Posterior Polar Cataract is associated with remnants of Tunica vasculosa lentis. (1) It presents as a white opacity situated on the posterior capsule appearing as a circular plaque with concentric whorls. (2) Surgical management of posterior polar cataracts is a challenge even for skilled surgeons due to high risk of posterior capsular rupture and vitreous loss during surgery. (3)
1. Preoperative Considerations:
- It has to be identified correctly on slit lamp examination – with its characteristic onion peel or bull’s eye appearance.
- Patient has to be counselled regarding increased surgical time, higher chances of posterior capsular rupture and even the possibility of posterior segment intervention and delayed visual recovery. (3,4)
- The fellow eye also needs to be evaluated.
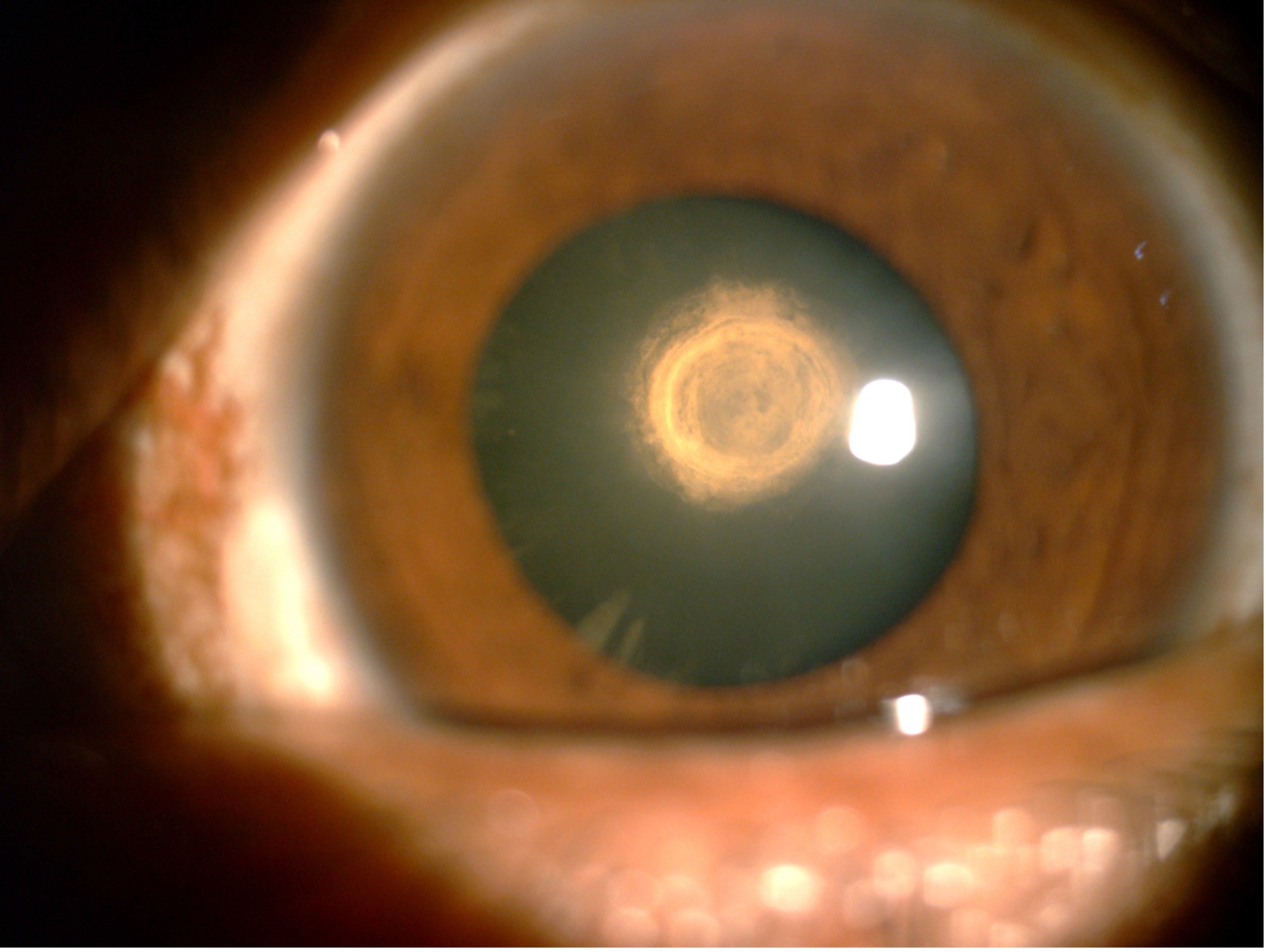
Image showing: Characteristic onion peel appearance of Posterior Polar Cataract (Courtesy of Rajan Eye Care Hospital).
2. The Preferred Anaesthesia:
- Peribulbar anaesthesia is preferred because of longer surgical time and thereby giving more comfort to the patient.
- Topical anaesthesia can be used with increasing experience with cataract surgery. It is necessary to be more cautious in case of topical anaesthesia as the patient can move their eye increasing the risk of forward movement of iris lens diaphragm. (3)
3. Adequate Capsulorhexis:
- The size of capsulorhexis should not be too small or too large. An adequate CCC of 4.5-5mm size is the preferred choice.
- Smaller CCC might increase the hydrostatic pressure in the capsular bag during hydrodelineation and increase the chance of a capsular bag rupture.
- A larger CCC may not leave adequate support for a sulcus-fixated IOL if the posterior capsule is deficient. (4,5)
4.Avoid Hydrodissection:
- Hydrodissection causes undue pressure on the posterior capsule and subsequent rupture of the capsular bag. (4)
- It is contraindicated in PPC especially if there is a pre-existing posterior capsule defect.
- Hydrodelineation is the preferred procedure, as it tries to separate the inner layers from the outer ones.
- Inside-out delineation is easy to perform, provides excellent surgical control, reduces stress on the zonules and delineates the central core of the nucleus.
- A golden ring within the lens should be looked for which indicates successful delineation. (6)

Image showing: Golden ring, sign of Hydrodelineation. (Courtesy of Rajan Eye Care Hospital)
5. Do notAttempt to Rotate the Nucleus:
- Avoid rotation of the nucleus as this can increase the risk of posterior capsule rupture. (6)
- The techniques should be aimed towards removing the nucleus while it is cushioned by the epinucleus.
6. Technique of nucleus management:
- Partial segmentation technique is where the central nucleus is emulsified first and then each layer of the epinucleus is aspirated layer by layer.
- The cortical matter is also gradually aspirated till the central area of PPC is reached.
- This mechanical separation of the cortex from the central PPC avoids traction, thereby minimizing the stress on the posterior capsule.
- Epinucleus and cortex can be removed using manual dry aspiration. (6)
- Aim for slow motion phaco with low vacuum, low aspiration rate and low inflow parameters to maintain a stable AC.
- The low infusion drives less fluid around the lens.
7. Inject Viscoelastic before Retracting Any Instrument from the Eye:
- Injecting viscoelastic from the side port before removing the phaco or I&A probe from the eye helps to keep the anterior chamber well-formed and prevents forward bulging of the posterior capsule throughout the surgery.
- A stable AC is preferred throughout the surgery and any major fluctuations should be avoided.
8. In case of PC rupture:
- The chamber should be filled with a dispersive viscoelastic to coat the posterior capsule rent as this prevents the vitreous from coming into the anterior chamber. (6)
9. Bimanual Automated I&A and Automated Vitrectomy:
- The infusion bottle height should be lowered and a bimanual vitrectomy with or without triamcinolone should be performed with high cut rate and low vacuum.
- A bimanual I&A is done for removing any residual cortex. (6)
10. IOL Implantation
- In case of a pre-existing PC tear, the eye is evaluated pre-operatively regarding capsular support and placement of IOL. IOL can be implanted in the bag if P-CCC is performed. (6)
- In case of a large rent, a 3 piece hydrophobic IOL can be implanted with optic capture done to stabilize the IOL and reduce contact of optic with the iris.
Good surgical outcomes can be obtained in a posterior polar cataract by adhering to these ten pearls.
References
- Lee MW, Lee YC. Phacoemulsification of posterior polar cataracts--a surgical challenge. Br J Ophthalmol. 2003;87(11):1426-1427. doi:10.1136/bjo.87.11.1426-a
- Duke-Elder S. Posterior polar cataract. In: Duke-Elder S (ed). System of Ophthalmology, Vol. 3, part 2: Normal and Abnormal Development, Congenital Deformities. Mosby: St Louis, MO, 1964, pp 723–726.
- Osher RH, Yu BC-Y, Koch DD. Posterior polar cataracts: a predisposition to intraoperative posterior capsule rupture. J Cataract Refract Surg 1990; 16: 157–162.
- Vasavada A.R., Singh R. Phacoemulsification with posterior polar cataract. J Cataract Refract Surg. 1999;25:238–245.
- Fine I.H., Packer M., Hoffman R.S. Management of posterior polar cataract. J Cataract Refract Surg. 2003;29:16–19.
- Vasavada AR, Vasavada VA, Raj SM. Approaches to a posterior polar cataract. Saudi J Ophthalmol. 2012;26(1):51-54. doi:10.1016/j.sjopt.2011.11.006


