In recent times, eyelid injuries are on the rise primarily because of the increasing incidence of road traffic accidents, industrial mishaps and intentional assaults on the human body. Injury to the eyelids, lacrimal system or orbital wall may be isolated or may occur in association with mid facial injuries.
History
A precise history is essential to assess the severity of the injury. In some cases, an ophthalmologist can anticipate the extent and severity of injury from the mechanism of injury. It is important to elicit the mode of injury, whether it is with sharp or blunt objects or due to thermal or chemical injury or due to dog bites. In cases of animal bites, a complete tetanus immunization history is obtained and if required proper immunization should be given.
Examination Of The Patient
The patient’s injury must be dealt with according to the priority. The basic “ABC’s” (Airway, Breathing, Circulation) must be evaluated, before proceeding to the management of localized injury. The repair of the globe takes precedence over the repair of eyelid laceration(Fig 1). In adnexal injury, the decision whether to repair the wound immediately or to delay repair depends on the degree of tissue edema or the presence of hematoma or infection

Fig 1: Multiple lacerations involving upper and lower lid with open globe injury
OPHTHALMOLOGICAL EXAMINATION
The ocular examination should be performed meticulously. Observation of ocular adenxae is done before manipulating the injured eye.
-
Attempt should be made to determine the visual acuity. Conditions wherein visual system evaluation is difficult, optic nerve and retinal functions may be tested by assessing the pupillary reactions. A confrontation visual field examination should also be done for any field loss, if possible.
-
In the absence of signs of penetrating ocular injury a thorough anterior segment examination, IOP measurement and fundus evaluation must be performed.
-
One should look for the presence of exophthalmos, since this may indicate a retrobulbar foreign body or haemorrhage.
-
Subcutaneous emphysema, anaesthesia of infraorbital skin or bony step offs of orbital rim all indicate orbital bone damage. Presence of marked lid edema may necessitate use of a Desmarre’s lid retractor.
EVALUATION OF THE LID INJURY
-
Duration:The time lapsed since the patient acquired injury is important to decide the approach to wound repair.
-
Mode of injury:Whether it is a blunt or penetrating injury.
Site of Injury:Whether the lid margin is intact or lacerated. Injuries in the region of medial canthus may be associated with lacrimal injuries. (fig 2)

Fig 2- Medial canthal injury with avulsion of lower lid and canalicular laceration
-
Tissue Loss:It is essential to note whether there has been any tissue loss because it may necessitate the mobilization of tissue or skin flaps from adjacent areas or free skin grafts.
-
Infection:If infection is present, the wound repair may be postponed for a few days.
-
Injury to the Levator aponeurosis.Full thickness lid defect or exposed orbital septum suggests injury to Levator muscle or aponeurosis. Inability to look up or absence of any wrinkling of the upper lid skin suggests injury to levator complex.
INVESTIGATIONS
A complete blood count and necessary blood chemistry analysis is carried out. Radiologic evaluation is advised when indicated.
MEDICOLEGAL DOCUMENTATION
All injuries must be documented in detail with drawings and clinical photographs.
TIMING OF SURGERY
In patients presenting within 24 hours of injury, primary repair of the wound is undertaken immediately.
GOALS OF EYELID REPAIR
-
To reestablish anatomical configuration.
-
To restore physiological function.
-
To provide a better cosmetic appearance.
REPAIR OF EYELID INJURIES
Principles to be followed for repair:
-
Local/General anesthesia
-
Sustained haemostasis with infiltration of 2% xylocaine with adrenaline with bupivacaine.
-
Thorough examination (with a focus on the canaliculi , the canthal tendons and the levator function)
-
Cleansing of the wound.
-
Removal of foreign material from the wound
-
Debridement of only that tissue that is conclusively devitalized.
-
Repair of special structures like the canaliculi, canthal tendons and levator aponeurosis
-
Closure in layers.
PRIMARY WOUND MANAGEMENT
Primary wound management may be discussed under the following heads:
-
Repair of non-marginal lid defects
-
Repair of lid margin laceration
-
with minimal loss of tissue
-
with moderate loss of tissue
-
with severe loss of tissue
-
-
Lid laceration involving injury to levator muscle or aponeurosis.
-
Injuries involving lateral canthus.
-
Injuries involving medial canthus
-
Management of canalicular laceration.
-
Total avulsion of an eyelid.
REPAIR OF NON-MARGINAL LID DEFECTS
Simple Lacerations
Smaller linear defects can be sutured without any undermining as they involve only skin and underlying muscle. There should be no tension or vertical pulling effect on the lid margins. Eyelid skin is usually sutured with 6’0 nylon or prolene suture. Non-absorbable skin sutures should be removed in about 5 days. The vertical linear wounds may be broken into multiple Z plasties in order to improve the scar. If the laceration in the upper lid extends upward to involve the eyebrow, it is essential to align the eyebrow first.

Fig 3 Simple laceration
Deep lacerations
Deep nonmarginal lacerations require careful layer by layer inspection of the wound to assess the integrity of the orbital septum, levator aponeurosis, rectus muscles, and globe. It requires careful closure in layers. (Fig 4). Subcutaneous closure is done with 5’0 vicryl.

Fig 4. Deep laceration - Subcutaneous closure done with 5’0 vicryl.
REPAIR OF LID MARGIN LACERATION
(i) With minimal loss of tissue:
Repair of marginal injuries can be difficult due to swelling. The lid margins should be freshened if devitalized tissue is present, to form straight, smooth surgical edges, sacrificing, as little tarsus as possible. Meticulous closure of eyelid margin is crucial. Inadequate closure can lead to lid notching, lagophthalmos and exposure keratopathy. The margin is repaired using the three-suture technique.
Lid margin sutures are passed first. A 6-0 silk suture is passed through the grey line 3 mm from the edge of the tear, to a depth of 3mm. This is brought out of the wound and reinserted into the other side of the laceration 3 mm deep to the lid margin and emerging through the grey line 3 mm from the edge of the wound (Fig 5a). The same suture is then passed back into the grey line on the same side, 1 mm from the edge of the tear, to a depth of 1 mm (Fig 5b). The needle is brought out and reinserted into the opposite edge of the tear 1 mm deep to lid margins and emerging through the grey line 1 mm from the margin of the wound. Two more vertical mattress sutures are passed exactly in the same way through the posterior lash line and the other posterior to the gray line. These three sutures are triply tied and ends left long (Fig 5c).5,0 polyglactin sutures are used to reaproximate the tarsus. There is no need to place sutures on the conjunctival surface since it will heal with the approximated tarsal edges. Skin sutures are removed in 5 to 7 days . Lid margin sutures are left in situ for 10-14 days.
Undue tension should be avoided on the marginal laceration as this may lead to wound dehiscence. Whenever there is tension on the wound, one can use the sliding or advancement flaps.
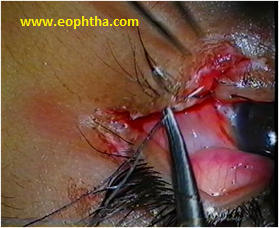
Fig 5a- A 6-0 silk suture is passed through the grey line 3 mm from the edge of the tear, to a depth of 3mm and is being reinserted into the other side of the laceration 3 mm deep to the lid margin.
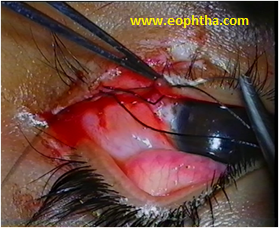
Fig 5 b- The suture is then passed back into the grey line on the same side, 1 mm from the edge of the tear, to a depth of 1 mm
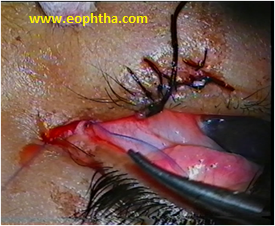
Fig 5 c – Three marginal sutures are passed and ends are left long
(ii) With moderate loss of tissue :(From one fourth to one half of eyelid).
When there is moderate loss of tissue with involvement of one-fourth to one-half of the eyelid horizontal relaxation of the eyelid is required. This can be achieved by lateral canthotomy and canthloysis of either the upper or lower limb of the lateral canthal tendon, depending on the eyelid involved. 5’0 prolene suture is used to fixate tarsus to the lateral rim periosteum. Subcutaneus closure is done with 5’0 vicryl.
In case the defect is too large to be closed with canthotomy and cantholysis a tenzel semicircular flap can be raised. For upper lid defect, the arc of the semicircle is downwards and for the lower lid the arc is above the canthus. Surgeon may also use transconjunctival flap, or free transconjunctival graft or Mustarde's marginal pedicle rotation flap for reconstruction.
(iii) With severe loss of tissue (more than half of eyelid)
For very large defects grafts from the opposite eyelid or surrounding tissue are used for repair. The commonly used techniques are Cutler Beard procedure, Hughe’s tarso conjunctival advancement flap, Mustarde's cheek rotation flap or Free transconjunctival graft and mucocutaneous advancement.
TRAUMA TO LEVATOR MUSCLE OR APONEUROSIS
Patient presenting with ptosis should be observed for atleast six months as spontaneous resolution may occur with time.Whenever, the orbital fat is exposed, it indicates disruption of the orbital septum and the wound should be adequately explored (Fig 6). The levator palpebrae superioris (LPS) fibers are identified by their vertical orientation, in comparison with the Orbicularis muscle fibres, which run circumferentially. If the aponeurosis has been disinserted from the tarsus, the cut edge is drawn forwards and reinserted by placing three 5-0 double arm vicryl sutures through the tarsus. Both arms of the suture are then passed through the aponeurosis. If surgery is being performed under local anesthesia, the level of aponeurosis can be adjusted by having the patient look in the straight-ahead gaze. If the orbital septum has been opened due to injury, it should not be sutured since this could result in lagophthalmos. If the laceration is at the level of the lid fold, the eyelid crease is recreated by placing 2-3 sutures. The sutures are passed through the skin muscle layer and include a superficial bite of the levator aponeurosis with 6'0 silk or separately with 5'0 vicryl.

Fig 6 - Full thickness upper lid defect with exposed orbital septum with injury to the levator aponeurosis
INJURIES INVOLVING LATERAL CANTHUS
If the lateral canthal tendon (LCT) is found to be severed, it is repaired by passing 4-0 non-absorbable prolene mattress sutures through both ends which should be anchored to the periorbita on the inner aspect of the lateral orbital tubercle (Whitnall's tubercle).( Fig 7). One should aim for overcorrection as the healing tends to shift the canthus inferiorly.

Fig 7 Injury to the lateral canthus
INJURIES INVOLVING MEDIAL CANTHUS:
Avulsion of the lid at the medial canthus mostly involves the lower lid. Medial canthal injuries are usually associated with canalicular injury (Fig 8). Intubation of the canaliculus should be performed prior to canthal repair. The surgeon should assess whether the anterior or posterior limb is avulsed. Repair of the posterior limb is more critical to achieve proper lid positioning.
One should assess whether there is soft tissue injury alone or bone is also fractured. In case of soft tissue injury, if both ends are visualised, the distal cut end is identified and sutured to its proximal part. If the proximal portion is not identified , then the horizontal mattress suture is passed through the distal avulsed end and then the needle is passed through the periorbita in the region of posterior lacrimal crest. with 4-0 prolene suture. If there is no periorbita, then microplating is used to fixate medial canthal tendon. This ensures it is anchored adequately, so that the puncta are turned inwards and ectropion does not result. In case of fracture, it is important to stabilize the fracture and then fixation or transnasal wiring can be performed to repair medial canthal tendon.

Fig. 8 Injury to medial canthus.
MANAGEMENT OF CANALICULAR LACERATION
Avulsion of lid at the medial canthus or lacerations in this region will result in complete severance of the canaliculi. Various techniques of surgical repair of canalicular lacerations have been described in the past by various authors. The basic principle in the repair of the lacerated canaliculus is reestablishing of the drainage function. The development of fine sutures, refinement in surgical technique and the use of the microscope have contributed to a better prognosis.
Stents:
Monocanalicular or bicanalicular stenting may be done. Monocanalicular have the advantage of not disturbing the normal canaliculus. Silicone is the most commonly used material. Mini-Manoka stent is one of the options. However to overcome the cost factor and difficult availability we have been using an alternative technique.
The first step is to identify the two cut ends of the canaliculi. The lateral cut end is identified by passing a lacrimal probe through the punctum ( Fig 9a). To identify the medial cut end, the wound is examined under magnification, preferably an operating microscope. The tiny opening of the cut canaliculus is rather paler than the surrounding tissues. However, if the cut end is not obvious, it is identified by pooling sterile saline in the wound and then watching for bubbles while injecting air from the upper canaliculus. The use of a pigtail probe to identify the medial end of the lacerated canaliculus should be avoided because of the risk of creating false passages and trauma to the intact canaliculus.
Once the 2 cut ends are identified, a mini-manoka tubing or a 22gauge cannula (venflon) sleeve after removing the sharp tip of the stillete is introduced upto the medial sac wall (Fig 9b). Four pericanalicular bites are then taken with 8-0 vicryl or nylon sutures, two posterior and two anterior.
The lid margin wound is closed by the technique of marginal repair, as described. It is of paramount importance that the MCT should be repaired when it has been disrupted. The silicone tubing or sleeve is left in place for at least 3 months.
When not using a mini-manoka stent, one of the commonest problems encountered is extrusion of the tube from the intubated canaliculus. To retain a monocanalicular stent, fixation sutures (double arm) are passed through the tube and eyelid skin over a peg. These sutures are then carried subcutaneously upwards and medially and tied again over a peg (Fig 9c). These sutures provide an upward and inward traction to the tube preventing its extrusion. Alternatively, to aid in its retention, the silicone tubes may be passed into the nose by using Quickert- Dryden probing system wherein the silicone tube is fixed to a malleable probe which is passed into the inferior meatus through nasolacrirnal duct and recovered from there. The other end of the tube is also passed into the nose from the opposite punctum (bicanalicular intubation). This ensures retention of the probe for the required period of time.

Fig 9a- Lacrimal probe is passed through the cut ends of the lower canaliculus

Fig 9b- A 22G intracath cannula with sharp end of the needle removed,is passed through cut ends of the canaliculus into medial sac wall

Fig 9c- Fixation of tube by passing double arm prolene through the tube and then through the skin and emerging towards the medial canthus and fixed to the polythene bolster
TOTAL AVULSION OF EYELID
In this condition avulsed segments should be found and the avulsed tissue placed in a sterile container containing antibiotic solution and stored in a refrigerator until it can be surgically reimplanted.
Conclusion:
Adequate primary repair of the lid injury gives the most satisfactory results and meticulous repair is mandatory for lid injuries. However where it becomes necessary, a secondary repair gives reasonably good correction, both functional and cosmetic.
REFERENCES
- Crowford JS: Lacrimal intubation seet with suture in the lumen , Ophthal Plast Reconstr Surgery 1988, 4:249
- Goldberg MF, Tessler HH: Occult intra ocular perforations from brow and lid lacerations, Arch ophthalmol 1971:86,145.
- Gossaman DM, Berlin JA : Management of acute adenexal trauma . In surgery of eye lid , orbit and lacrimal systems . American Acad Ophthalmol, 1993
- Grover AK , Kaur S Principles of Oculoplastic Surgery : CME Series No.5, Editor AK Grover.
- Grover A.K. and Bhatnagar A.; Trauma to Eyelids, Canalicular lacerations and its management. J.K.S.O.S. (April-June 1991), Vol.3 No.2:135-146.
- Gupta VP: Basic Principles of eye lid reconstruction: CME Series No.5, Editor AK Grover.
- Loft HJ.Wobig JL. Daily RA. The bubble test: an atraumaticmethod for canalicular laceration repair. Ophthalmic Plastic and Reconstructive Surg 1996;12;61-64.
- Levine MR, Buckmn G: Semicercular flap revisited.Arch Ophthalmology, 1986: 104,915-17.
- Long JA. A method of monocanalicular silicone intubation. Ophthalmic Surg 1988 19 204 205
- McLeish WM Bowman B, Anderson RL The pigtail probe protected by silicone intubation a combined approach to cana icu ar reconstruction. Ophthalmic Surg 1992;23:281-283.
- Mustarde JC: Repair and Reconstruction in the Orbital Region. Edinburgh: Churchill Living stone: 1971, chap 7-8.
- Reifler DM. Management of canalicular laceration. Surv Ophthalmol 1991,36:11
- Ritleng, Peirre. A simplifed technique for lacrimal intubation. Ocular surgery news. Vol 14, No 7
- Tenzel RR: Reconstruction of the central one half of an eyelid. Arch Ophthalmol 1975: 93: 125-126.Grover AK, Kaur S Principles of Oculoplastic Surgery: CME Series No.5, Editor AK Grover.
- Fezza JP. Plast Reconstr Surg 2008 Mar 121(3): 1009-14.3
- Caviggioli F, Klinger F, Villani F, Fossati C, Vinci V, Klinger M. Aesthetic Plast Surg. 2008 May;32(3):555-7.
- Conlon MR, Smith KO, Cadera W, Shun D, Allen LH. An Animal model studying construction techniques and histopathologic changes in repair of canalicular lacerations. Can J Ophthalmol 1994:29:3d
- Committee on Trauma of the American College of Surgeons : Advanced trauma life support course , Chicago , 1984, Amercian College of Surgeons .

