Acute retinal necrosis was first described in Japan by Urayama and colleagues who described six otherwise healthy patients, presented with panuveitis and retinal arteritis developing retinal detachment. At that point of time, this entity was known in the Japanese literature as “Kirisawa uveitis”1.Young and Bird first used the term “bilateral acute retinal necrosis” in 1978 2. In 1982 Culbertson and associates 3 first reported the possible involvement of a herpes group virus as the causative agent of acute retinal necrosis syndrome after histopathology and electron microscopy evaluation of an enucleated eye. The Executive Committee of the American Uveitis Society 4 de?ned the disease by its clinical characteristics and disease course in 1994.
Epidemiology:
Acute retinal necrosis generally affects healthy, immunocompetent individuals regardless of sex or race. However,Fisher et alfound little male preponderance in their study 5. The disease affects typically young adults. Bimodal age distribution has been described by various authors with peaks at 20 and 50 years of age 6, 7, 8. However, ARN has been reported in children also. Acute retinal necrosis generally begins with unilateral disease. The second eye becomes involved in one-third cases usually within 1 to 6 weeks 5, 9. The longest interval reported between the involvements of two eyes is 34 years10. An association with specific human leukocyte antigens (HLAs) has been reported by various studies. Holland and associates11 reported that 55% of American white patients with acute retinal necrosis manifested the HLA-DQw7 antigen in their study. In the Japanese patients, HLA-Aw33, B44, and DRw6 are more commonly expressed 12. Also in patients with a more fulminant and aggressive presentation are reported to be associated with HLA-DR9 13. However, from India no such reports are available to date.
Etiology:
Acute retinal necrosis is caused by multiple members of the Herpes virus family. Varicella-zoster virus (VZV) accounts for the majority of cases 15. Other viruses include herpes simplex type 1 (HSV-1) and type 2 (HSV-2), and rarely cytomegalovirus (CMV) and Epstein-Bar virus (EPV). Vitreous or aqueous samples from 30 eyes of 28 patients with a diagnosis of acute retinal necrosis were analyzed by Ganatraet al7using polymerase chain reaction to determine the viral cause of acute retinal necrosis and to evaluate possible associations between the viral cause and the patient’s age. From the results of their study, the authors concluded that varicella-zoster virus or herpes simplex virus type 1 cause acute retinal necrosis syndrome in patients older than 25 years, whereas herpes simplex virus type 2 causes acute retinal necrosis in patients younger than 25 years. They also suggested that a history of central nervous system infection in a patient with acute retinal necrosis syndrome suggests that herpes simplex virus is likely to be the viral cause. Tran and associates14 reported the association of herpes simplex virus type 2 with young age and triggering events like trauma or systemic corticosteroids in acute retinal necrosis patients.
Histopathological features:16
Histopathology of acute retinal necrosis reveals full-thickness retinal necrosis-all layers of retina & retinal pigment epithelium is involved. Retinal and choroidal vessels are also involved and are characterized by occlusion of the vascular lumen. A transition zone containing inflammatory cells, cellular debris, and viral inclusion bodies within retinal cells are observed between necrotic and normal retina. The vitreous cavity shows sloughed necrotic tissues of inflammation with macrophages and polymorphonuclear cells.
Clinical Pictures:
Early symptoms are usually very minimal and patients may complain of irritation, redness, photophobia, and floaters. Some patients complain of mild-to-moderate ocular pain, which may be worse with eye movements. Anterior segment examination reveals mild to moderate anterior uveitis. In some patients, there may be increased intraocular pressure due to secondary glaucoma. Posterior segment involvement occurs within 1 to 2 days. The characteristic triad of lesions encountered in acute retinal necrosis consists of moderate to severe vitritis, confluent necrotizing retinitis and vasculitis. Ophthalmoscopically, the retinal necrosis appears as well-demarcated, multifocal patches of yellowish-white infiltrates in the periphery at the level of deep retina and retinal pigment epithelium. The lesions usually start in midperiphery and do not follow the architecture of retinal vessels. The border between the necrosis and normal retina appears well defined, smooth, and geographic; and retinal hemorrhages, although present, are not a prominent feature. Active vasculitis is characterized by vascular sheathing and perivascular small intraretinal hemorrhages. Characteristically arteries are more affected than veins. Over the few weeks, retinal necrosis becomes confluent and progresses rapidly and circumferentially toward the posterior pole. It should be kept in mind that although the involvement of macula is not a characteristic feature of acute retinal necrosis, its involvement does not preclude the diagnosis. As the retinal necrosis and sloughing progress, resultant debris accumulation and inflammation of vitreous ensues often giving rise to a dense vitreous haze.
STAGES OF ACUTE RETINAL NECROSISStage 1:Necrotizing retinitis
Stage 2:Vitreous opacifications / organization
|
|---|

Figure1: Acute retinal necrosis. Note the characteristic vitreous haze
Course of the disease:
With treatment resolution of acute retinal necrosis begins approximately in 3 weeks. In untreated patients, inflammation starts resolving 6 to 12 weeks after the onset of symptoms. Retinal thinning and atrophy starts at the peripheral margins and gradually moves centrally. Meanwhile, retinal pigment epithelium perturbation develops with areas of clearing they form a characteristic “Swiss- cheese appearance”. Vitreous organization and traction continue to develop during this phase. The thin atrophic retina often contributes to the development of retinal holes or tears, which typically appear at the junction of the normal and affected retina. Retinal holes, combined with vitreous traction, lead to retinal detachment in up to 75% of cases 5, 9, 17. Thus retinal detachments in acute retinal necrosis patients have both a rhegmatogenous and tractional component.(Figure 2)
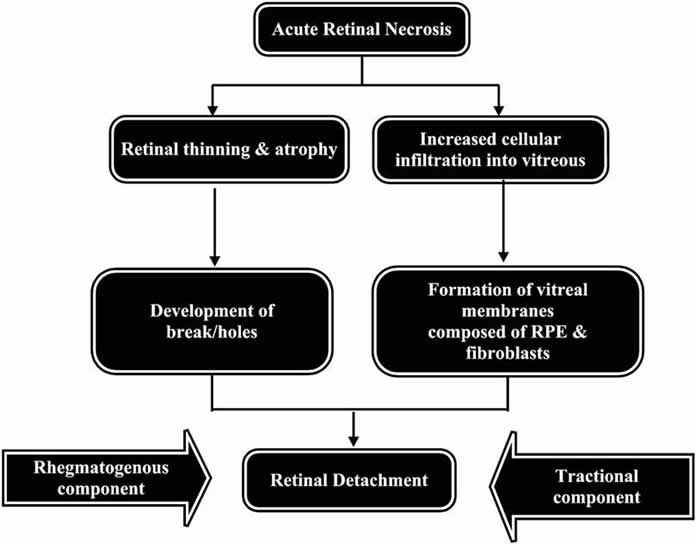
Figure2: mechanism of retinal detachment in acute retinal necrosis
Diagnosis:
Diagnosis of acute retinal necrosis is usually based on clinical appearance and course. However, patients with atypical presentation should be investigated as a delay in initiation of treatment may significantly affect the visual prognosis. Conventional methods of viral isolation like viral culture are cumbersome and time-consuming. The best option for investigating such challenging cases with diagnostic dilemma is polymerase chain reaction. PCR has been proved more than 90% sensitive for detection of VZV, HSV & CMV 7, 18, 19.With the advent of a newer technique like real-time PCR, which helps quantitative estimation of the pathogen, aqueous or vitreous specimens can be analyzed in conditions where the cause of severe uveitis may not be obvious.
Differential Diagnosis:
Various clinical entities can present as necrotizing retinitis thereby making the diagnosis of acute retinal necrosis often difficult. Few such conditions are discussed here with their differentiating feature with acute retinal necrosis.
Progressive outer retinal necrosis (PORN)
Progressive outer retinal necrosis is another necrotizing herpetic retinopathy, which occurs in patients with acquired immune deficiencysyndrome. Likeacute retinal necrosis, VZV and HSV are also common causative agents of PORN but, their clinical course and features is different. In progressive outer retinal necrosis, as the name suggests, the outer retina is primarily involved. Macular involvement commonly occurs early unlike acute retinal necrosis. There is minimal or absent occlusive vasculitis andanterior chamber or vitreous inflammation.
|
Key points of differentiation of Progressive outer retinal necrosis
|
|---|
Cytomegalovirus Retinitis
Differentiating cytomegalovirus retinitis form acute retinal necrosis is very important because it does not respond to antiviral drug acyclovir recommended for acute retinal necrosis. Cytomegalovirus retinitis is the most common necrotizing retinitis, generally occurs in immunocompromised individuals with CD4 lymphocyte less than 50 cells/mm.
The clinical course of the CMV retinitis is chronic and indolent with minimal or absent vitreous in?ammation. Characteristic lesions are described as granular and they are usually distributed near retinal vessels, suggesting a hematogenous spread. Active retinitis occurs adjacent to atrophic areas demonstrating a brush-?re appearance. Characteristically hemorrhage is more common in CMV retinitis than in acute retinal necrosis.
|
Key points of differentiation of Cytomegalovirus retinitis
|
|---|
Toxoplasma chorioretinitis:
In immunocompromised individuals, toxoplasma chorioretinitis can present with a primary infection and lack the typical chorioretinal scar seen in immunocompetent patients thereby complicating the diagnosis. In?ammation is usually more intense, retinal hemorrhage occurs less frequently, and vasculitis is more prominent adjacent to areas of necrosis. The peripheral retina is usually less involved in toxoplasmosis compared with ARN syndrome. Serological tests also can aid in diagnosis.
|
Key points of differentiation of Toxoplasma chorioretinitis
|
|---|
Ocular syphilis
Ocular syphilis in an immunocompromised patient can present with a diffuse, patchy necrotizing retinitis, prominent vitritis, and vasculitis. History of previous syphilis infection and laboratory tests like nonspeci?c treponemal antibody tests, such as rapid plasma reagin (RPR) and Venereal Disease Research Laboratory (VDRL), and speci?c treponemal antibody tests, such as ?uorescent treponemal antibody absorption (F TA-ABS) and microhemaggluntination test (MHA-TP) helps in diagnosis.
|
Key points of differentiation of Ocular syphilis
|
|---|
Treatment:
A. MEDICAL THERAPY:
Antiviral Agents:
The aim of medical therapy in acute retinal necrosis is rapid recovery of the disease and prevention of fellow eye involvement. As majority of cases of ARN are due to either HSV or VZV infections, intravenous acyclovir is the current medical treatment of choice for acute retinal necrosis.
Acyclovir is a guanine analog with activity against VZV, HSV-1, HSV-2, and Epstein-Barr virus, although most strains of CMV are resistant to it. The drug selectively inhibits DNA polymerase, requiring a virus-speci?cthymidine kinasefor activation. Acyclovir targets only virus infected cells and limits toxicity to human cells.The reason is only the virus infected cells contains a virally encodedthymidine kinasewhich is required for transformation of acyclovir into acyclovir tri-phosphate. Recommended therapeutic regimen consists of induction with 15 mg/kg/d intravenous acyclovir in 3 divided doses for 7 to 10 days and oral antiviral medication is then with either acyclovir (800 mg 5 times a day), valacyclovir (1 g 3 times a day), or famcyclovir (500 mg 3 times a day) is continued up to six weeks or more. Major side effect of acyclovir is on renal function. This is due to crystallization and deposition of the drug in the kidneys of patients who are dehydrated or have preexisting renal insufficiency. Renal dysfunction can be avoided by infusing acyclovir slowly over 1 hour and administering 1 liter of fluid with each gram of the drug. Oral acyclovir has rarely been associated with renal dysfunction. Nausea, vomiting, and abdominal pain can occur and probably represent a direct toxic effect on the gastrointestinal tract.
|
EFFECT OF ACYCLOVIR THERAPY IN ACUTE RETINAL NECROSIS CASES
|
|---|
Often few patients, mainly the immunosuppressed patients do not respond to treatment with acyclovir. It should be kept in mind that as discussed earlier in differential diagnosis section of this article, CMV retinitis mimicking the acute retinal necrosis may not respond to treatment with acyclovir .In such cases or in cases with acyclovir stains of HSV & VZV, gancicilovir or valacyclovir can be used. Though ganciclovir is highly effective against HSV & VZV, but for its greater risks of systemic toxicity, it should be used cautiously. Valacyclovir, the L-valyl ester of acyclovir, is a prodrug which is rapidly and nearly completely converted to acyclovir after oral administration. It has an excellent bioavailability which yields serum acyclovir levels comparable to intravenous acyclovir 22, 23 and requiring less frequent dosing than oral acyclovir. So, the drug has the same antiviral indications with the advantage of simpler dosing and it is as safe as oral acyclovir. Huynh et al 24reported that the oral administration of valacyclovir quickly leads to substantial vitreous acyclovir concentrations demonstrating the successful use of valacyclovir in the primary treatment of acute retinal necrosis. However it is not recommended in immunocompromised or HIV-seropositive patients.
Corticosteroid:
Corticosteroid has been used to inflammatory component of acute retinal necrosis because vitritis and vitreous organization progress in spite of effective antiviral treatment. Corticosteroid helps in reducing intraocular inflammation and clearing vitreous haze in acute retinal necrosis20, however they do not have any beneficial effect in reducing severity of the clinical entity and its lesions. It should be kept in mind that corticosteroid therapy in acute retinal necrosis should be started only after initiation of antiviral therapy as it can promote viral replication. Recommended dosage is 1 to 2 mg/kg for 1 week and the drug is tapered over 2 t o 6 weeks. Topical corticosteroid can be used to treat anterior segment inflammation, if present.
Antithrombotic therapy:
Some authors suggest the antithrombotic therapy to combat vascular obstructive complications of the acute retinal necrosis. However, till now there is no clinical trial that has proven efficacy of antithrombotic agents in acute retinal necrosis.
B. LASER PHOTOCOAGULATION
The major devastating squeal of acute retinal necrosis is retinal detachment which occurs in up to 75% of patients. Culbertson et al 16recommended to apply prophylactic confluent laser photocoagulation posterior to the areas of active retinitis to create a “new artificial ora serrata” posterior to the affected zones in which retinal holes are likely to develop. A reduction in occurrence of retinal detachment to 17% in patients with laser photocoagulation compared with 67 % in non laser treated patients has been reported by Sternberg and its associates 25.
C. SURGICAL MANAGEMENT OF RETINAL DETACHMENT
Surgical management of retinal detachment in acute retinal necrosis patients are often frustrating. The reasons for difficulty in repairing retinal detachment in acute retinal necrosis patients has been described by Blumenkranz et al26 who explained three reasons: (1) the multiplicity and posterior location of retinal breaks, for which selection of an appropriate scleral buckle becomes very difficult; (2) the presence of vitreous traction and proliferative vitreoretinopathy and (3) higher rate of postoperative complications due to the inflammatory nature of the disease. However with the help of techniques 27, 28, 29 like parsplana vitrectomy, air-?uid exchange, endolaser, and gas or silicone oil tamponade varying reports of success rate, even up to 100 percent has been published.
REFERENCE:
- Urayama A, Uamada N, Sasaki T, et al. Unilateral acute uveitis with periarteritis and detachment. Jpn J Clin Ophthalmol . 1971; 25:607–619.
- Young NJ, Bird AC. Bilateral acute retinal necrosis. Br J Ophthalmol . 1978;62:581–59
- Culbertson WW, Blumenkranz MS, Haines H, Gass DM, Mitchell KB, Norton EWD. The acute retinal necrosis syndrome: histopathology and etiology. Ophthalmology 1982; 89:1317–1325.
- Holland GN. Executive committee of the American uveitis society. Am J Ophthalmol .1994; 117:6 63–667.
- Fisher PJ, Lewis ML, Blumenkranz M, et al.: The acute retinal necrosis syndrome, part1:clinicalmanifestations.Ophthalmology1982, 89:1309–1316
- Van Gelder RN, Willig JL, Holland GN, et al. Herpes simplex virus type 2 a s a causeof acute retinal necrosis syndrome in young patients. Ophthalmology. 2001;108: 869–876.
- Ganatra JB, Chandler D, Santos C, et al. Viral causes of acute retinal necrosis. Am J Ophthalmol . 2000; 129:166–172.
- de Boer J, Luyendijk L, Rothova A, et al. Detection of intraocular antibody production to herpes viruses in acute retinal necrosis syndrome. Am J Ophthalmol .1994; 117: 201–210.
- Duker JS, Blumenkranz MS: Diagnosis and management of the acute retinal necrosis (ARN) syndrome. Surv Ophthalmol 1991, 35:327–343.
- Falcone PM, Brockhurst RJ: Delayed onset of bilateral acute retinal necrosis syndrome: a 34-year interval. Ann Ophthalmol 1993, 25:373–374.
- Holland GN, Cornell PJ, Park MS, et al. An association between acute retinal necorsis synedrome and HLA-DQw7 and phenotype Bw62, DR4. Am J Ophthal . 1989;108: 370–374.
- Ichikaw T, Saki J, Usui M. HLA antigens of patients with Kirisawa’s uveitis and herpetic keratiti. Atarashii Ganka . 1989;6:107–114.
- Matsuo T, Matsuo N. HLA-DR9 associated with the severity of acute retinal necrosis syndrome. Ophthalmologica . 1991;203:133–137.
- Tran THC, Stanescu D, Caspers-Velu L, et al. Clinical characteristics of acute HSV-2 retinal necrosis. Am J Ophthalmol . 2004;137:872–879.
- Culbertson WW, Blumenkranz MS, Pepose JS, et al. Varicella-zoster virus is a cause of the acute retinal necrosis syndrome. Ophthalmology. 1986;93:559–569.
- Culbertson WW, Blumenkranz MS, Haines H, et al. The acute retinal necrosis syndrome. Part 2: Histopathology and etiology. Ophthalmology. 1982; 89:1317–1325.
- Clarkson JG, Blumenkranz MS, Culbertson WW, et al.: Retinal detachment following the acute retinal necrosis syndrome. Ophthalmology 1984, 91:1665–1668.
- Short GA, Margolis TP, Kuppermann BD, et al. A polymerase chain reaction-based assay for diagnosing varicella-zoster virus retinitis in patients with acquired immunode?ciency syndrome. Am J Ophthalmol 1997;123:157–164.
- McCann J, Margolis T, Wong M, et al. A sensitive and speci?c polymerase chain reaction-based assay for the diagnosis of cytomegalovirus retinitis. Am J Ophthalmol 1995;120:219–226
- Blumenkranz MS, Culbertson WW, Clarkson JG, et al: Treatment ofthe acute retinal necrosis syndrome with intra- venous acyclovir.Ophthalmology 93:296-300,1986
- Palay DA, Sternberg P Jr, Davis J, et al. Decrease in the risk of bilateral acute retinal necrosis by acyclovir therapy. Am J Ophthalmol . 1991;112:250–255.
- Weller S, Blum MR, Doucette M, et al. Pharmacokinetics of the acyclovir prodrug, valacyclovir after escalating single- and multiple-dose administration to normal volunteers. Clin Pharmacol Ther 1993;54:595– 605.
- Hoglund M, Ljungman P, Weller S. Comparable acyclovir exposures produced by oral valacyclovir and intravenous acyclovir in immunocompromised cancer patients. J Antimicrob Chemother 2001;47:855– 861.
- Tony h. Huynh, mark w. Johnson, grant m. Comer, and douglas n. Fish. Vitreous Penetration of Orally Administered Valacyclovir. Am J Ophthalmol 2008;145:682– 686. 2008
- Sternberg P Jr, Han DP, Yeo JH, et al. Photocoagulation to prevent retinal detachment in acute retinal necrosis. Ophthalmology. 1988;95:1389–1393.
- Blumenkranz MS, Clarkson JG, Culbertson WW, et al: Vitrectomy for retinal detachment associated with the acute retinal necrosis syndrome.Am J Ophthalmd 106:426-429, 1988
- Blumenkranz M, Clarkson J, Culbertson WW, e t al. Visual results and complications after retinal reattachment in the acute retinal necrosis syndrome. The in?uence of operative technique. Retina . 1989;9:170–174.
- Matsuo T. Vitrectomy and silicone oil tamponade as an initial surgery for retinal detachment after acute retinal necrosis syndrome. Ocul Immunol In?amm. 2005;13: 91–94.
- McDonald HR , L ewis H, Kreiger AE, et al. Surgical management of retinal detachment associated with the acute retinal necrosis syndrome. Br J Ophthalmol .1991;75:455–458.
- Browng DJ, Blumenkz‘ MS, Culbertson WW; et al: Association of varicella zoster dermatitis with acute retinal necrosis syndrome.Ophtlmology 94:602-606,1987
