Introduction
Allergic eye disease (AED) is a common problem, owing to the fact that the eye is the first organ to encounter environmental allergens. It has been reported to affect 20% of the population worldwide1, 2. Allergic eye disease is found to be on the rise in line with other atopic diseases like asthma, due to environmental reasons.
Classification of Allergic Eye Diseases1, 4
1.Allergic conjunctivitis
Acute allergic conjunctivitis
-
Seasonal allergic conjunctivitis
-
Toxic induced (acute contact with irritant)
Chronic allergic conjunctivitis
-
Perennial allergic conjunctivitis
-
Toxic induced (long standing)
2.Contact dermatoblepharitis
3.Vernal keratoconjunctivitis
4.Atopic keratoconjunctivitis
5.Giant papillary conjunctivitis
6.Microbial allergic conjunctivitis
- Staphylococcal blepharoconjunctivitis
- Phylectenular keratoconjunctivitis
- Splendore Hoeppli phenomenon (allergic granulomatous Nodules)
Immunopathology in allergic eye disease 3, 5
The ocular surface exhibits a variety of immunologic responses which result in conjunctival /corneal inflammation. In the Gell and Coombs classification system, 5 classes of hypersensitivity reactions are recognized. Of these, Type I and Type IV reactions are of significance in AEDs.
Type I (immediate) hypersensitivity reaction2 occurs when a sensitized individual comes in contact with a specific antigen. Immunoglobulin E (IgE) has a strong affinity for mast cells. The cross-linking of 2 adjacent IgE molecules by the antigen triggers mast cell degranulation. This causes release of preformed and newly formed mediators of the inflammatory cascade. These with various chemotactic factors, cause increased vascular permeability and migration of eosinophils and neutrophils. The principal ocular type I hypersensitivity reaction occurs in allergic conjunctivitis (SAC, PAC)
Type IV (delayed /CMI) hypersensitivity reaction is mediated by T lymphocytes. It occurs 48 hours after allergen challenge. Type IV hypersensitivity reactions imply immunocompetence on the part of the individual, since an intact immune system is required to mount the cell-mediated response. Ocular examples of type IV hypersensitivity include phlyctenular keratoconjunctivitis, AKC, VKC, corneal allograft rejection, contact dermatitis, and drug allergies
Cascade of events in allergic conjunctivitis:
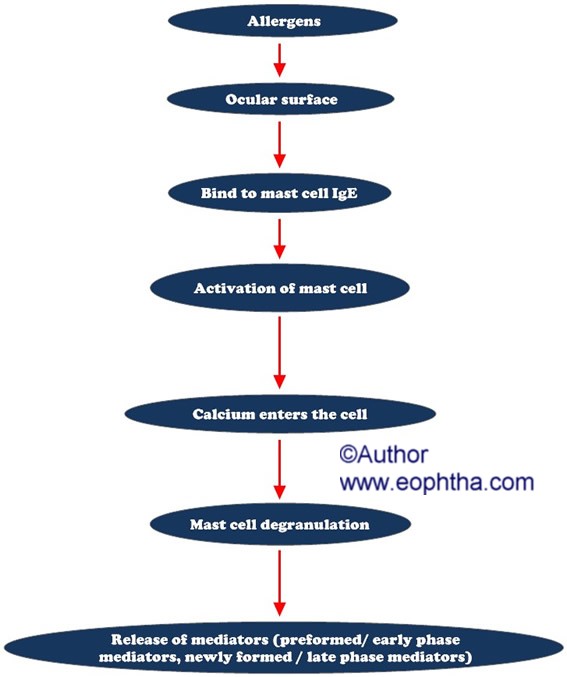
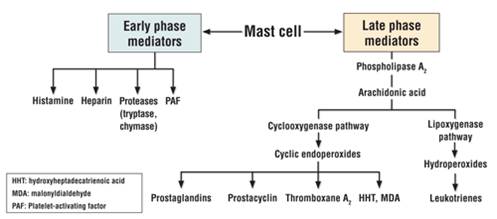
Preformed mediatorslike histamine, tryptase, protease cause itching, redness, swelling, degradation of neighbouring cells, and inflammatory cell accumulation.Newly formed mediatorslike prostaglandins, leukotrienes, platelet-activating factor, cytokines and chemokines also mediate redness, swelling, infiltration of eosinophils and neutrophils.
Some cases of ocular allergy cannot be explained by mast cell degranulation alone, especially chronic responses. This suggests mediators from other cells like basophils, eosinophils and neutrophils trigger and perpetuate inflammatory response. Type IV hypersensitivity reactions (delayed allergic reactions) occur hours after allergen challenge and mast cell activation. VKC and AKC are mediated by a combination of type I and type IV hypersensitive reactions.
Activatedeosinophilsrelease highly charged polypeptides including: Major basic protein (MBP), Eosinophil cationic protein (ECP), Eosinophil derived neurotoxin (EPX), eosinophil peroxidase (EPO).ECP and MBP are epitheliotoxic and are involved in corneal damage that occurs in severe allergy. Tear levels of ECP and EPX are correlated with clinical signs and symptoms of allergic disease and are considered local markers of eosinphil activation.
Although the role ofneutrophilsin allergic disorders is not clear, they release inflammatory mediators like leukotrienes, PAF and cytokines. Tear level myeloperoxidase (MPO), a neutrophil activating marker is increased in allergic conjunctivitis
One important process responsible for allergic inflammation is the production ofcytokines 5, 6by T lymphocytes. CD4-T cells are the predominant cells in inflamed conjunctiva. T cells are divided into two subsets (Th1 and Th2) on basis of their cytokine profile.Th1cells produce IL2 and interferon gamma (INF-g). Th2 cells produce IL3, IL4, and IL5.Th2 cells predominate in allergic inflamed tissues.
An increase in Th2 cytokine (IL4, IL5, and IL3) has been demonstrated in SAC, VKC and AKC. Compared to SAC, VKC has an over expression of these cytokines in addition to other mechanisms. In AKC and GPC in addition to Th2 cytokines, increase of Th1 cytokines (IL2 and INF-g) is found suggesting cell mediated hypersensitivity in severe atopic conditions
Features |
VKC |
AKC |
|
Age of onset |
Childhood/teens |
20-50 years |
|
Duration |
Resolves in mid-late teens |
Resolves by 50 years |
|
Seasonal variation |
Markedly worse in spring |
Variable, worse in winter |
|
Conjunctival papillae |
GPC, mainly upper lid |
Small/medium, mainly lower lid |
|
Conjunctival scarring |
Uncommon |
Symblepharon common |
|
Skin |
Uncommon |
Often* |
|
Eosinophils |
Numerous |
Less and less often degranulated |
|
Corneal involvement |
Less extensive |
More extensive* |
|
Cataract |
Uncommon |
Common, ASCC / PSCC |
*Periorbital changes secondary to chronic eye rubbing (Dennie Morgan lines) and Hertoghe sign (absence of lateral eyebrows) are found in AKC.*Higher incidence of keratoconus (16%) and recurrent herpes simplex keratitis associated with AKC.
Diagnostic approaches in AED 3
Diagnosis is usually based on anaccuratehistoryand a properClinical examination, especially in cases of SAC, PAC, AKC, VKC, GPC and contact blepharoconjunctivitis.
Some pseudo-allergic clinical forms like tear film dysfunction, mechanical /toxic conjunctivitis, sub-acute and chronic infections may mimic allergy. In such situations, clinical examination needs to be substantiated with laboratory diagnostic methods.
A. Skin Tests 3
Skin prick test:It consists of application of the suspected allergen (pollen, mites, and animal dander) to the flexor aspect of the forearm and pricking with a needle. This provides evidence of specific sensitivity to food and environmental allergens. This is highly sensitive for systemic allergies but not specific for ocular allergies. It requires the support of other tests.
Patch Test:It consists of application of hapten containing cellulose discs to the back and assessing the reaction after 48 hours. It must be remembered that back skin is thicker and is less exposed to environment. It is possible that the thin consistency and sun exposure exacerbates the specific and nonspecific hyper responsiveness of the eyelid skin.
B. Invitro Assays
Assessment of specific IgEin the serum is indicated and preferred in some cases especially children. It must be remembered that AKC & VKC are not always associated with specific allergic sensitization. In VKC 50% of patients are not associated with IgE sensitization. A normal value does not exclude allergy and high values can occur in conditions other than atopy.
Eosinophilia(>500 cells/ml) is not found in SAC, PAC and GPC but present in AKC & VKC.
Eosinophilic Cationic Protein(ECP) is significantly elevated in active allergy and needs systemic therapy even in cases of exclusively ophthalmic sensitization.

Trantas Dots in VKC
C. Local Tests
Conjunctival Provocation Tests(CPT):This consists of the application of a standardized allergen to the eye every 15 minutes until a moderate reaction is observed. The response subsides after 20 minutes. Sometimes the late reactions can occur. It helps to identify the specific allergen and helps in avoiding/eliminating the same. However, the rare risk of anaphylaxis and bronchospasm has to be kept in mind and therefore performed only in specialized centers and only when necessary.
Specific IgE in tears:In non-allergic patients, specific IgE is usually nondetectable. Detection may be of value in cases where ocular allergy is suspected, in the presence of negative systemic tests. However, difficulties in collecting the tear sample (50µl), absence of standardized reference parameters for tear IgE measurement have led to a preference for provocation tests.
Total IgE in tears:3 Normal tear levels of IgE are very low (3ng/ml). Detectable levels of IgE are diagnostic of allergic conjunctivitis. This has been made simple due to the commercial availability of Lacrytest strips (similar to Schirmer strips), which are placed in the lower fornix. Due to the presence of anti-IgE antibodies and calorimetric system, change in color intensity gives a semi-quantitative result of total IgE. This test is found to correlate well with CPT but poorly with skin tests, proving that local sensitization may occur.
Tear film cytology:The presence of even a single eosinophil in tears is said to be diagnostic of allergy.
Conjunctival scraping:Done with a spatula provides more cells than tear film cytology. This also helps in differentiating from Chlamydial and viral conjunctivitis when needed.
Conjunctival biopsy: Conjunctival biopsy will show increased infiltration with mast cells, eosinophils, and chorion (absent from the normal conjunctiva.) will help differentiate AKC from autoimmune fibrosing conjunctivitis.
Tear film mediators:3, 5, 6Quantitative analyses of inflammatory mediators in the tear film have been used as a disease marker, to understand immune mechanisms and to identify therapeutic targets. Elevated tear film histamine levels (normal 10ng/ml) and tryptase levels provide an indication of mast cell degranulation and activity respectively, especially after CPT or VKC exacerbations. They are mainly used to study the effects of mast cell stabilizers than for diagnosis. Tear levels of ECP (a marker of eosinophil activation) is found to be elevated in all forms of allergic conjunctivitis especially with corneal involvement. Determination of tear cytokine/ chemokines provides insight into the allergic pathophysiology. Disadvantages of these methods include difficulty in obtaining / inadequacy of tear samples
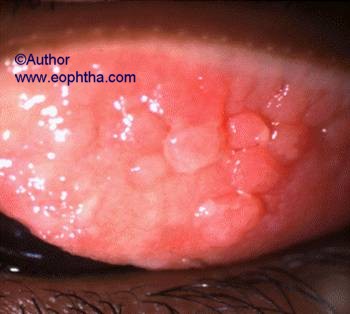
Figure: Cobblestone papillae in VKC
D. Confocal microscopy7
Confocal microscopy is useful in elucidating alterations in corneal morphology in allergic keratoconjunctivitis. Corneal disease in AKC is associated with alterations in the basal epithelium and subbasal corneal corneal nerves, which relate to changes in, tear function and corneal sensitivity. A decrease in number and density of subbasal long nerve fibres accounting for the decreased corneal sensation is seen in AKC. Corneal nerves are thickened (edema and increased metabolism) associated with bifurcation abnormalities indicates stromal remodeling in response to chronic inflammation. Corneal nerves have neuropeptides and neurotransmitters which exert a trophic effect on the epithelium. Altered expressions of these are found in VKC. Inflammatory cells and activated keratocytes are found in the superficial stroma in AKC and VKC.
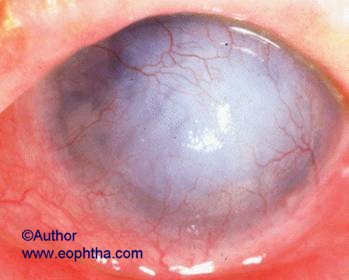
Corneal vascularisation in AKC

Lid involvement in AKC

Giant Papillary Conjunctivitis

Shield ulcer in VKC
Treatment of ocular allergy
Current therapy of ocular allergy involves elimination of the offending allergen, modulation of the immune system, and pharmacologic inhibition of the chemical mediators.
A. Nonpharmacological Interventions
-
Avoidance of allergens remains the first step. This may involve environmental adjustments, from removing the source of the allergen to changing the occupation.
-
Cold compresses and refrigerated ocular medications provide symptomatic relief, especially itching.
-
Lubrication with preservative free drops help remove / dilute allergens
-
Use of daily disposable contact lenses with proper cleaning and disinfecting techniques is recommended. Patients with seasonal allergy should avoid contact lenses during seasonal flare ups.
B. Pharmacological interventions13
The most common allergic diseases, SAC and PAC are classically IgE mediated and therapeutic focus is confined to suppression of mast cell degranulation and their mediators like histamine. Conversely, chronic diseases like AKC and VKC are both IgE mediated and cell mediated and suppression of mast cell mediators is not sufficient. Severe disease needs use of potent drugs; complex treatment regimens and long term follow up. None of the available drugs cover all therapeutic requirements for all allergic eye diseases.
| Class |
Drugs |
Properties & Indications |
Comments |
|
Decongestant/ Antihistamine Combinations |
Naphazoline 0.025%/ Pheniramine 0.3% |
Vasoconstrictors |
Short duration of action |
|
Anti-histaminics* |
Levocabastine |
Vasoconstrictors |
Short duration of action |
|
Mast cell stabilizers* |
Chromolyn |
Prevent secretion of mast cell granules. |
Slow onset of action |
|
Mast cell stabilizer/Antihistaminics (dual action) |
Azelastine |
Rapid onset of action |
Bitter taste (Azelastine) |
|
Steroids* |
Loteprednol |
Block arachidonic* acid pathway |
No mast cell stabilization |
Table 1: Topical Ocular allergy Medications 2, 3, 4, 8
H1 receptor stimulation mediates pruritis and H2 receptor mediates vasodilatation. Nonspecific antihistaminics* block histamine and muscarinic receptors thereby causing mydriasis and angle closure. Vasoconstrictors are not used as they are nonspecific and do not have any effect on the allergic cascade
Mast cell inhibitors* aid in phosphorylation of a 78,000-d protein that terminates secretion of mast cell granules; increase calcium influx into the cell preventing membrane changes; reduce membrane fluidity prior to mast cell degranulation.The result is a decrease in degranulation of mast cells, thereby preventing release of histamine and other chemotactic factors. Lodoxamide was found to be 2500 times more effective as it reduces tear ECP levels in contrast to sodium chromoglycate. Tear Eosinophilic Cationic Protein (ECP) has been shown to be a marker for eosinophil activation in ocular allergy.
Nonsteroidal anti-inflammatory drugs (NSAIDs) act on the cyclooxygenase pathway and inhibit production of prostaglandins and thromboxanes. They do not block lipoxygenase pathway. Common NSAID approved for allergy treatment is ketorolac tromethamine.
Corticosteroids* act at the first step of the arachidonic acid pathway. They inhibit phospholipase, which converts membrane phospholipids into arachidonic acid. By preventing formation of arachidonic acid, corticosteroids block both cyclooxygenase and lipoxygenase pathways, in contrast to NSAIDs, which act only on the cyclooxygenase pathway.
C. Topical nonocular pharmacological treatment
Recent reports show a promising effect of intranasal corticosteroids13 in allergic rhino conjunctivitis. Intranasal steroids with low systemic bioavailability especially mometasone furoate and fluticasone furoate control the nasal-ocular reflex component in SAC and PAC. They do not carry the risk of causing cataract or elevated intraocular pressure.
D. Immunomodulators / Immunosuppressives3, 13
Reports have shown the clinical usefulness of immunomodulators like topical 2% cyclosporine 3, 9, 10 in severe chronic conditions (AKC, VKC), especially during acute exacerbations. Their steroid sparing effect is beneficial in cases requiring long term steroids. Topical use 0.5%13 cyclosporine showed no significant benefit. Topical Tacrolimus3 (0.9%) ointment has been found to be useful in atopic lid disease. This immunomodulator has a similar mechanism of action to cyclosporine.
E.Immunotherapy2
Immunotherapy in allergic eye diseases is aimed at inducing host tolerance of the allergen. It has been tried since 1911 but the results are found to be inconsistent. It consists of identifying the allergen by skin tests. Hyposensitisation consists of repeated administration of the allergen at gradually increasing doses either by systemic (subcutaneous / sublingual) route or topical (conjunctival) route. Hyposensitisation by the subconjunctival route is found to be ineffective and systemic administration carries the risk of anaphylactic shock. Some of the allergens are polymerized with gluteraldehyde or polyethylene glycol to avoid the risk of anaphylactic shock. The mechanisms by which immunotherapy work include:
-
Increases IgG which competes with IgE and prevent it from binding to the mast cell IgE
-
Transforms the Th2 lymphocytes (which stimulate IgE production) into Th1 lymphocytes
-
Acts on T lymphocytes, monocytes and platelets thereby inhibiting production of mediators favoring histamine release
Though found effective in rhino conjunctivitis associated with weed / grass pollen, results of immunotherapy in allergic conjunctivitis are inconsistent.
Treatment in specific conditions
A. Giant papillary conjunctivitis 1, 2 (GPC):Goals of treatment include resolution of symptoms and restoration of functional use of contact lenses or ocular prosthetics. Removal of the responsible foreign body is the definitive treatment. Fortunately, contact lens need not be completely discontinued to minimize the symptoms of GPC. Changing contact lens care routine, use of disinfecting solutions without chemical preservatives and switching to disposable or daily-disposable soft contact lenses avoid accumulation of protein deposits. Rigid gas permeable contact lenses may provide further relief due to decreased tendency to develop adherent deposits and coatings. Pharmacologic treatment of GPC includes the use of mast cell stabilizers, topical corticosteroids and antihistamines.
B. Vernal keratoconjunctivitis (VKC):Preventive measures include relocation to cooler climates if possible and avoiding exposure to nonspecific triggering factors such as sun, wind, and salt water. Pharmacologic treatment of VKC includes the use of mast cell stabilizers, antihistamines, topical corticosteroid pulses during exacerbations. Preservative free lubricants and cold compresses provide symptomatic relief. Mucolytic agents (10% Acetylcysteine) are useful in cases with severe mucoid deposits. The clinical benefit 3, 9 and steroid sparing effect of Cyclosporine 2% eye drops have been reported.
Severe cases of shield ulcer with fibrin deposits / plaques require superficial keratectomy or excimer laser phototherapeutic keratectomy (PTK) to promote epithelial regeneration. Other surgical procedures, such as cryoablation or surgical removal of papillae with mucosal grafting, may be needed in extremely advanced cases.
C. Atopic keratoconjunctivitivs (AKC):The lids are involved and need intensive treatment, in addition to pharmacologic measures like mast cell stabilizers, antihistamines and topical corticosteroid pulses. The lid disease is treated with oxytetracyline 250mg once or twice a day, or doxcycline 100mg once daily. Frequent lubrication with preservative free tears is essential to treat associated tear film dysfunction. The possibility of recurrent herpes simplex keratitis will need topical or systemic antiviral therapy. In some situations, more aggressive or steroid-sparing treatment may be indicated.
Topical 2% cyclosporine 3, 10used 4-6 times per day is proven effective for exacerbations and is considered as an adjunct or alternate therapy in situations where steroid use needs to be minimized. Systemic cyclosporine (5 mg/kg/d) is shown to be useful in inducing remission. Low-dose maintenance therapy (5 mg/kg q5d) may be required in refractory cases. Topical Tacrolimus (0.1% ointment), a T lymphocyte immunomodulator is reported to be useful in atopic lid disease.
PKP may be undertaken in cases of severe corneal scarring or thinning, but great attention to control ocular surface inflammation and tear film dysfunction is required. Surgical procedures for the lids and cataract surgery may be needed in some cases
Plasmapheresis 3 has been suggested as a successful adjunct therapy for patients with high IgE levels.
Novel Therapeutic Approaches
Recent reviews have described alternative medicines 12 in treating chronic inflammatory disorders like asthma and atopic dermatitis. These usually are herbs, phytochemical and vitamins. Their mechanisms of action involve the suppression of the Th2 cytokine pathway or inhibition of mast cell components.
Probiotics such as Lactobacilli 11 have been studied in VKC due to their anti-inflammatory properties. These microorganisms form a part of the conjunctival micro flora in humans. Lovienoet al.administered a probiotic eye drop consisting ofLactobacillus Acidophilusto seven patients with mild to moderate VKC. 4 weeks after treatment, significant improvement in signs and symptoms was observed in 6 patients. It was also demonstrated that ICAM-1 expression on epithelial cells was down regulated, supporting their anti-inflammatory effect. This could present an opportunity to treat moderate forms of chronic allergic disease effectively and safely.
Pearls
-
Allergic conjunctivitis is not a single disease.
-
IgE and mast cell mediated responses are initial events
-
Th2 cell play a central role in chronic allergic diseases
-
Accurate history is essential; if it does not itch, it is not allergy
-
Diagnosis is usually clinical; Chronic forms need lab diagnosis
-
Cornea is never involved in SAC & PAC
-
Perform skin tests
-
If systemic tests are negative, do local tests
-
CPT proves local hypersensitivity
-
Low tear volumes make tear analysis impractical.
-
Tear total IgE level assessment is easy, not specific
-
Dual action drugs are the first line therapy in ocular allergy
-
Avoid vasoconstrictors; Avoid steroid abuse
-
Tear film dysfunction may simulate or overlap allergy
-
Avoiding allergen and nonpharmacological measures are important
-
Patient education and awareness is essential
Abbreviations
AED- Allergic Eye Disease
AKC- Atopic KeratoConjunctivitis
CMI- Cell Mediated Immunity
CPT- Conjunctival Provocation Tests
ECP- Eosinophil Cationic Protein
EPX- Eosinophil Derived Neurotoxin
EPO- Eosinophil Peroxidase
GPC- Giant Papillary Conjunctivitis
IgE- Immunoglobulin E
IL- Interleukin
MBP- Major Basic Protein
PAC- Perennial Allergic Conjunctivitis
SAC- Seasonal Allergic Conjunctivitis
VKC- Vernal KeratoConjunctivitis
References
- Cornea and external disease: progress III by Thomas Reinhard
- Inflammatory diseases of the conjunctiva by Thanh Hoang-Xuan
- Uveitis and Immunological Diseases by Uwe Pleyer, Stephen C Foster
- Friedlander MH., Conjunctivitis of allergic origin: Clinical presentation and differential diagnosis. Survey of ophthalmology 1993:38; 105-114
- Immune Mechanisms in Allergic Eye Diseases: What is New? Ifeoma Offiah; Virginia L. Calder Curr Opin Allergy Clin Immunol.2009; 9(5):477-481.©2009
- Leonardi A et al., Multiple cytokines in human tear specimens in seasonal and chronic allergic conjunctivitis. Clin Exp Allergy. 36:777-784
- Hu Matsumoto et al., Corneal in vivo confocal scanning laser microscopy in AKC. Ophthalmology 115:2004-2012
- McGill JI. A review of the use of olopatadine in allergic conjunctivitis. Int Ophthalmol 2004; 25:171¡V9.
- Bleik JH et al. Topical cyclosporine in vernal keratoconjunctivitis. Ophthalmology 1991; 98(11):1679¡V84.
- Hingorani M et al. A randomized, placebo controlled trial of topical cyclosporine -A in steroid dependent atopic keratoconjunctivitis. Ophthalmology 1998; 105(9):1715¡V20.
- Lovieno Aet al. Preliminary evidence of the efficacy of probiotic eye-drops in patients with vernal keratoconjunctivitis. Graefes Arch Clin Exp Ophthalmology 2008; 246:435–441.
- Mainardi T et al., Complementary and alternative medicine: herbs, phytochemicals and vitamins and their immunologic effects. J Allergy Clin Immunol 2009; 123:283–294 Immunology and allergy clinics of North America. Feb 2008. Vol 28. Number 1
