Uvea is the middle vascular coat of the eyeball. From anterior to posterior, the uvea or uveal tract can be divided into three parts- Iris, Ciliary body, and choroid. The name “uvea” has originated from the Latin word grape. Why a grape? If the stem is removed from a grape, the hole looks like the pupil and the grape the eyeball.
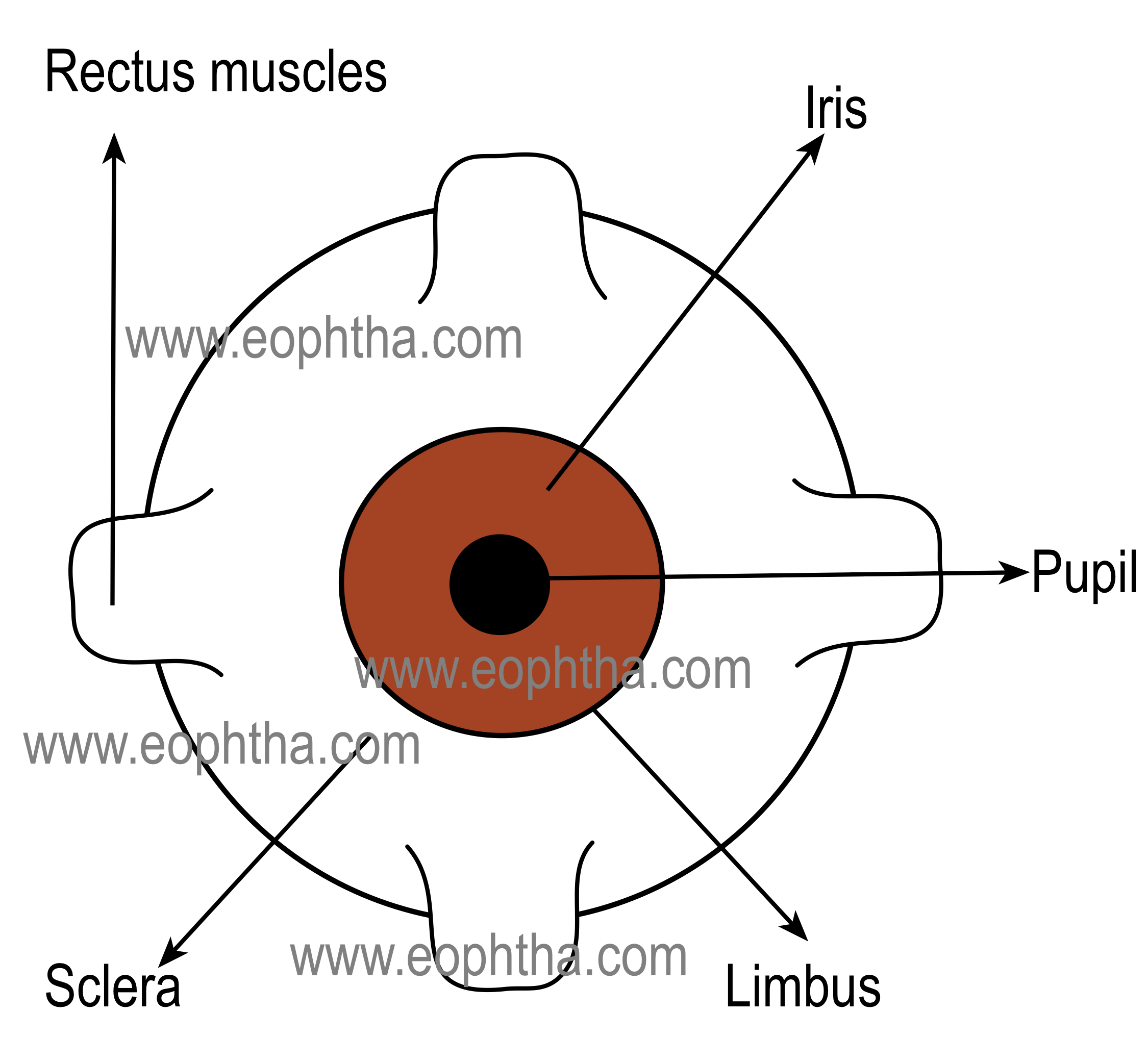
Iris:
Iris is the anterior-most part of the uveal tract. It is a thin and circular structure which forms a diaphragm like structure in front of the crystalline lens. The word “iris” has originated from a Greek word. In Greek mythology, the iris is the name of the Greek goddess of the rainbow.
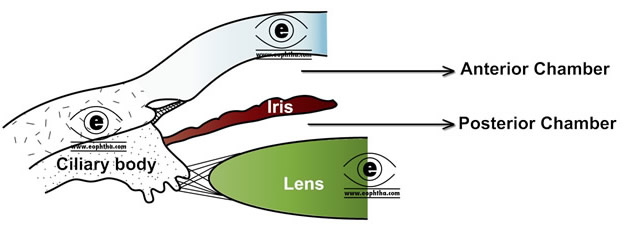
The diaphragm formed by the iris contains a central aperture known as the pupil. The location of the pupil is not exactly central, its little nasal to the center. The pupil determines the amount of light entering the eye. The normal size of the pupillary aperture is 3-4 mm. Details on the pupil will be discussed in chapter "Pupil".
Iris is attached to the middle of the anterior surface of the ciliary body. The iris divides the space in front of the lens into the anterior chamber and posterior chamber.
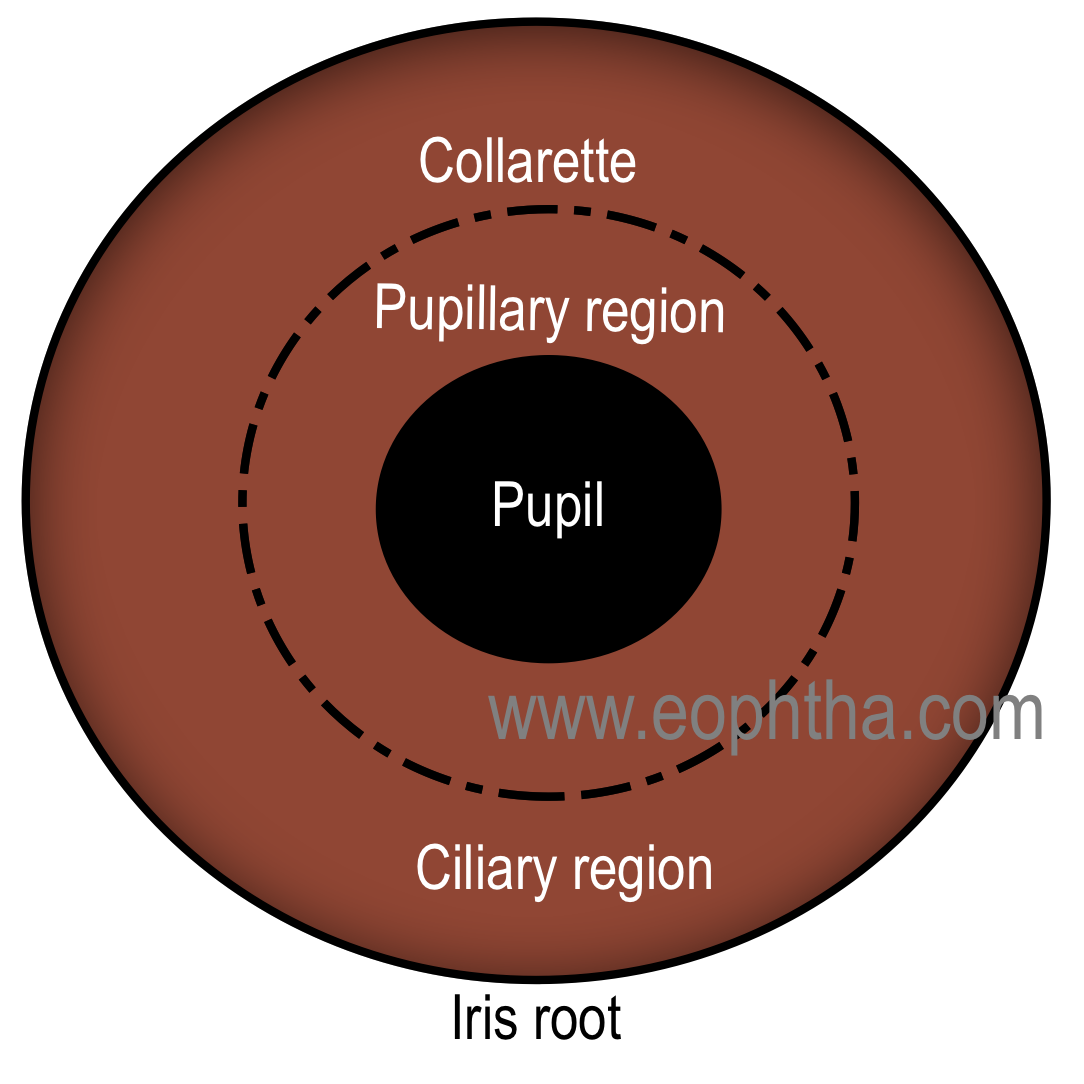
The topography of Iris:
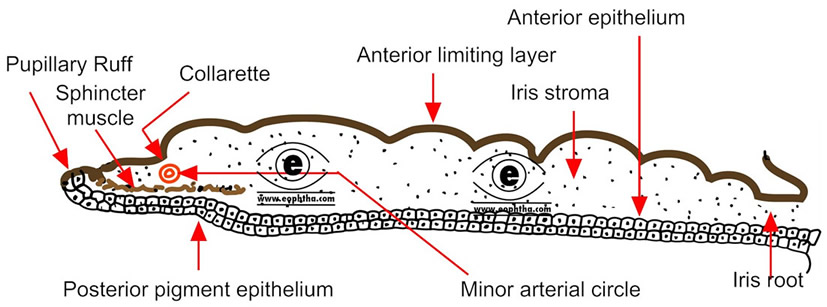
The average diameter of the iris is 10 to 11 mm. It is thickest at the collarette, which is located approximately 1.5 mm from the pupillary margin and thinnest at the iris root, the part of the iris which joins with the ciliary body. The thickness of the iris root is approximately 0.5 mm.
During blunt trauma, damage to the iris occurs most commonly at the iris root, where the iris rips away from the ciliary body
The anterior surface of the iris is divided into a pupillary zone and a ciliary zone by a circular ridge, located 1.5 mm away from the pupillary margin, called collarette (also known as iris frill).
Pupillary Zone:Pupillary zone extends from the pupillary margin to the collarette. The pupillary zone is relatively flat. The pupillary margin is marked by a dark border, known as a pupillary ruff. Pupillary ruff is the anterior termination of the pigmented layer, which lines the posterior surface of the iris.
Ciliary Zone:Ciliary zone of the iris extends from the collarette to the iris root. There are some depressions or pit arranged in rows present in this area known as crypts. Crypts are found in two locations. Those present near the collarette are relatively larger and known as Fuchs’s crypt and few are seen in the periphery of the iris.
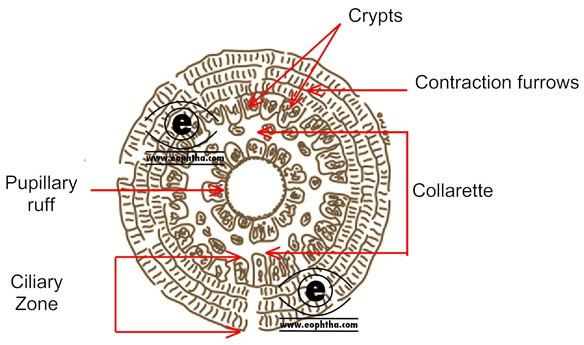
Collarette is the site of fetal pupillary membrane attachment.
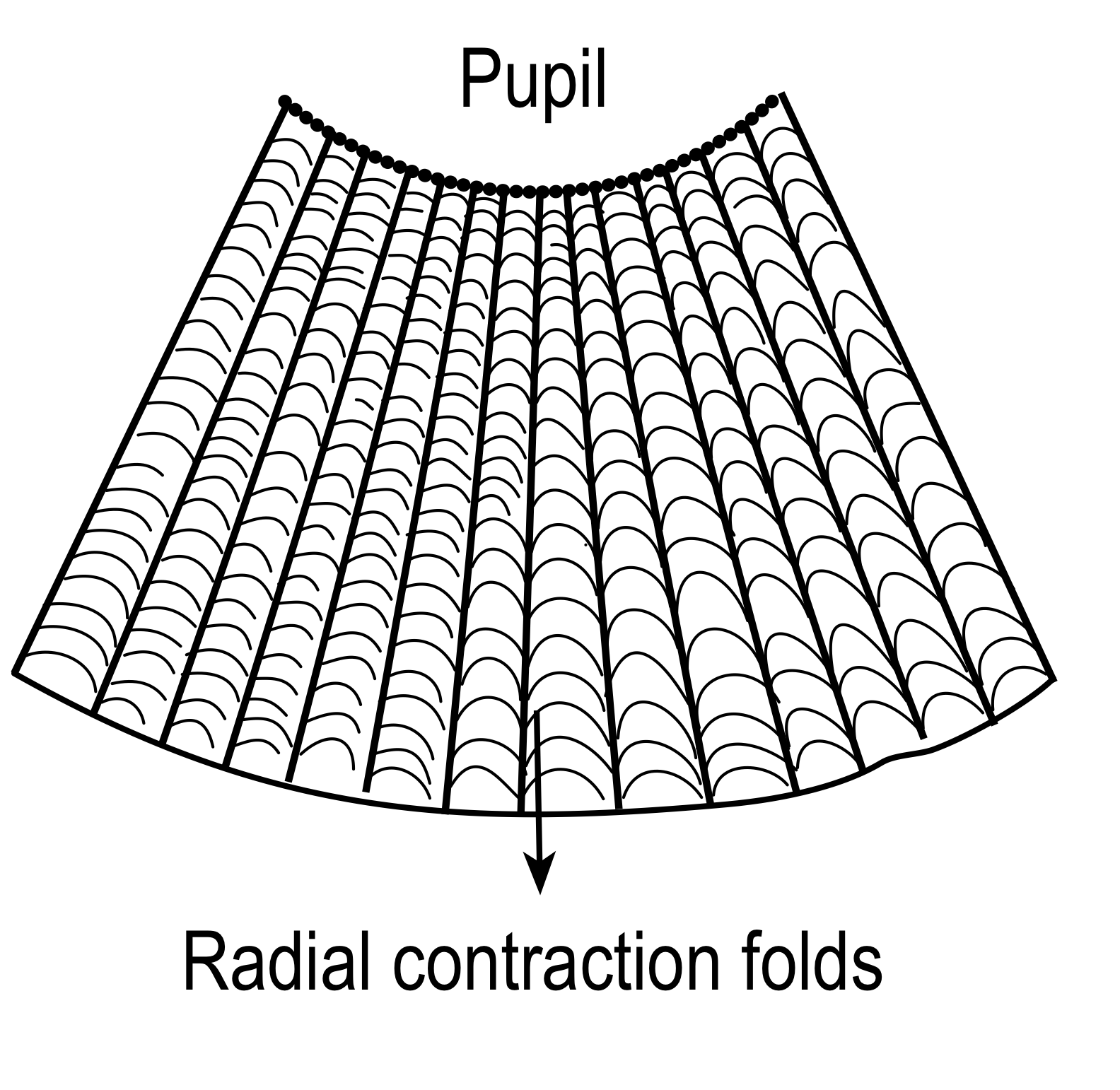
The posterior surface of Iris:Posterior surface of the iris is much more uniform.The posterior surface of the iris is darker than the anterior surface and shows numerous radial contraction folds. However circular folds are also seen.
In laser iridotomy, the opening is created in areas of iris crypts, as it requires less amount of energy in these thinnest areas of iris thickness.
The microscopic structure of Iris :
1. Anterior limiting layer:
The anteriorlimiting layer lines the iris and is the anterior-most condensations of the iris stroma. The layer consist of mainly fibroblasts and melanocytes. These cells are arranged in a meshwork-fibroblasts are located on the surface and melanocyte beneath them.
The color of the iris depends on the thickness of the layer and melanocyte dispersed in the anterior limiting layer. The color of the iris is largely determined by three main variables: (1) the density and structure of the iris stroma, (2) the pigment epithelium, and (3) the pigment content (granules) within the melanocytes of the iris stroma
Heterochromia of iris (Greek:heteros'different' +chroma'color'): is of two kinds. Incomplete heterochromia, one iris is a different color from the other. Inpartial heterochromiaorsectoral heterochromia, part of one iris is a different color from its remainder.
The anterior limiting layer is absent in the areas of crypts and very thin at the contraction furrows.
Clinical NuggetNeovascularisation of iris occurs in the anterior limiting layer.
2. Iris stroma:
Iris stroma forms the main bulk of iris tissue and contains sphincter pupillae, dilator pupillae muscles, vessels and nerves.
Cells in iris stroma:
- Pigmented cells = melanocytes + clump cells
- Non-pigmented cells = fibroblasts + lymphocytes + macrophages + mast cells.
Fibroblasts are the most prominent cells in the iris stroma. These cells are located in close association with blood vessels, muscles, and nerves. Melanocytes can be found around the adventitia of blood vessels. Melanocytes contain mitochondria, smooth and rough endoplasmic reticula, free ribosomes and melanin granules in various stages of development. They have long processes with the help of which they form plexuses with fibroblasts and adjacent melanocytes.
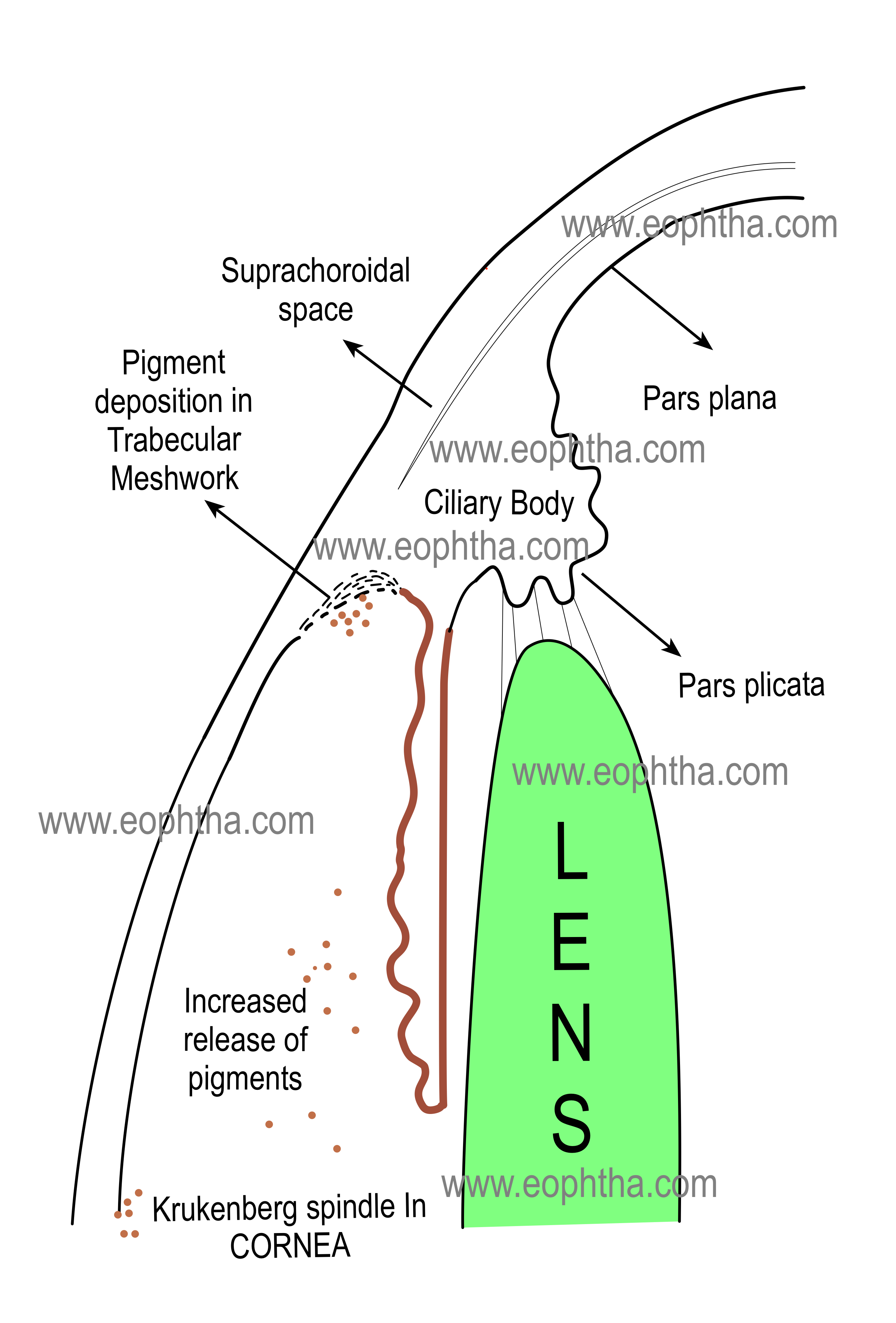
Pigment dispersion syndrome:Pigment dispersion syndrome is a bilateral condition characterized by the liberation of pigment granules from the iris pigment epithelium. It Iscaused by the mechanical rubbing of the posterior pigment layer of the iris against lens zonules as a result of excessive posterior bowing of the mid-peripheral portion of the iris. However, the pigment epithelium itself may be abnormally susceptible to pigment shedding.
Clump cells (also called clump cells of Koganei ) are large, round, pigmented cells, located in the pupillary portion of the stroma, mainly near the sphincter muscle. There are two types of clump cells. Type I cells are numerous and believed to be “altered macrophages” and they act as scavengers of free pigments, present within the iris. Type II cells are less in numbers and are thought to represent smooth muscle cells in arrested stages of development.
Muscles in iris stroma:
The sphincter pupillae muscle is a circular muscle, 0.75 to 1 mm wide, composed of smooth muscle cells. The muscle is 0.1 to 1.7 mm in thickness and is considerably thicker than the dilator papillae.It encircles the pupil and is located in the pupillary zone of the stroma. The sphincter muscle is firmly adherent to the surrounding stroma of iris. The sphincter muscle is composed of spindle-shaped cells that are oriented parallel to the pupillary margin, so, contraction of the sphincter causes the pupil to constrict (a process known as miosis). The muscle is innervated by the parasympathetic system.
The sphincter pupillae retains its function even if severed radially because of its unique distribution of fibers.
The dilator pupillae muscle extends from the iris root to a point in the stroma below the midpoint of the sphincter. A dense band of connective tissue separates the sphincter and dilator muscles from each other. However, near the termination of the dilator muscle, small projections insert into the sphincter. Because of the radial arrangement of the fibers of the muscle, contraction of the dilator pupillae muscle pulls the pupillary portion toward the root, thereby enlarging the size of the pupil ( a process ka mydriasis). The dilator pupillae muscle is sympathetically innervated. (Read anterior pigment epithelium of iris also).
Blood vessels in iris stroma:
Iris vessels include arterioles, venules, and capillaries. The iris arteries are branches of the major circle of the iris, located in the ciliary body near the iris root. The iris vessels usually follow a radial course from the iris root to the pupil margin. These vessels are surrounded by a dense network of collagenous fibrils which is embedded into the collagen network of the stroma. Such an arrangement of the collagen network prevents the iris vessels from kinking and compression during the extensive iris movement during constriction and dilatation of the pupil. Iris veins have very thin walls consisting of endothelium surrounded by a thin layer of collagen. Capillaries are formed by a single layer of unfenestrated epithelium, which forms a part of the blood-aqueous barrier.
Nerves in iris stroma:
Iris nerves are usually unmyelinated, however, some nerves are found to be enclosed by Schwann cells.
3. Anterior pigment epithelium:
The cells in the anterior pigment epithelial layer of the iris have two distinct portions.
Muscular basal portion anteriorly (lies next to stroma): composed of elongated, contractile, smooth muscle fibers. These muscle fibers extend into the stroma, forming three to five layers of dilator muscle fibers joined by tight junctions
Epithelial apical portion posteriorly (lies above posterior pigment epithelium of iris): composed of pigmented cuboidal epithelium where cells are joined by tight junctions and desmosomes.
The epithelial apical portion of the anterior pigment epithelium is in close apposition with the apical surface of the posterior pigment epithelium. A similar kind of apex-to-apex arrangement is to see between the pigmented and nonpigmented epithelium of the ciliary body. The cause of this apex-to-apex arrangement is due to their common embryologic precursor, the optic cup. The anterior iris epithelium continues posteriorly as the pigmented epithelium of the ciliary body.
4. Posterior pigment epithelium of iris:
Posterior pigment epithelium is the second layer of pigmented epithelium situated posterior to the iris stroma. The cells are rectangular or pyramidal in shape with the round cell nucleus and their cytoplasms contain large pigment granules. The cells of the posterior pigment epithelium are more heavily pigmented than the anterior pigment epithelium. The cells are joined to each other by maculae adherens and occludens. These cells rest on a thin layer of the basement membrane situated posteriorly.
Ciliary body
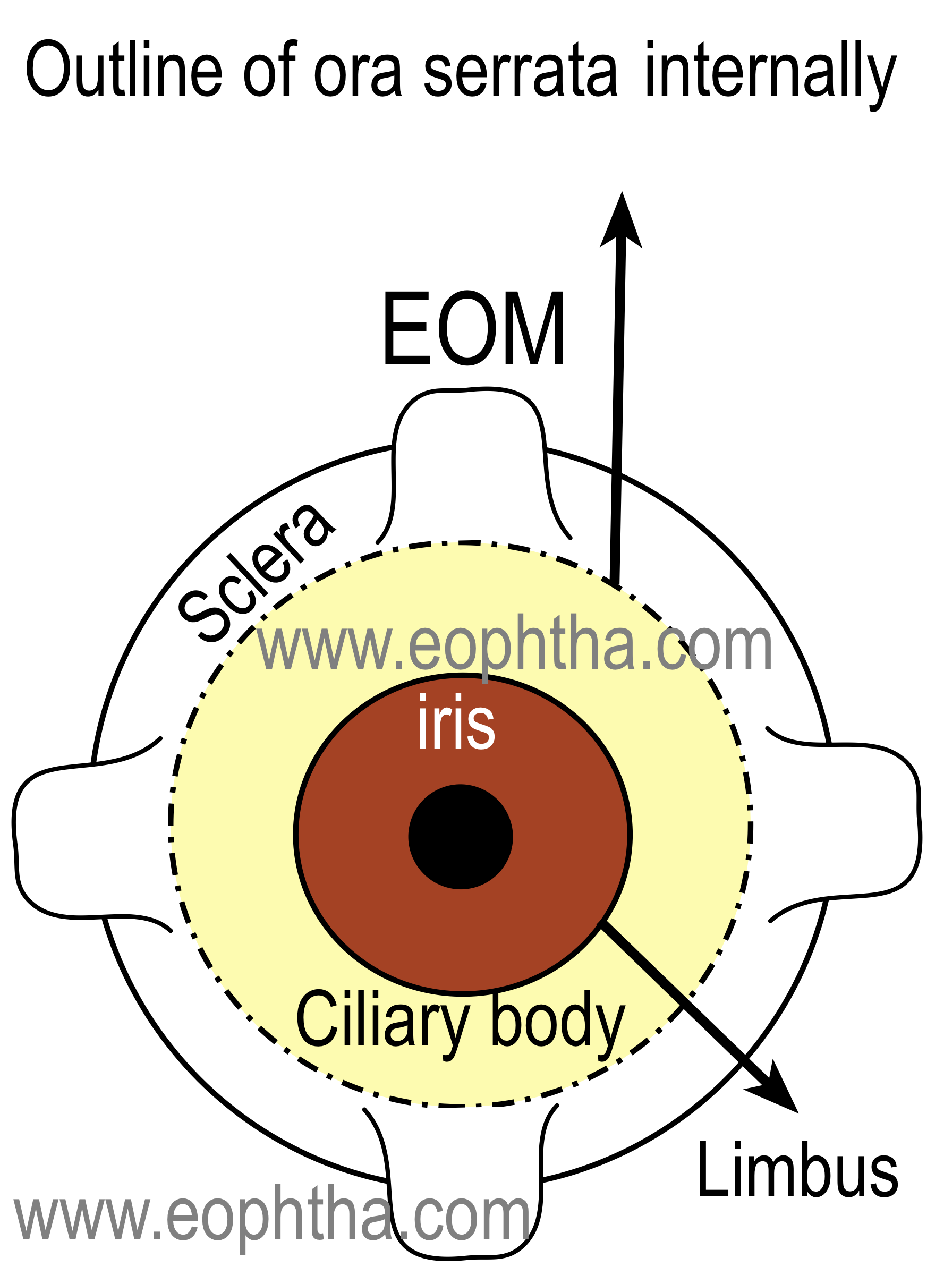
The ciliary body is the middle part of the uveal tract. It is a ring (slightly eccentric ) shaped structure that projects posteriorly from the scleral spur, with a meridional width varying from 5.5 to 6.5 mm. It is brown in color due to melanin pigment. Anteriorly it is confluent with the periphery of the iris (iris root) and the anterior part of the ciliary body bounds a part of the anterior chamber angle. The posteriorly ciliary body has a crenated or scalloped periphery, known as ora serrata, where it is continuous with the choroid and retina. The ora serrata exhibits forward extensions, known as the dentate process, which are well defined on the nasal side and less so temporally. The ciliary body has a width of approximately 5.9 mm on the nasal side and 6.7 mm on the temporal side.
Extension of the ciliary body:On the outside of the eyeball, the ciliary body extends from a point about 1.5 mm posterior to the corneal limbus to a point 6.5 to 7.5 mm posterior to this point on the temporal side and 6.5 mm posterior on the nasal side.
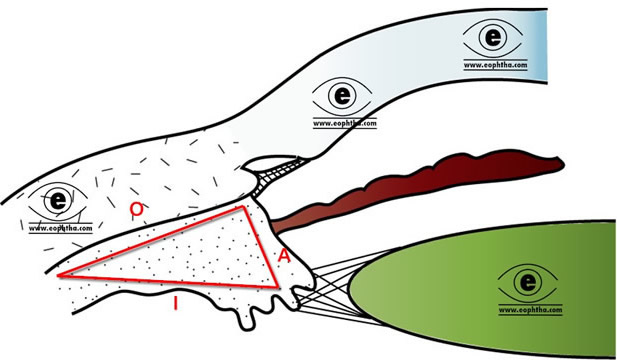
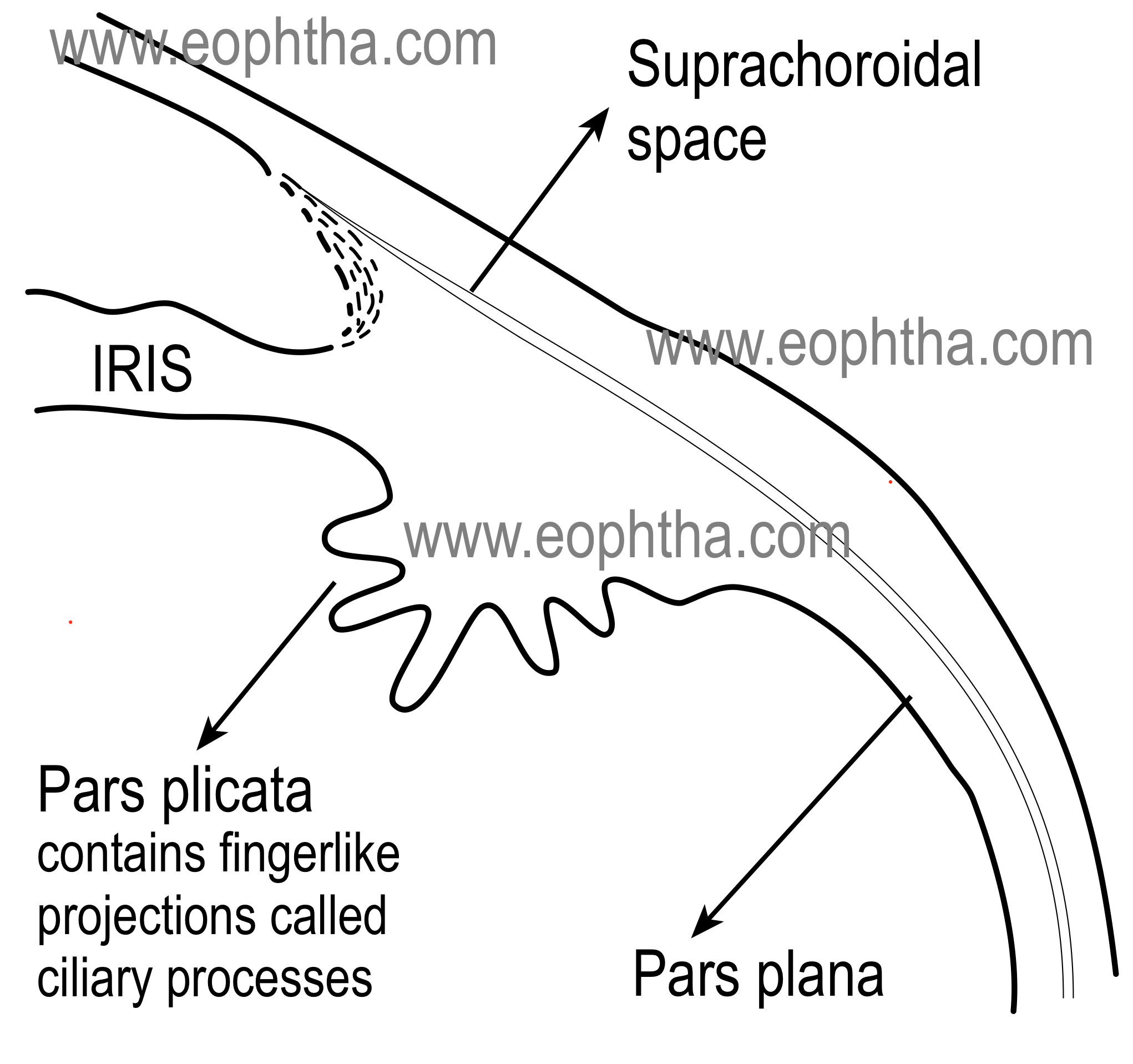
Parts of the ciliary body:Ciliary body, in cross-section, is a triangular structure ( in the diagram it can be compared as the triangle AOI). The outer side of the triangle (O) is attached to the sclera with suprachoroidal space in between. The anterior side of the triangle (A) forms part of the anterior & posterior chamber. In its middle, the iris is attached. The inner side of the triangle (I) is divided into two parts. The anterior part (2 mm) with finger-like processes is known as pars plicata (corona ciliaris) and the posterior smooth (4 mm) is known as pars plana (orbicularis ciliaris).
Pars plicata:The pars plicata is the portion of the ciliary body that contains the ciliary processes. Ciliary processes are the finger-like projections, which extend into the posterior chamber. The regions between ciliary processes are called valleys of Kuhnt. They are approximately 70 to 80 in numbers. A ciliary process measures approximately 2 mm in length, 0.5 mm in width, and 1 mm in height.
Pars plana:As discussed earlier, pars plana is the flat or smooth part of the ciliary body. It terminates at the ora serrata, which is the transitional zone between the ciliary body and choroid. Histologically, the pars plana consist of a double layer of epithelial cells: the inner, nonpigmented epithelium, which is continuous with neurosensory retina; and the outer, pigmented epithelium, which is continuous with the retinal pigment epithelium (RPE).
The pars plana is a relatively avascular zone, which is important surgically in the pars plana approach to the vitreous space. The pars plana provide surgical access to the vitreous and retina.
Ora serrata: the transition zone:
The ora serrata can be termed as the anterior border of the neurosensory retina. Ora serrata shows forward extensions into the retina, which are well defined in the nasal side and less so temporarily. Dentate processes are “teeth-like” extensions of the neurosensory retina into pars plana. There are approximately 20 to 30 dentate processes per eye. Ora bays are rounded extensions of the pars plana.
Topographically, ora serrata corresponds to the insertion of the medial and lateral rectus muscles.
Lens and ciliary body:
The zonules course from ciliary body to the lens. Some of these zonular fibers insert into the internal limiting membrane of the pars plana region and travel forward through the valleys (valleys of Kuhnt) between the ciliary processes. It can be mentioned here that the distance between the equator of the lens and ciliary body is approximately 0.5 mm.
Layers of the ciliary body:
From inside to outside (from sclerad to vitread ), the ciliary body consists of the following four layers.
1. Ciliary epithelium:
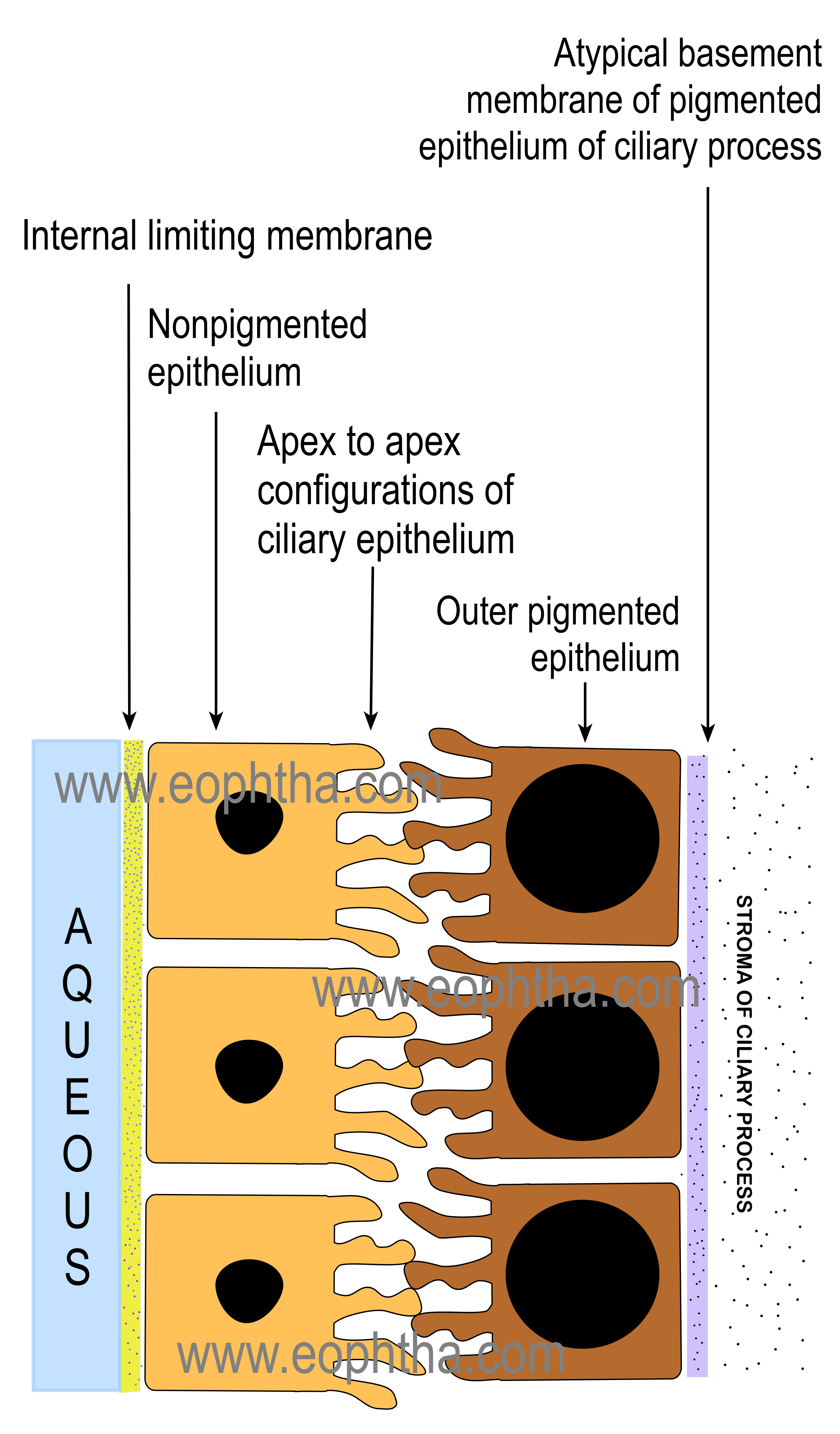
The ciliary epithelium consists of two-layer which cover the inner surface of the ciliary body ( don't confuse !! from the vitreous side, it is the external side). these two layers are representative of two layers of optic cup embryologically.
1A. Non pigmented epithelium (NPE) of the ciliary body :
NPE of the ciliary body extends from iris root to ora serrata. It begins as a continuation of the posterior pigmented epithelium of the iris near the iris root. In the nonpigmented epithelium of ciliary body, cells become smaller and there is significant decrease in melanin granules in the cells . At pars plicata, cells are cuboidal and they gradually become columnar with increasing ages. At ora serrata, the NPE continues as the sensory retina.
The internal limiting membrane is secreted by the basal lamina of the non-pigmented epithelium on its basal surface, which is on the vitreal side. It is the continuation of the inner basement membrane of the iris and continues posteriorly as the inner basement membrane of the retina. It gives origin to parts of the suspensory lens ligament.
1 B. Pigmented epithelium of ciliary body:
The cells of the pigmented epithelium are 8 to 10 micron wide and contain large pigment granules. These pigment granules are three to four times larger than those of the choroid and retina. These cells are rich in organelles and are very active metabolically.
The cells of pigment epithelium secrete the basement membrane which continues posteriorly with the retinal pigment epithelium (RPE).
Ciliary epithelium: metabolic activity
The cells of both the ciliary epithelium have a greater number of mitochondria and thus they have a higher degree of metabolic activity, with a significant role in the active secretion of aqueous humor.
As the name suggests, pigmented epithelium cells have large melanosomes that occupy almost the whole of the cytoplasm. It has to be kept in mind that because of the unique apex to apex configuration of the cells of non-pigmented and pigment epithelium of the ciliary body, the basement membrane of the non-pigmented epithelium faces the posterior chamber whereas the basement membrane of the pigmented epithelium of the ciliary body rests on the stroma of the ciliary body.(See Ciliary Process below)
2. Ciliary stroma:
The ciliary stroma consists of bundles of loose connective tissue. The ciliary stroma contains blood vessels, nerves, and ciliary muscle. Ciliary stroma continues anteriorly with iris stroma and continues posteriorly with choroidal stroma after thinning out at pars plana.
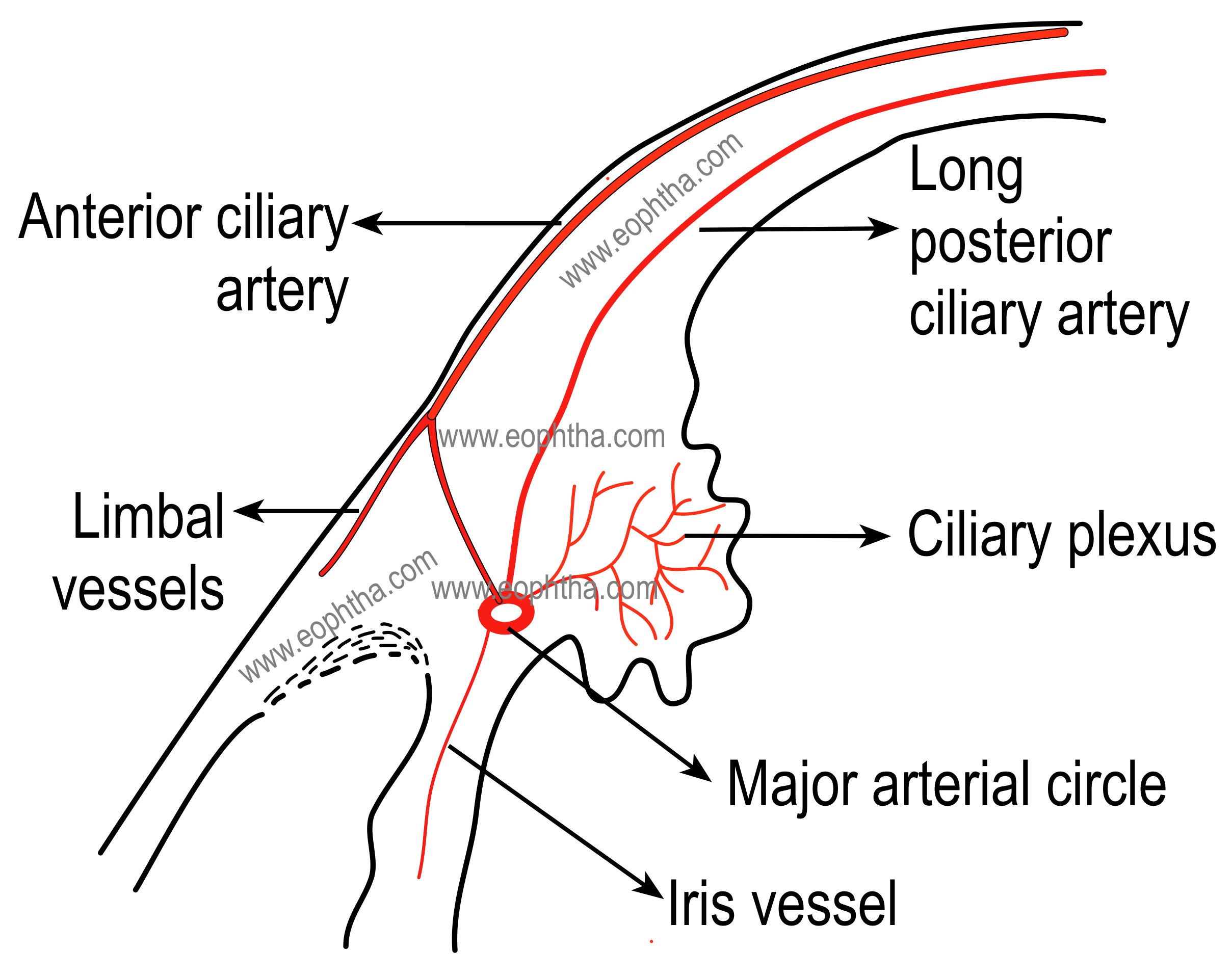
Blood vessels in ciliary stroma: Major arterial circle of the iris
Major arterial circle of iris, formed by the anastomosis of long posterior ciliary arteries and anterior ciliary arteries, is located in ciliary stroma near iris root just in front of the circular portion of the ciliary muscle. Ciliary stroma also consists of numerous capillaries which are fenestrated and large in size. The capillaries are more in numbers in ciliary processes, making them the most vascular organ of the eye.
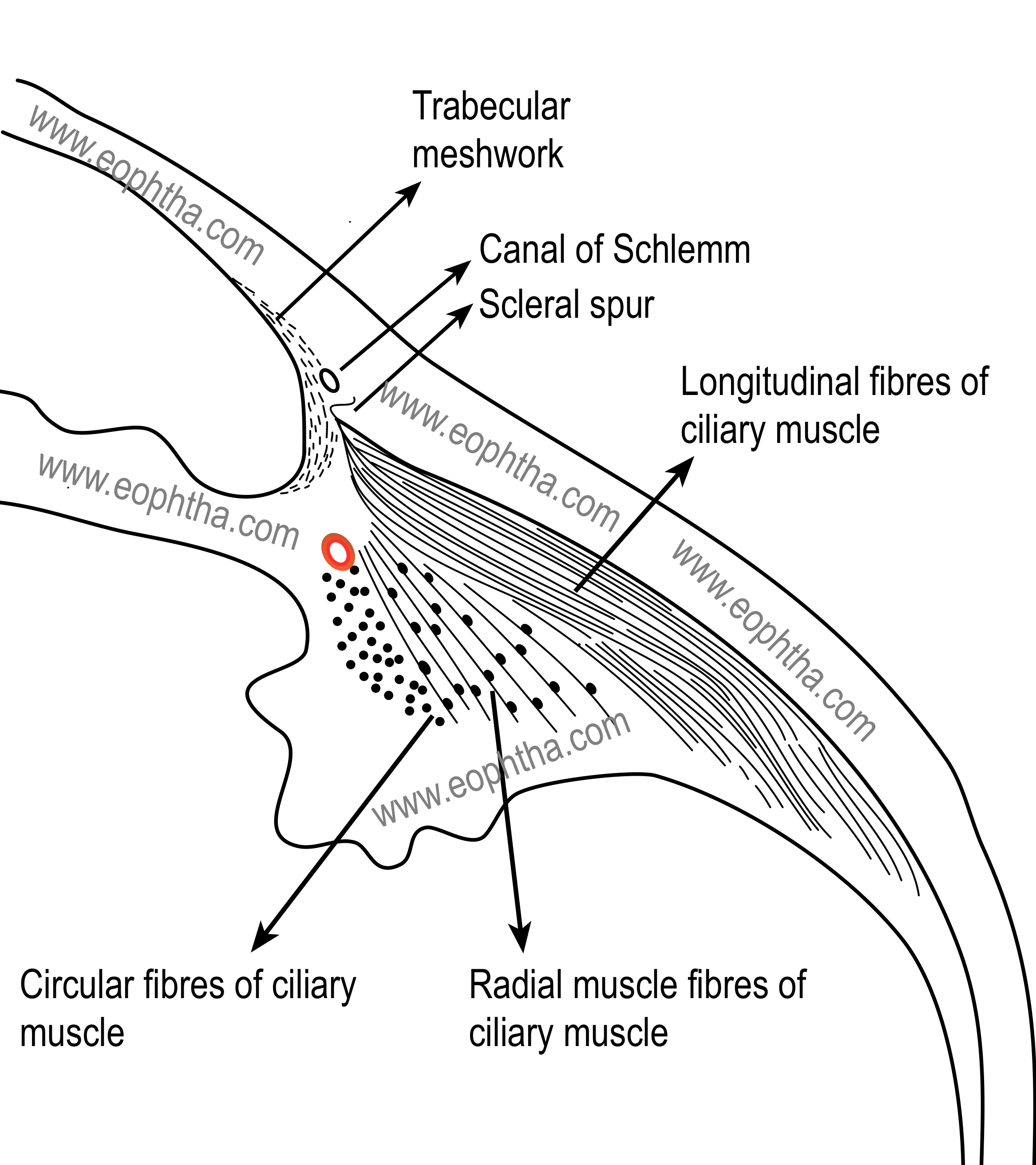
The muscle in ciliary stroma: ciliary muscle
The ciliary muscle is a nonstriated or smooth muscle primarily situated in the anterior two-thirds of the ciliary body stroma. The muscle has three parts
- Outer longitudinal or meridional portion (Brücke's muscle):This is the most external part (nearest to the sclera) of the ciliary muscle. This part of the muscle is v-shaped, the base of the v is attached to the scleral spur and limbs are inserted into the stroma of the choroid.
- Middle oblique portion (also called reticular or radial): This part of the muscle also originates from the scleral spur and the muscle fibers are attached to the collagenous substances near ciliary processes.
- Inner circular portion (Müller's muscle):Here the muscle bundles are circular in shape ( that's why it is also called the annular part of the ciliary muscle) and act as a sphincter. It lies close to the periphery of lens and embedded in ciliary stroma near the major arterial circle of iris.
Contraction of the ciliary muscle, especially of the longitudinal and circular fibers, pulls the ciliary body forward during accommodation. Read about theaccommodative power of the crystalline lens. This forward movement of the ciliary body relieves the tension in the suspensory lens ligament (zonules), making the elastic lens more convex, and thereby helps the eye in accommodation by increasing the refractive power of the lens.
The ciliary muscle is innervated by the autonomic nervous system, parasympathetic postganglionic fibers derived from the oculomotor nerve. The nerve fibers reach the muscle via a short ciliary nerve. The parasympathetic stimulation activates the muscle for contraction, whereas sympathetic innervation likely has an inhibitory effect.
Parasympathetic fibers, coming from the Edinger Westphal nucleus with the oculomotor nerve, are mixed with nerve fibers from the ciliary ganglion and form a plexus in the ciliary muscle.
Kindly note that while classifying the different parts of the ciliary muscle, the term outer is used as external, meaning nearer to the sclera or to the outer side
Sympathetic fibers from the cervical sympathetic trunk, synapse in the superior cervical ganglion and run to the ciliary muscle via the long ciliary nerve. The sensory fibers, coming from the nasociliary branch of the trigeminal nerve, also run in the long ciliary nerve to the ciliary body and terminate in the ciliary muscle.
Supraciliary lamina:
Supraciliary lamina is the outermost layer of the ciliary body which lies adjacent to the sclera. It is composed of loose connective tissue with collagen strands, fibroblasts, and melanocytes. Some of the collagen strands merge with scleral collagen. Because of the lamellar arrangement of connective tissue in this area, supraciliary lamina acts as a potential space. Thus it also helps aqueous humor to exit by the unconventional pathway.
Ciliary body detachment occurs through supraciliary lamina
Ciliary process :
Ciliary processes are finger-like projections seen in pars plicata of the ciliary body. Ciliary processes are approximately 70 to 80 in numbers in each eye and extend into the posterior chamber, and the regions between these ciliary processes are called valleys of Kuhnt. Zonules of the lens (suspensory ligaments of the lens) are inserted in these valleys. Each of these ciliary processes is 2 mm in length and 0.5 mm in diameter. The ciliary process lies 0.5 mm from the periphery(equator) of the crystalline lens. The ciliary processes are white whereas the valleys of Kuhnt are dark in color.
Ciliary processes increase the surface area of pars plicata, which is approximately 6 square centimeter, approximately five times the surface area of the corneal endothelium.
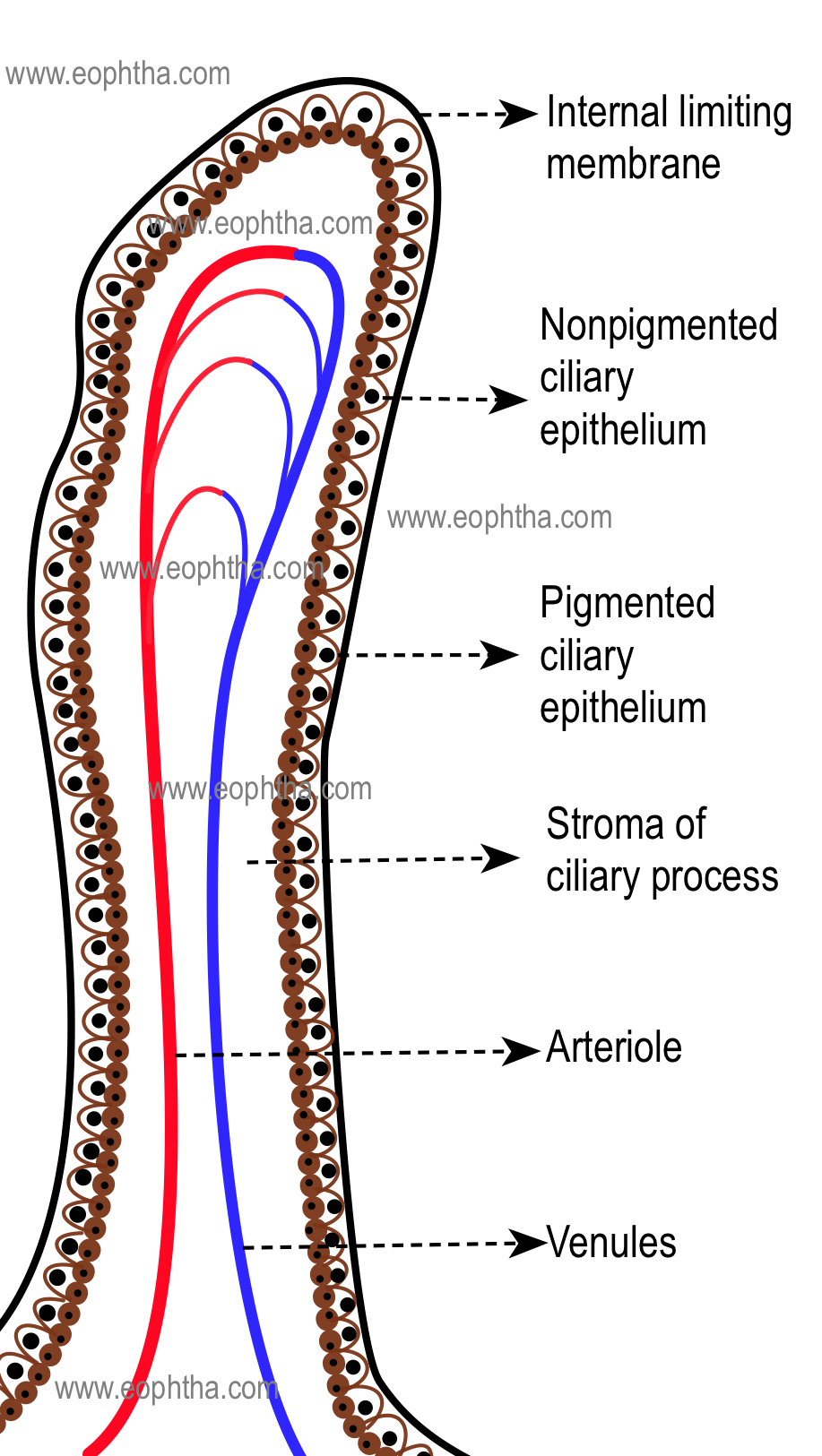
The microscopic structure of a ciliary process can be discussed below.
1. Capillaries: Each ciliary process contains a network of capillaries in its center. These capillaries consist of a thin endothelium which is characterized by numerous fenestrations or pores.
2.Stroma: Connective tissue stroma is very thin and consists of ground substances which include mucopolysaccharides, proteins, collagen connective tissue fibrils, mainly collagen type III, etc.
3. Ciliary epitheliums:Two epithelia namely pigmented and nonpigmented epitheliums are arranged in apex to apex configuration. The outer pigmented epithelium consists of mainly cuboidal cells that contain numerous melanin granulomas. This outer pigmented epithelium has an atypical basement membrane that is situated on the stromal side of the ciliary process. This atypical basement membrane is a continuation of Bruch's membrane of the choroid. The nonpigmented epithelium consists of columnar cells that contain numerous mitochondria, endoplasmic reticulum, etc. The basement membrane of the nonpigmented epithelium faces aqueous humour and is also called the internal limiting membrane.
A variety of intercellular junctions are involved in connecting adjacent cells of two layers of ciliary epithelium and also their apical surfaces. These include gap junctions, puncta adherentia, desmosomes, etc.
Blood supply of ciliary process:
Long posterior ciliary artery, a branch of the ophthalmic artery, pierce the globe near the optic nerve and run-up to the ciliary body to form major arterial circle, which is formed with the anastomosis of anterior ciliary arteries. Several branches from major arterial circle supply ciliary processes. These are mainly pre-capillary arterioles and they divide into a network of capillary plexuses in each of the ciliary processes. These vessels drain into choroidal and intrascleral veins.
The precapillary arterioles supplying the ciliary processes have sphincters which are may be responsible for the autoregulation of blood supply to the tissue
Choroid
The choroid is a thin but highly vascular membrane lining the inner surface of the sclera. It extends from anteriorly ora serrata to the optic nerve posteriorly. It has a rough outer surface which is attached to the sclera at the optic nerve and at the exit of the vortex veins. The smooth inner surface of the choroid is attached to the retinal pigmented epithelium (RPE). Choroid becomes continuous with pia and arachnoid at the optic nerve. The choroid is normally 100-220 µm thick; thickness is highest at macula 500- 1000 µm.
- Choroidal thickness increases in intraocular inflammation.
- The smooth configuration of the choroid can be observed ophthalmoscopically in choroidal detachment
Microscopic structure of choroid:
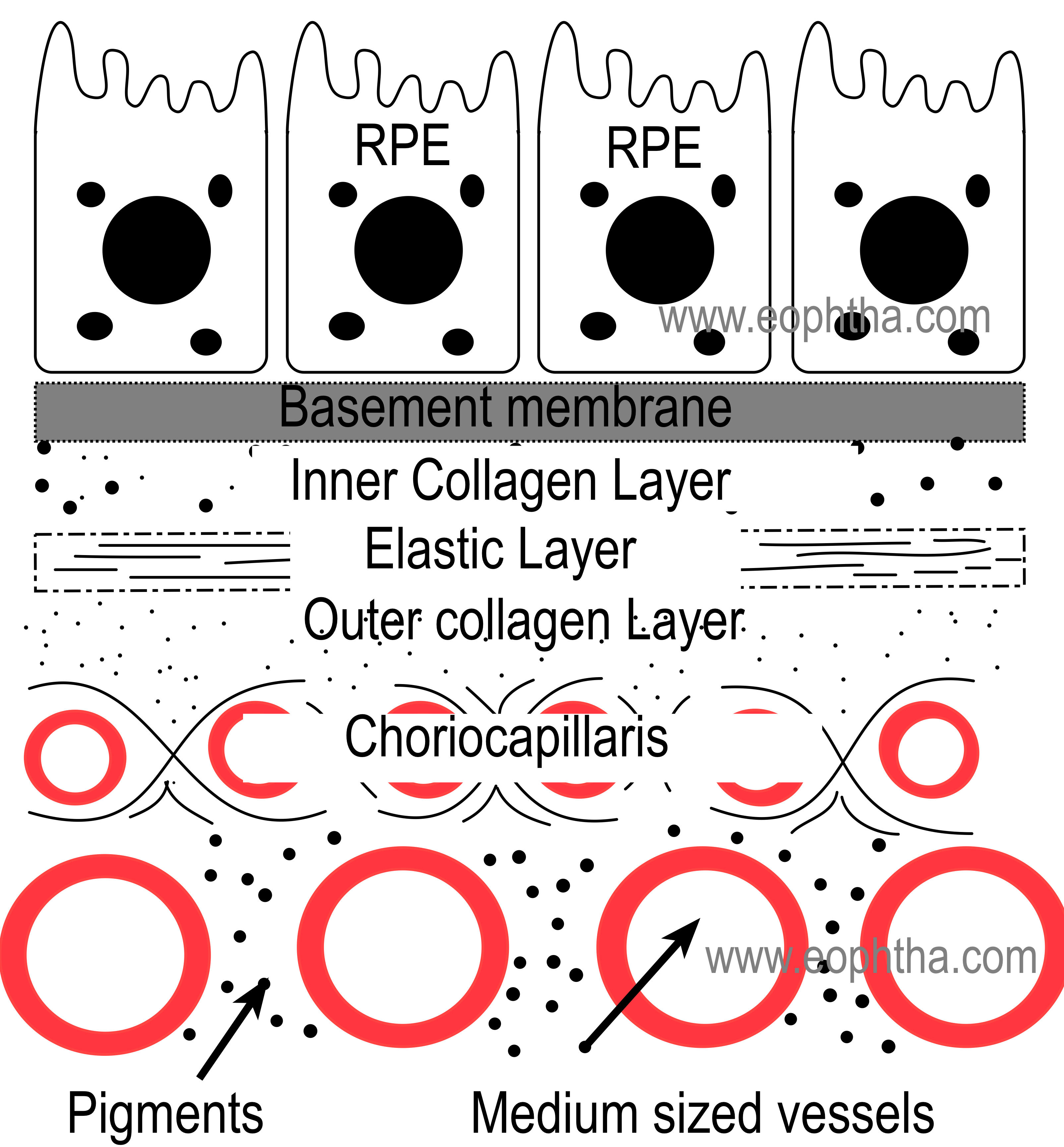
The choroid is composed predominantly of blood vessels surrounded by melanocytes, nerves and connective tissue. Choroid can be divided into the following layers histologically:
1. Suprachoroid lamina (lamina fusca):
Suprachoroid lamina is consists of collagen fibers, fibroblasts, and melanocytes. Suprachoroid lamina overlies a potential space between sclera and choroid known as suprachoroidal space. This potential space contains the long posterior ciliary arteries and nerves.
2. Choroidal stroma:
Unlike tissues like iris, where stroma occupies a major part of the tissue, the choroidal stroma is sparse as the major bulk of choroid is made up of choriocapillaris. The choroidal stroma is a pigmented loose connective tissue which contains the following elements:
- Vessels:The vessels of the choroid are arranged in layers. Larger vessels are located on the outer side and the layer is called Haller's layer. The vessels of this layer branch and form medium-sized vessels. The layer of these medium-sized vessels is known as Sattler's layer. These vessels again branch forming smaller vessels and capillaries. Venues of choroid drain into veins which ultimately drain into four vortex veins (one from each quadrant of the eye).
Choroidal veins are devoid of valve
- Nerves:
- Cells:Melanocytes, fibrocytes, mast cells, and plasma cells are the predominant cells found in choroidal stroma. Melanocytes are distributed heavily in the outer part of the layer and near the optic disc. Among the non pigmented cells, fibroblasts are the most common.
- Connective tissue:Collagen fibrils are dispersed in all directions and surround the blood vessels
3. Layer of Choriocapillaris:
It is a single layer of capillaries which are larger than the normal capillaries of our body. It has been estimated that the lumen of these capillaries are three to four times larger than normal capillaries. The capillary walls are fenestrated and contain pericytes. Choriocapillaries contain a basement membrane.
Pericytes found in capillaries are also known as cells of Rouget. They have contractile functions and are believed to alter the blood flow in capillaries.
Choriocapillaries are thickest and most abundant in the submacular area. Experimentally it has been found that choriocapillaris is arranged in a lobular structure where the feeding arterioles are in the center and draining veins are in the periphery.
Choroidal circulation: tits bits
- Choroidal circulation constitutes 85% of the blood circulation of the eye.
- Choroidal blood flow is higher than that in tissues like the retina and brain.
- Choroidal blood-flow ranges from 800 to 2000 mL/min/100 g of tissue.
- Choroid provides the metabolic requirements of the full retinal thickness only in the macular region.
- In embryonic life, choroid serves as an additional site for the erythropoiesis.
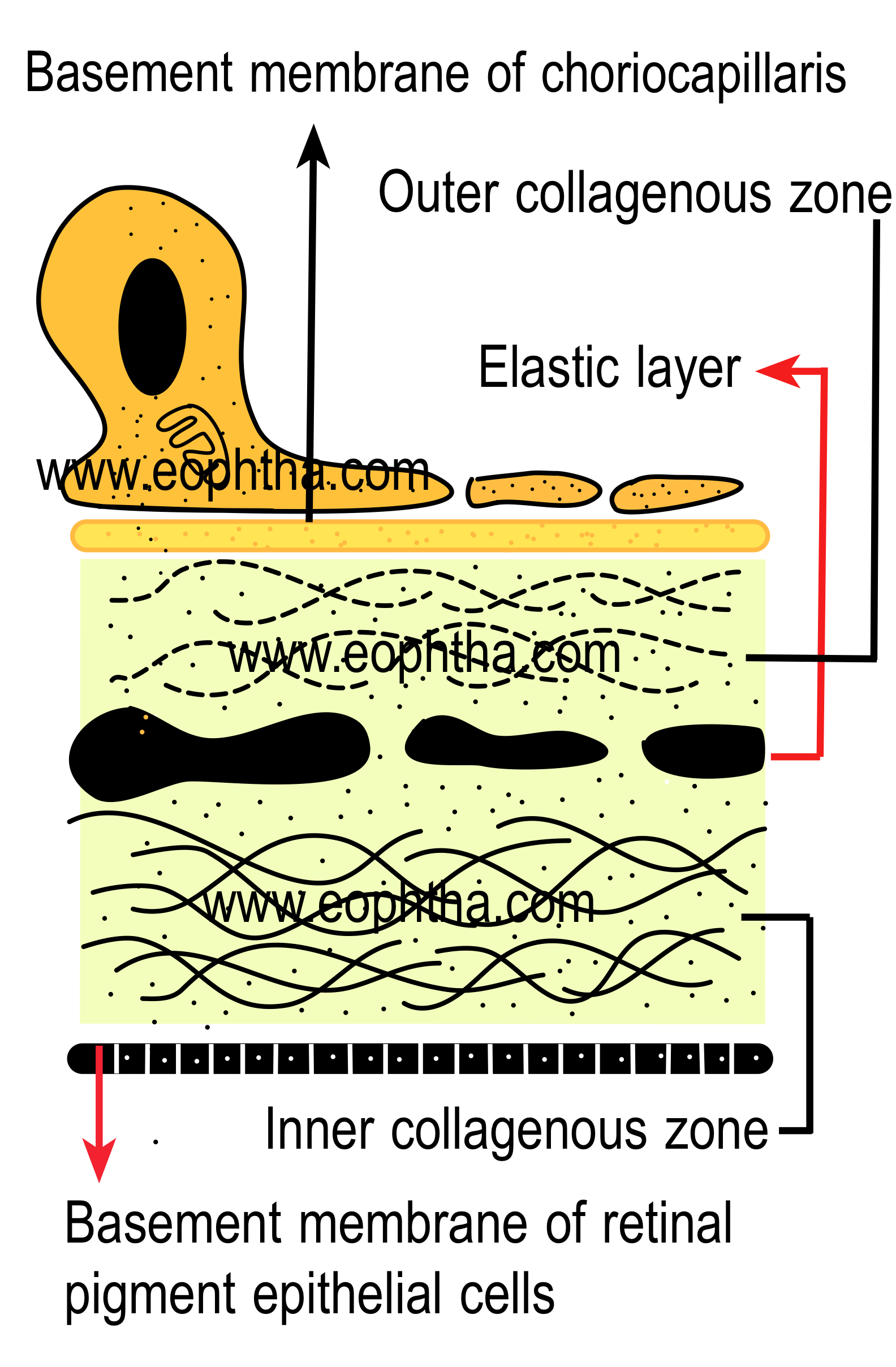
4. Bruch's membrane:
Bruch's membrane is the innermost layer of the choroid and it is also known as lamina vitrea. Bruch's membrane is thickest near the optic disc (2-4 micron) and the thickness decreases towards the periphery. Bruch's membrane is composed of 5 layers and from internal to external, these are
- The basement membrane of the RPE,
- Inner collagenous zone,
- Elastic tissue layer,
- Outer collagenous zone, and
- Basement membrane of the choriocapillaris
Outer blood-retinal barrier
The outer blood-retina barrier (BRB) is composed of three structural entities, the fenestrated endothelium of the choriocapillaris, Bruch's membrane, and the retinal pigment epithelium (RPE).
Various microscopic layers of the uveal tract and their continuation can be summarised in the following table.
|
Iris |
Ciliary body |
Choroid/ Retina |
|
|
Supra ciliary lamina |
|
|
Stroma |
||
|
BM of the anterior iris epithelium |
BM attaches the pigment epithelium to the stroma |
BM of Bruch's membrane of the choroid |
|
Anterior epithelium of the iris |
Pigment epithelium |
Retinal pigment epithelium |
|
Posterior pigment epithelium of the iris |
Nonpigment epithelium |
Sensory retina |
|
Internal limiting membrane |
Internal limiting membrane |
Blood supply of uveal tract:
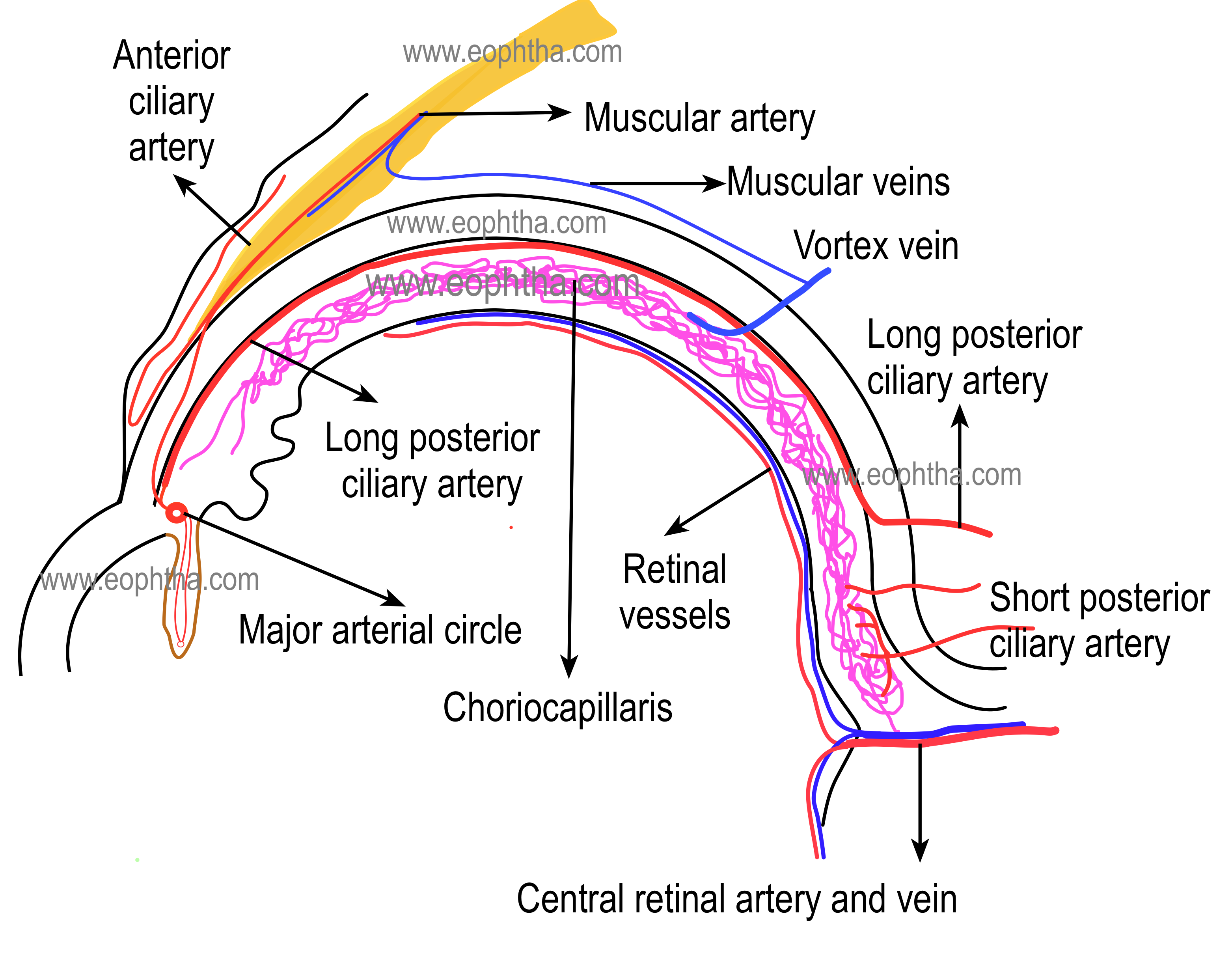
The blood supply of the uveal tract is mainly from three arteries namely short posterior ciliary arteries, long posterior ciliary arteries, and anterior ciliary arteries.
The posterior ciliary arteries are branches of the ophthalmic artery, and many variations can occur in their distribution. (Two-sided table)
SHORT POSTERIOR CILIARY ARTERIES:15 to 20 short posterior ciliary arteries arise → form 10 to 20 branches → enter the sclera in a ring around the optic nerve → anastomose with other branches from the short posterior ciliary arteries to form the circle of Zinn (Zinn-Haller) which encircles the optic nerve at the level of the choroid → they run in suprachoroidal space between sclera and choroid, branch and supply the choroid.
LONG POSTERIOR CILIARY ARTERIES: Two long posterior ciliary arteries enter the sclera: one lateral and one medial to the ring of short ciliary arteries → run between the sclera and the choroid to the anterior globe → enter the ciliary body and branch superiorly and inferiorly → anastomose with each other and with the anterior ciliary arteries to form a circular blood vessel, the major arterial circle of the iris.
ANTERIOR CILIARY ARTERIES: Seven anterior ciliary arteries are derived from muscular branches of the ophthalmic artery ( two each from arteries of the superior rectus, medial rectus, inferior rectus and only one from lateral rectus muscle)→ reach episclera, form plexus, and give branches →pierce sclera near the limbus to enter the eye→anastomoses with long posterior ciliary arteries to form the major arterial circle of iris. Branches from major arterial circle enter iris and anastomoses with each other to form minor arterial circle.


.PNG)