidence of corneal abnormalities in the Silicone Study. Silicone Study Report 7. Arch Ophthalmol 1995;113:764–9.
34. Cox MS, Azen SP, Barr CC et al. for The Silicone Study Group. Macular pucker after successful surgery for proliferative vitreoretinopathy. Silicone Study Report 8. Ophthalmology 1995;102:1884–91.
35. Lean J, Azen SP, Lopez PF, Qian D, Lai MY, McCuen B for The Silicone Study Group. The prognostic utility of the Silicone Study classification system. Silicone Study Report 9. Arch Ophthalmol 1996;114:286–92.
36. Diddie KR, Azen SP, Freeman HM et al. for The Silicone Study Group. Anterior proliferative vitreoretinopathy in the Silicone Study. Silicone Study Report 10. Ophthalmology 1996;103:1092–9.
37. Abrams GW, Azen SP, McCuen BW, Flynn HW, Lai MY, Ryan SJ for The Silicone Study Group. Vitrectomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy: results of additional and long-term follow-up. Silicone Study Report 11. Arch Ophthalmol 1997;115:335–44.
38. Kobayashi S, Sato S, Inoue M, Yamane S, Watanabe Y, Arakawa A, Uchio E, Kadonosono K. Comparison of 20- and 25-gauge vitrectomy for primary repair of rhegmatogenous retinal detachment.Ophthalmic Surg Lasers Imaging. 2010 Sep-Oct;41(5):550-4.
39. Lira RP, Takasaka I, Arieta CE, Nascimento MA, Caldato R, Panetta H. Cryotherapy vs laser photocoagulation in scleral buckle surgery: A randomized clinical trial Arch Ophthalmol. 2010 Dec;128(12):1519-22.
40. Stangos AN, Petropoulos IK, Brozou CG, Kapetanios AD, Whatham A, Pournaras CJ Pars-plana vitrectomy alone vs vitrectomy with scleral buckling for primary rhegmatogenous pseudophakic retinal detachment Am J Ophthalmol. 2004 Dec;138 (6):952-8.
41. Lewis SA, Miller DM, Riemann CD, Foster RE, Petersen MR. Comparison of 20-, 23-, and 25-Gauge Pars Plana Vitrectomy in Pseudophakic Rhegmatogenous Retinal Detachment Repair. Ophthalmic Surg Lasers Imaging. 2010 Dec 30:1-7.






