An ulcer is a breach in the continuity of corneal epithelial. However, a corneal ulcer is an epithelial breach with superficial tissue loss (subepithelial or stroma) having variable grades of inflammation. The causes can be infectious (bacterial, fungal, viral, Pythium) and autoimmune (marginal keratitis, peripheral ulcerative keratitis). Here, we discuss ten essential clinical key points for diagnosing a corneal ulcer.
1. History
A detailed and meticulous history is essential in each case. The patients commonly present with pain, redness, photophobia, and defective vision. The history of trauma (vegetative matter, stick, mud, clay, insect bite, etc.), onset, presentation, and progression should be noted. Sudden onset and rapid progression are associated with Pseudomonas, Pneumococcus, and Staphylococcus ulcers. Gradual onset and slow progression are seen in Acanthamoeba, Nocardia, and Mycobacterium. A detailed history of ocular (Contact lens, adnexal infections, ocular surface disease) and systemic risk factors (Diabetes mellitus, malnourishment) will also explain the etiology. A family history of connective tissue disease (Autoimmune keratitis) and any surgical interventions in the past should also be noted.
2. Preliminary examination
It includes essential evaluations such as:
Visual acuity is usually reduced in corneal ulcer cases due to edema, hypopyon, uveitis, and endophthalmitis.
Intraocular pressure- is assessed by digital tension or non-contact tonometry and can be raised in viral keratitis secondary to trabeculitis.
Duct evaluation is vital as the duct can be blocked, and bacterial overload may be responsible for the ulceration.
DM profile- Uncontrolled diabetes may cause immunosuppression and reduced corneal sensation, which may be responsible for corneal ulceration and slow response to treatment
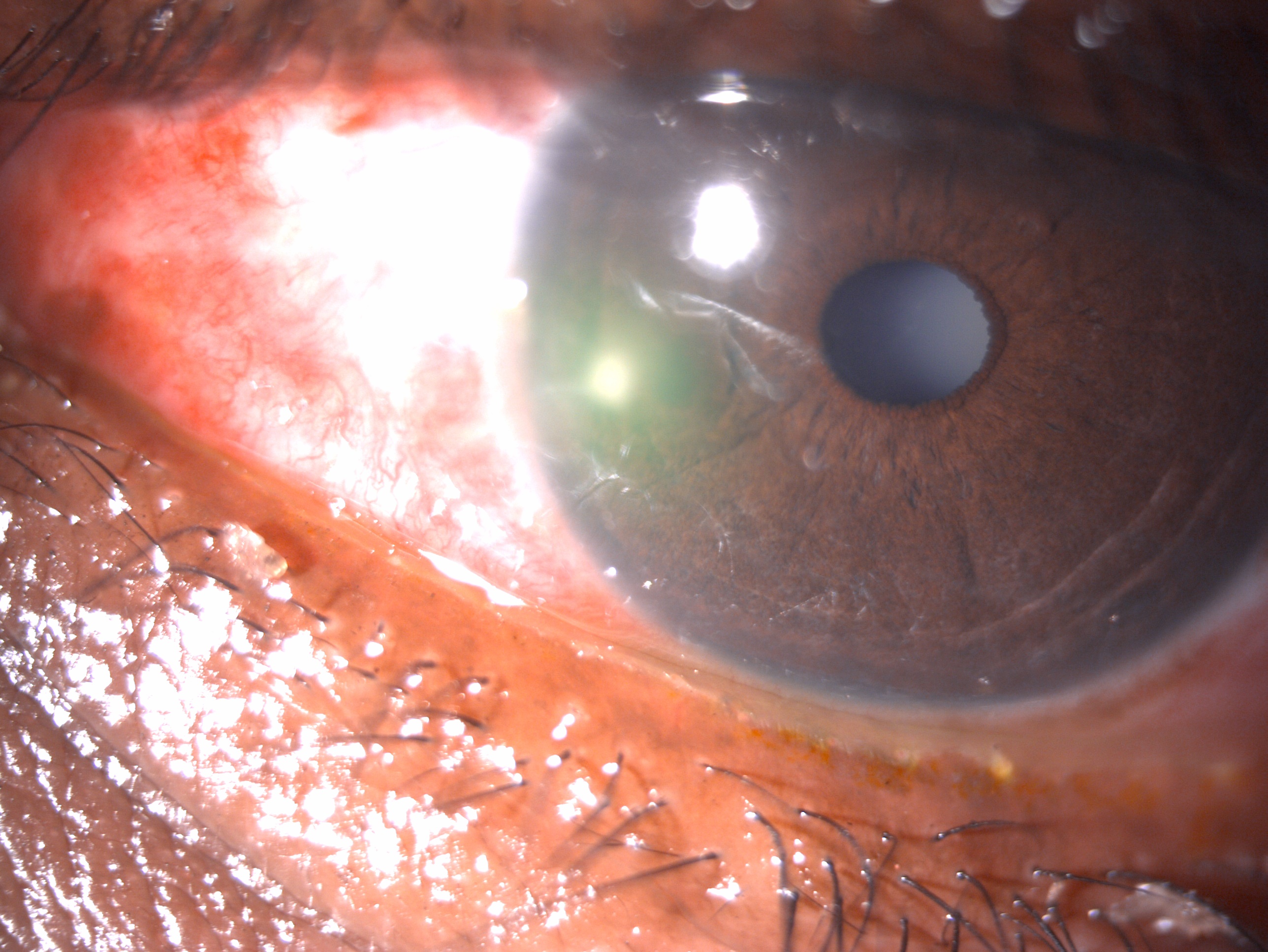
Adnexa- should be examined for blepharitis, MGD, trichiasis, lagophthalmos, ectropion, and dacryocystitis
Conjunctiva- follicles, papillae, pseudomembrane, discharge, vascularization, dry eyes, conjunctivilization, foreign body, and limbal stem cell deficiency should be examined.
Discharge- Greenish (pseudomonas), purulent, mucoid (bacterial ulcer), membranous (Corynebacterium), mucopurulent (pseudomonas), watery (viral/ bacterial).
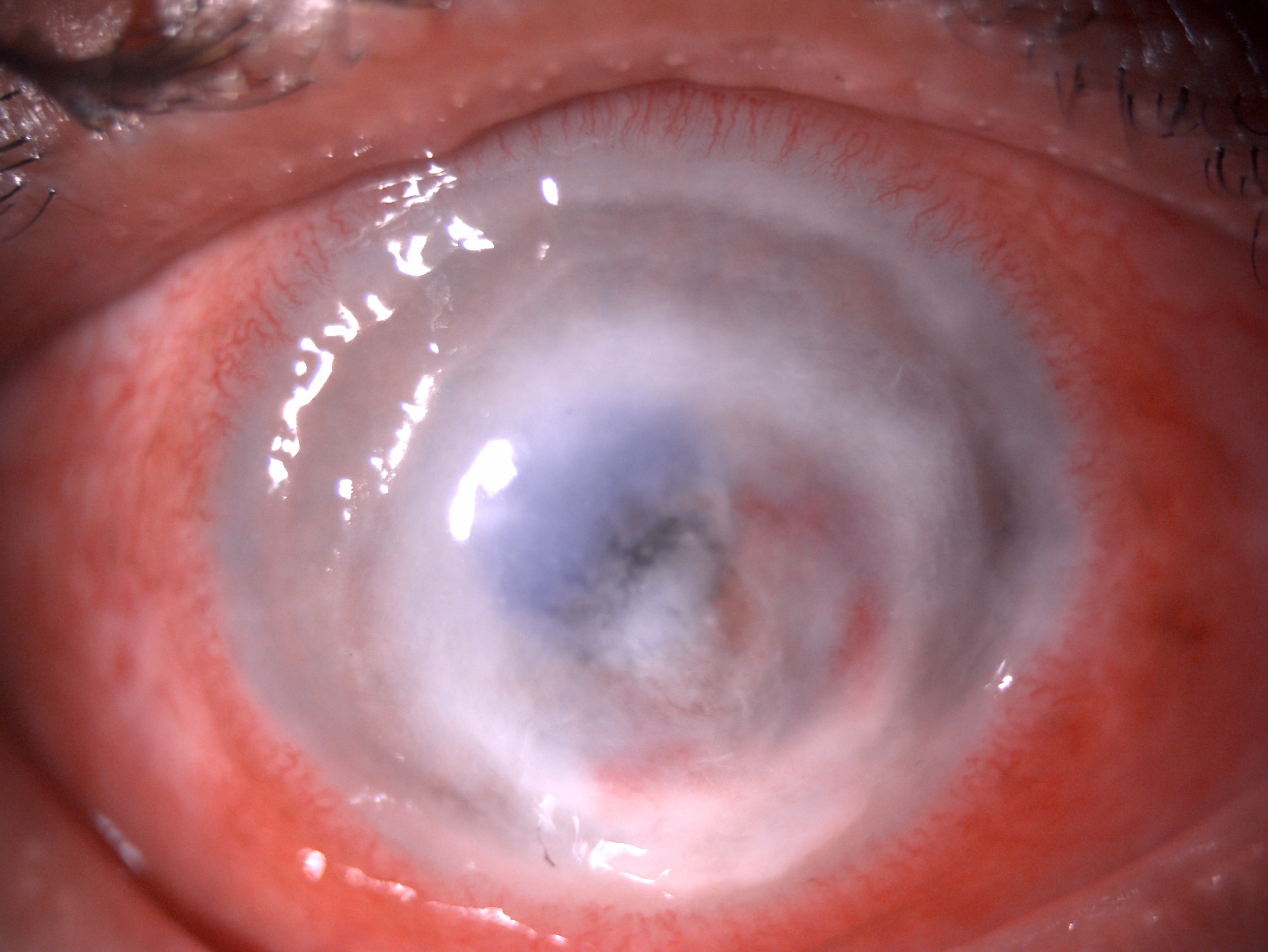
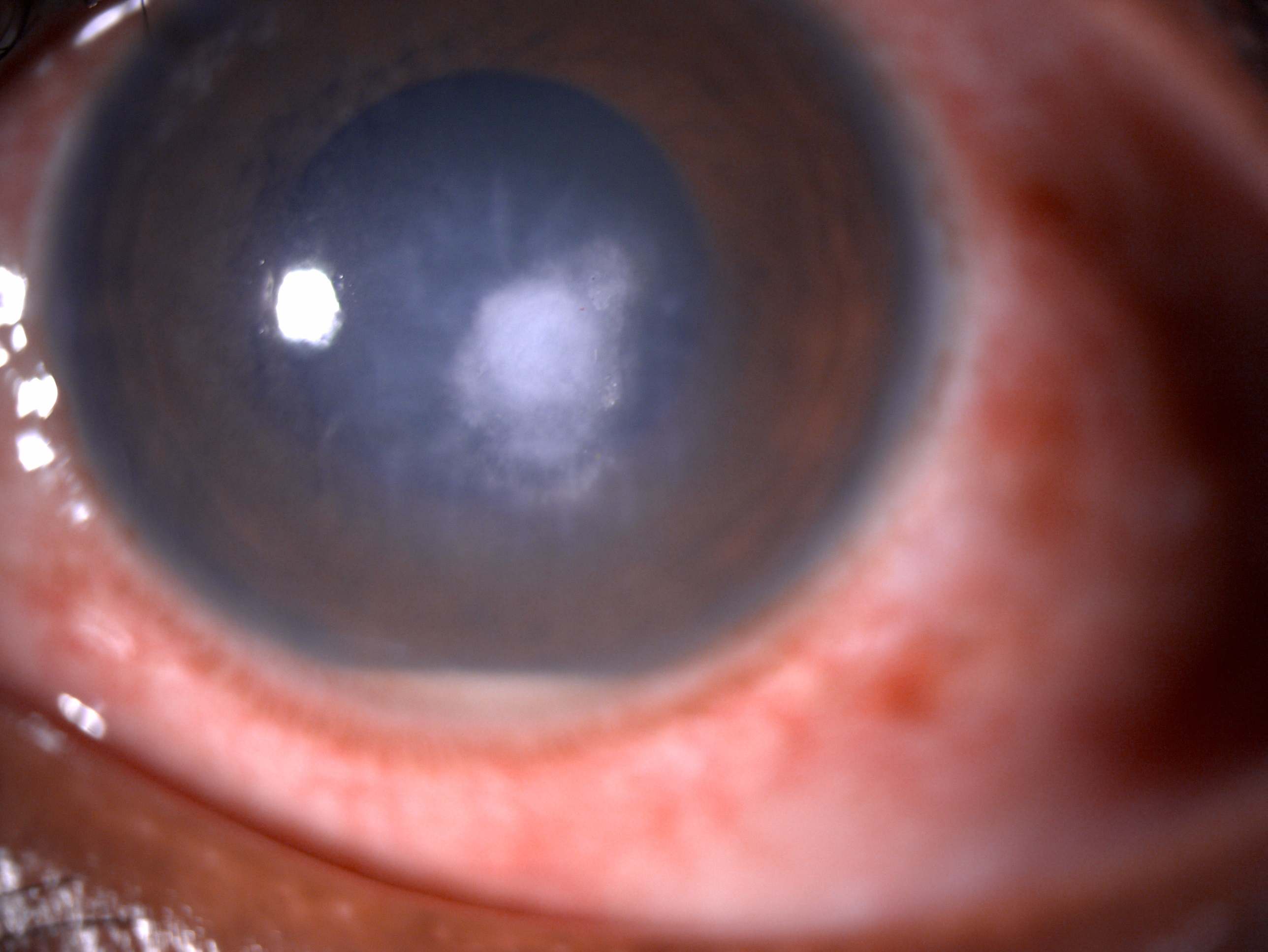
3. Corneal ulcer characteristics
Location- In general central (infective) and peripheral (autoimmune)
Central- Staphylococcal, Aspergillus, Pseudomonas and Fusarium, Paracentral- Pseudomonas, Fusarium, Peripheral- Herpes simplex, Mycobacterium, PUK, Marginal keratitis, Mooren's, Superior- foreign body, shield ulcer, marginal keratitis, Inferior- Exposure keratopathy, marginal keratitis
Size- The maximum vertical and horizontal diameter must be noted, and the size of the epithelial defect (fluorescein staining) and infiltrate must be separately documented.
Shape- Gives the closest clue in most of the cases. Dendrite- HSV keratitis, Ring-shaped- Acanthamoeba, Ground/ Hourglass appearance- Pseudomonas, and Wreath shaped- Nocardia, Cracked windshield appearance- Mycobacterium
Margins-Well defined- healing ulcers, Punched out Neurotrophic, Feathery- fungal and Overhanging- Mooren's ulcer
Base-Dry looking- fungal, Necrotic slough with discharge- Pseudomonas, Crater formation- PUK, Mooren's, Early stomal melt- Pythium
Depth- Best assessed with oblique slit lamp illumination. It can be divided into anterior stromal (superficial 1/3), mid-stromal, posterior stromal ( more than 2/3 stroma), and total thickness infiltrate.
Associated findings- Satellite lesion, endoexudates, limbal spread, hypopyon are other characteristics that should be documented. Corneal scarring and ghost vessels are seen in recurrent viral keratitis. Pseudo dendrites, radial perineuritis in Acanthamoeba, coarse multifocal raised superficial punctate keratitis in Microsporidium, SPK's in a quiet eye- Thygeson's keratitis
Vascularization- Should be differentiated as superficial and deep. Superficial vascularization is seen in marginal keratitis and most noninfective and infective keratitis. Deep vascularization is usually a sign of viral keratitis, and old cases of viral keratitis will have ghost vessels.
Pigmentation- Gives an essential clue in dematiaceous fungi Curvalaria, Alternaria, and Cladosporium.
4. Corneal sensations
They are evaluated clinically with the help of a cotton wisp when the patient is looking in opposite gaze or Cochet-Bonnet esthesiometer). Reduced corneal sensations are noted in viral keratitis, neurotrophic keratitis, and patients with diabetes mellitus.
5. Colour photographs and Schematic diagram documentation
The ideal way to assess the progression or resolution of a corneal ulcer is colour photographic documentation on each visit which gives a clinical clue to the response to treatment. If the facility is not available, colour schematic diagrammatic documentation should be done to assess the treatment response. Green- epithelial defect, lens yellow- infiltrate, hypopyon black- a scar, IOL blue- edema, red- congestion, hyphema brown- KP's,
6. Systemic and other signs
Anterior chamber- Should be assessed for anterior chamber reaction and hypopyon, which can be mobile (bacterial), fixed (fungal), sterile (Behcet's), and hemorrhagic (viral- HSV, Pneumococcus)
Iris- Should be examined for neovascularization (long-standing ulcers, Pythium), peripheral anterior synechiae, posterior synechiae, and prolapse in case of perforation.
Pupil- is sluggish or dilated (atonic) in majority cases due to persistent inflammation.
Lens- can be evident in early stages and cataractous in long-standing ulcers due to persistent inflammation. Pigments and broken synechiae can also be noted on the anterior lens capsule.
Fundus evaluation to rule out endophthalmitis or spillover in suspected cases and examination of other eye should be performed in each case
Systemic evaluation- to rule out comorbidities and immunosuppression
7. Grading the ulcer
it is essential to have a fair idea regarding the prognosis in each case. Microbial keratitis is best graded based on Jones's criteria.
|
S. No |
Ulcer characteristic |
Grading of Ulcer |
||
|
Mild |
Moderate |
Severe |
||
|
1 |
Size |
<2 mm |
2-5 mm |
>5 mm |
|
2 |
Depth |
1/3 |
1/3-1/2 |
>1/2 |
|
3 |
Infiltrate depth and extent |
Superficial and dense suppuration |
Mid-stromal with dense suppuration |
Posterior stromal with dense suppuration |
|
4 |
Scleral involvement |
None |
None |
May be involved |
8. Corneal scraping
Scraping is performed under topical anesthesia (0.5% proparacaine) using a Kimura spatula or Bard-Parker blade or a 26G needle from the ulcer base and margins. The routine stains used for smearing are Gram, KOH, Giemsa, calcofluor white (CFW), and lactophenol cotton blue. Gram stain can pick up bacteria, fungi, microsporidia, Giemsa- Bacteria fungi, Acanthamoeba, microsporidia, CFW- Acanthamoeba, fungi, microsporidia, Acid-fast stain- Ziehl Neelsen auramine 0 for Mycobacterium, Nocardia and Grocott–Gömöri methenamine silver- Fungi, Acanthamoeba, microsporidia and Periodic acid–Schiff (PAS)- Fungi and Acanthamoeba.
9. Culture
Culture should be obtained in most cases of corneal ulcers so that microorganisms can be identified and sensitivity patterns can be determined. Culture results are usually available in 48-72 hours. The various culture media used for identification are blood agar (5-10%) identified most bacteria and fungi, chocolate agar- Hemophilus, Neisseria, Moraxella, SDA- fungi, Leaf incarnation- Pythium, Non-nutrient agar with E.coli- Acanthamoeba, Brain heart infusion broth- streptococci, meningococci, yeast, Cooked meat broth- P. acne, L J medium- Mycobacteria, Nocardia.
10. Treatment
Treatment depends on the microorganisms and severity of the ulceration. Hospital admission is warranted for severe ulcers, one-eyed patients, comorbid patients, and patients requiring therapeutic keratoplasty. The offending agent must be eliminated, such as contact lens, foreign body, steroids, etc. Topical drug therapy based on microorganisms profile. Monotherapy is indicated in small ulcers < 4x4 mm, and dual therapy should be initiated when ulcer size > 4x4 mm and the ulcer involves a visual axis. Initially, the drug is instilled hourly and then tapered based on the clinical response. The drugs for various keratitis can be:
Bacterial keratitis- Antibacterials
Gram-positive cocci –Cefuroxime, Vancomycin, Teicoplanin
Gram negative rods- Fortified’ gentamicin or 1.5% fluoroquinolone or ceftazidime 5%
Gram negative cocci- Fluoroquinolone or ceftriaxone 5%
Mycobacteria- Amikacin or 2% clarithromycin 1%
Nocardia- Amikacin or 2% trimethoprim 1.6% + sulfamethoxazole 8%
Fungal keratitis- Antifungals
The drug of choice is 5% natamycin suspension. The other drugs are 1% itraconazole ( more sensitive for fusarium), 1% voriconazole ( more sensitive for aspergillus), Amphotericin B (candida).
Pythium keratitis- Antipythium drugs- 0.2% Linezolid and 1% amikacin
Acanthamoeba keratitis- 0.02% PHMB and 0.02% Chlorhexidine
Viral keratitis- 5% Acyclovir ointment, 0.15% ganciclovir, oral acyclovir 400 mg
Adjuvant drugs
Cycloplegics-2.5% Homatropine / 1% atropine- to relieve pain from ciliary spasm, break the posterior synechiae (PS) and prevent the formation of PS
Antiglaucoma drugs- 0.5% timolol to prevent secondary glaucoma due to blockage of the trabecular meshwork
Lubricants- 0.5% CMC to promote ocular surface lubrication and healing of epithelial defects
Surgical treatment
Therapeutic keratoplasty- Implicated for non-resolving ulcer for more than 2 weeks, corneal perforation, melt, and limbal involvement.
Lens removal may be needed in the same sitting, or later the patient can be subjected to cataract extraction alone or combined with PKP.
Oral antibiotics and antifungals are indicated in cases with scleritis, non-resolving ulcers, and endophthalmitis
Steroids
Steroids are usually initiated 3-4 weeks after TPK based on the preoperative and post-operative button culture results and no signs of graft infection.
Patient compliance, education, counselling, and regular follow-up are critical elements in determining the final visual outcome of patients with a corneal ulcer.
References
- Garg P, Rao GN. Corneal ulcer: diagnosis and management. Community Eye Health. 1999;12(30):21-3. PMID: 17491983; PMCID: PMC1706003.
- Srinivasan M. Prevention of traumatic corneal ulcer in South East Asia. Community Eye Health. 2017;30(99):S15-S17. PMID: 29849440; PMCID: PMC5968419.
- Mark S, Mathias R, Roscoe D, Holland SP. The corneal ulcer one-touch study: a simplified microbiological specimen collection method. Am J Ophthalmol. 2015 Jan;159(1):37-43.e1. doi: 10.1016/j.ajo.2014.09.021. Epub 2014 Sep 22. PMID: 25244977.
- Kanski's Clinical Ophthalmology-A Systematic Approach. Eighth Edition

