The use of TORIC IOL in the modern cataract surgical world has rightfully become a necessary tool for all surgeons. This is because of the demand for customization and the need for great refractive outcomes, rendering all cataract surgeries as “REFRACTIVE CATARACT SURGERIES” today!
Patients no longer are happy being dependent on glasses or want to miss the chance of being less dependent on glasses after their cataract surgery! This article quotes a few of the top pointers that may benefit all cataract surgeons, even more, the young ophthalmologists evolve into refractive cataract surgeons with the use of TORIC IOLs. A very necessary next step in the era of constant changes and customizations that have been the last 5-10 years in cataract surgery! So, let's dive in:
1. Start Early, Start Strong (Small)
The first pointer is that the “mind games” of expectations with TORIC IOLs is a cloud that you don’t want to set in. So, it is important to start Toric IOL cataract surgeries much EARLY in practice. Don’t let patient expectations, your expectations or matching the experts be standards before you set into using these - astigmatism correcting IOLS. And whenever this mind block does hit you, remember a simple fact about Toric IOLs: “99% PLANNING for Success and 1% DEALING with Failure”. Odds that most of us would take in a blink! Also, the failures related to TORIC IOLs are NOT CATASTROPHIC and mostly can be dealt with by all Cataract surgeons!
Yes, the question of Armamentarium required to start use of TORIC IOLs does creep into our minds, and YES, it is an investment (if you have not upgraded to the latest TECHNOLOGY available for IOL calculations) but it is an investment that you make to come to terms with being a current refractive cataract surgeon! Also, there’s a thin line between budgeting for what’s required/needed and what is luxury! So, know your equipment and its use before dwelling on buying equipment. What you need is a reliable keratometry (often repeating amongst two of your basic (manual or auto k) and one keratometer (could be inbuilt in your biometer also) and good biometry. So a small bank balance may be required before you start Toric IOL in practice IN ORDER TO GET YOUR CALCULATIONS BANG ON!

2.Candidate Selection
Who?
The candidates that benefit from a TORIC IOL are those HAVING GREATER THAN OR EQUAL TO 0.75 D ASTIGMATISM, needing correction for sharper vision post-operatively. IDEALLY SCREEN ALL YOUR PATIENTS FOR BEING TORIC IOL CANDIDATES, that way, you are more prone to give an option rather than realise later that someone may benefit from TORIC IOL Implantation in their cataract surgery. Special focus on AGAINST THE RULE (ATR) ASTIGMATISM that you would want to correct more aggressively, especially in younger individuals, as we know that the older we get, the more ATR we develop. The same goes for being less aggressive while treating WITH THE RULE(WTR) Astigmatism.
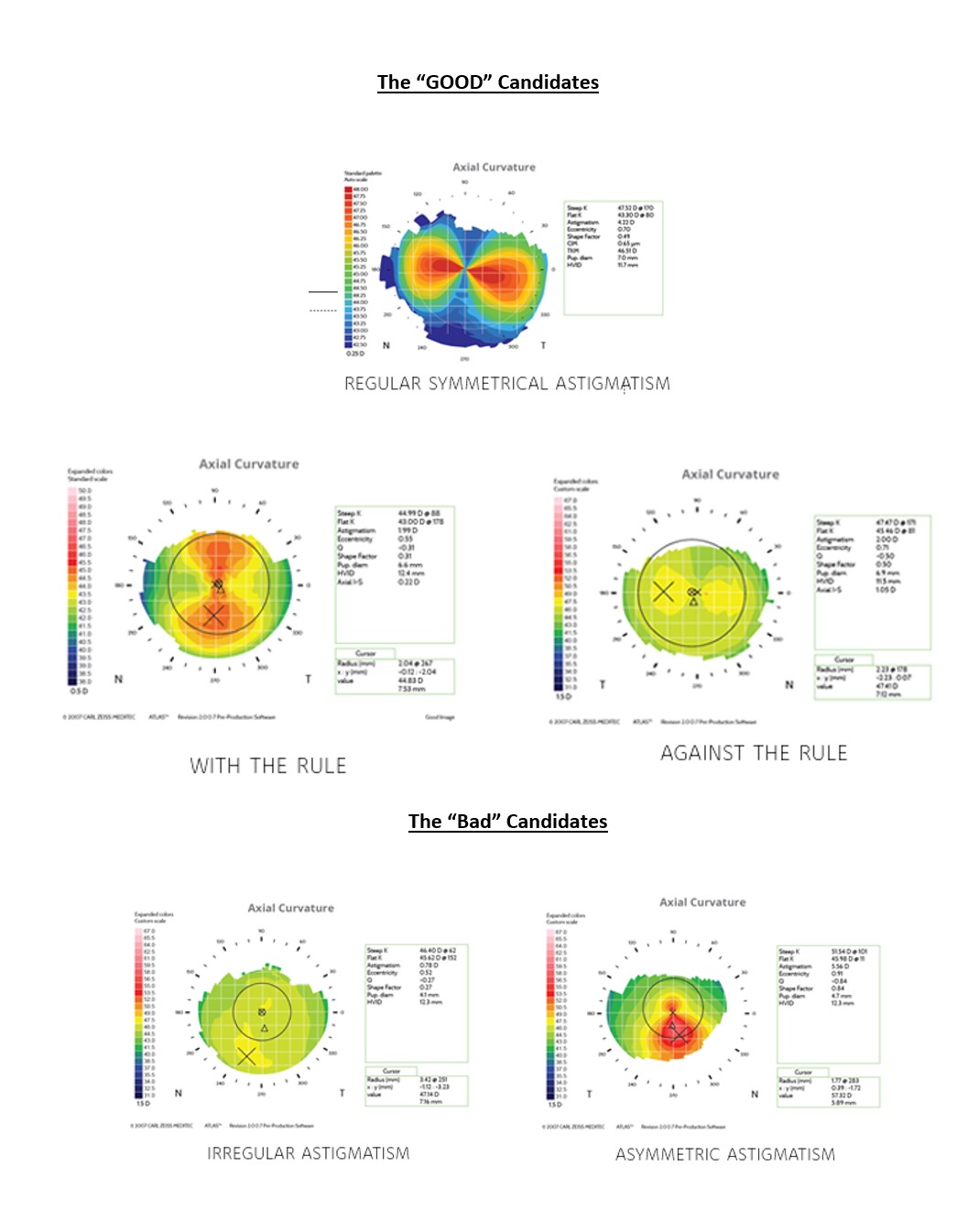
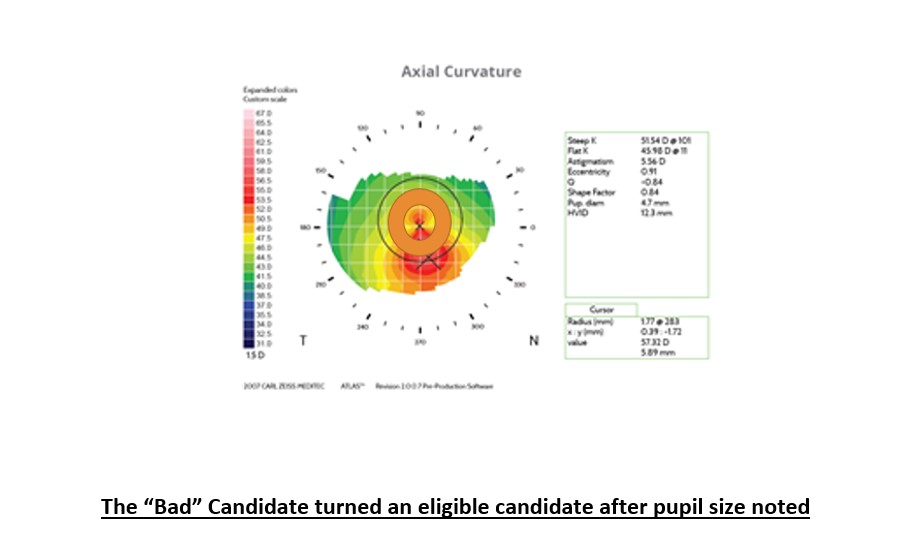
Also, It is very important to have a thorough study of the topography and choose only those cases with REGULAR ASTIGMATISM to treat with toric IOLS. Importantly, the patient should be KEEN IMPROVE his / her DISTANCE VISION WITH LESS DEPENDENCE ON GLASSES. Something that must be addressed before plans are drawn for surgery.
Who Not?
The candidates that don’t benefit from a TORIC IOL implantation or may have an adverse effect or in whom the surgeon may face a challenge post or intra-operatively are those having IRREGULAR ASTIGMATISM, HIGH ORDER ABERRATIONS and/or OTHER PRE EXISITING-OCULAR PATHOLOGY, amongst other causes. Previous corneal surgery may cause unpredictable results. Even cases having a previous history of refractive surgery may impose a separate group of challenges in calculations that may trouble beginners.
Challenges like small non-dilating pupil, Floppy iris syndrome, intraoperative hard eyes, cataract with loose zonules, hypermature cataracts with wrinkling capsular bags, or eve pseudoexfoliation syndromes may not be the ideal choice for premium IOLs like TORIC IOLs for all ophthalmologists in their early TORIC days.
3. Chair Time With Your Patient
The single most IMPORTANT POINTER that anyone can give is about sitting down with your patients for an extra 5 minutes if need be and explaining to them about their cataract, astigmatism and outputs that can be achieved post-surgery. This not only sets patients up for a successful surgical journey. It also helps the doctor understand better about their expectations after cataract surgery.
Explain to patients about cataracts in detail, explain about the pros and cons of any surgical experience even in the best of hands and also explain about ASTIGMATISM. How correcting astigmatism improves the surgical outcome and makes them LESS DEPENDENT ON GLASSES thereafter for a sharper image. DO NOT MENTION “GLASS-FREE VISION” OR PROMISE SOMETHING THAT CAN OVERLOOK HUMAN / TECHNOLOGY ERRORS.
Explain about the design of the IOL and its functionality of the IOL. Explain and use the terms like “to ALIGN to a certain axis”, “misalignment chances” and “redialling possibilities”. Explaining these beforehand makes you less vulnerable to conflict post-operatively and a more cooperative patient in the long run.
Do touch about the need for READERS after distance vision correction to the best and least glass-dependent IOL of choice if choosing monofocal toric IOLs. In case of EDOF or MULTIFOCAL or TRIFOCAL TORICs, do remember to NOT GUARANTEE but Level expectations as the “Best Prescription Available For Their Expectations”.
4. Make Checklists
The saying “People Fail, Checklists Don’t” is quite true for TORIC and PREMIUM IOL surgeries. So, it may be wise to make checklists. This ensures a less erroneous way of going around and achieving success by using this method whilst working up, preoperative ordering, marking, intraoperative directions and post-operative dealings for these patients. A QUICK EXAMPLE is:
Remember to make checklists for preoperative workup for your optometrists and you, for the generating of toric IOL sheet / calculating your toric IOL power, ordering IOL forms and checklists for receiving these IOLs in your setup. Make checklists so the person of concern mentions your IOL details in your OT list and checklists to ensure that your Intraoperative TORIC IOL sheets should be available, mentioning the IOL and the AXIS OF ORIENTATION in the OT.
Preop Evaluation Checklist
Autokeratometry
Manual Keratometry
Refraction
Corneal Topography
Optical Biometry
Immersion Biometry ( In Selected Cases)
OCT ( Macula)
Tear Film Analysis & Breakup Time ( Dry Eye Analysis)
Final IOL Power www.apacrs.org (BARRETT Online Topic Calculation)/www.ascrs.org
5. Ensuring Precision In Scans
The scans though technology dependent can often be a source of error that may result in leaving you red-faced. So, a few pointers on ensuring precise biometry is important. Often doing biometry for these patients is left to a trainee or another optometrist. It may be a good idea to do these scans yourself or by someone dedicated to do so, whom you trust will not cut corners. Do repeat these investigations on different dates or different times, if need be, on the same machine.
Repeat Keratometry measurements can be done via different machines like auto keratometer, manual keratometer, and topographer to get a better value. Avoid any dilated biometry or topography, and do take note of pupil diameter (most machines give a value). Dry Eye Syndrome patients will need treatment before doing biometry.
6. Topography is Key!
Repeat your topography scans when in doubt. As beginners and as surgeons meeting patient expectations, we must aim to provide Toric IOLs for all regular astigmatism patients where it is a necessity. Reading of Topography is a must-know art for all refractive cataract surgeons in order to differentiate between a good candidate and a bad one.
7. IOL Nuances: Choosing The Correct IOL For You
PREFER to run both eyes biometry values and scans for all patients before counselling surgery. This makes the plan transparent for both eyes, even if surgery may not be required in the second eye at that time. This helps gain the confidence of the patient in the long run and helps counsel them better because binocular results matter more in the premium IOL segment!
Always take 5 mins off your schedule to sit down and calculate the biometry scan and match it with the one you get off your machine (inbuilt). Some doctors prefer to run the scan via two or more formulas too! That, too is acceptable but has the iota chance of creating a bit of confusion whilst ordering. So choose the formula that works best for you. Some companies also like to do the calculations for you, and that can be a boon to cross-check your values.
Before ordering the IOL, make sure you have all the details like optical A Constant, model number and name of the IOL and your Surgically Induced Astigmatism (SIA) data with you. Some IOL manufacturers prefer to share the BARETT LF with their IOL model and prefer to use that. Always order the IOL based on CYLINDER VALUE AT THE IOL PLANE and NOT IN TERMINOLOGY OF T1, T2, T3, etc, which may be specific to one IOL company. In your calculation sheet, prefer to choose the astigmatic correction power that corrects the resultant to a WITH -THE-RULE ASTIGMATISM or closest to IT.
With the advent of Minimal Invasive Cataract Surgery (MICS) and incision sizes going down to 2.2mm, the SIA can be assumed as close to 0.1D when the incision is made temporally (in and around the degrees 10-170 degrees) as per the concept of CENTROID SIA. This makes calculating SIA redundant if making a temporal incision and doing a MICS.
On the other hand, by knowing your SIA you can use this as an important tool and play with your incision size and positions to minimise the required TORIC IOL astigmatic power.
The IOL company of choice varies with each surgeon and what papers you read (some company sponsored). A landmark paper from Ophthalmology in 2018 did suggest the use of one platform to have more rotational stability over the other (amongst prominent IOL makers available). Lately, newer IOL designs have been coming in, and the results are quite promising on these IOLs as well.
8. Don’t Underestimate The Tear Film
An evaluation of the ocular surface (DRY EYE EXAM) is one of the most important aspects of the preoperative routine for any patient who is considering a TORIC IOL. Dry eyes can significantly compromise the quality of vision, even after routine cataract surgery. Even more, Dry Eyes can make your calculations, biometry and topography faulty, thereby worsening the condition and setting up for IOL surprises!
During the preoperative evaluation, it is important to take any significant history for Dry Eyes before considering premium IOL implantations. These include fluctuating vision (one of the most important history given), contact lens intolerance, foreign body sensation, grittiness, and a record of ocular symptoms that worsen later in the day. Various tests are now readily available for Dry Eye Examinations, but the age-old Tear Break Up Time (TBUT), Tear meniscus height evaluation, and staining of the cornea to look for epitheliopathy are reliable indicators of moderate dry eyes.
A healthy and stable tear film makes the ocular surface healthy, thereby elevating the best chance of success after cataract surgery, more so if a premium lens technology is at play. Thereby, there is a need to address dry eye proactively, and a conversation must be made with the patient to discuss the treatment with respect to their dry eyes to ensure the resulting “wow effect” and match patient standards after refractive cataract surgery.
9. Making A Mark: Toric Marking Preoperatively And Intraoperatively
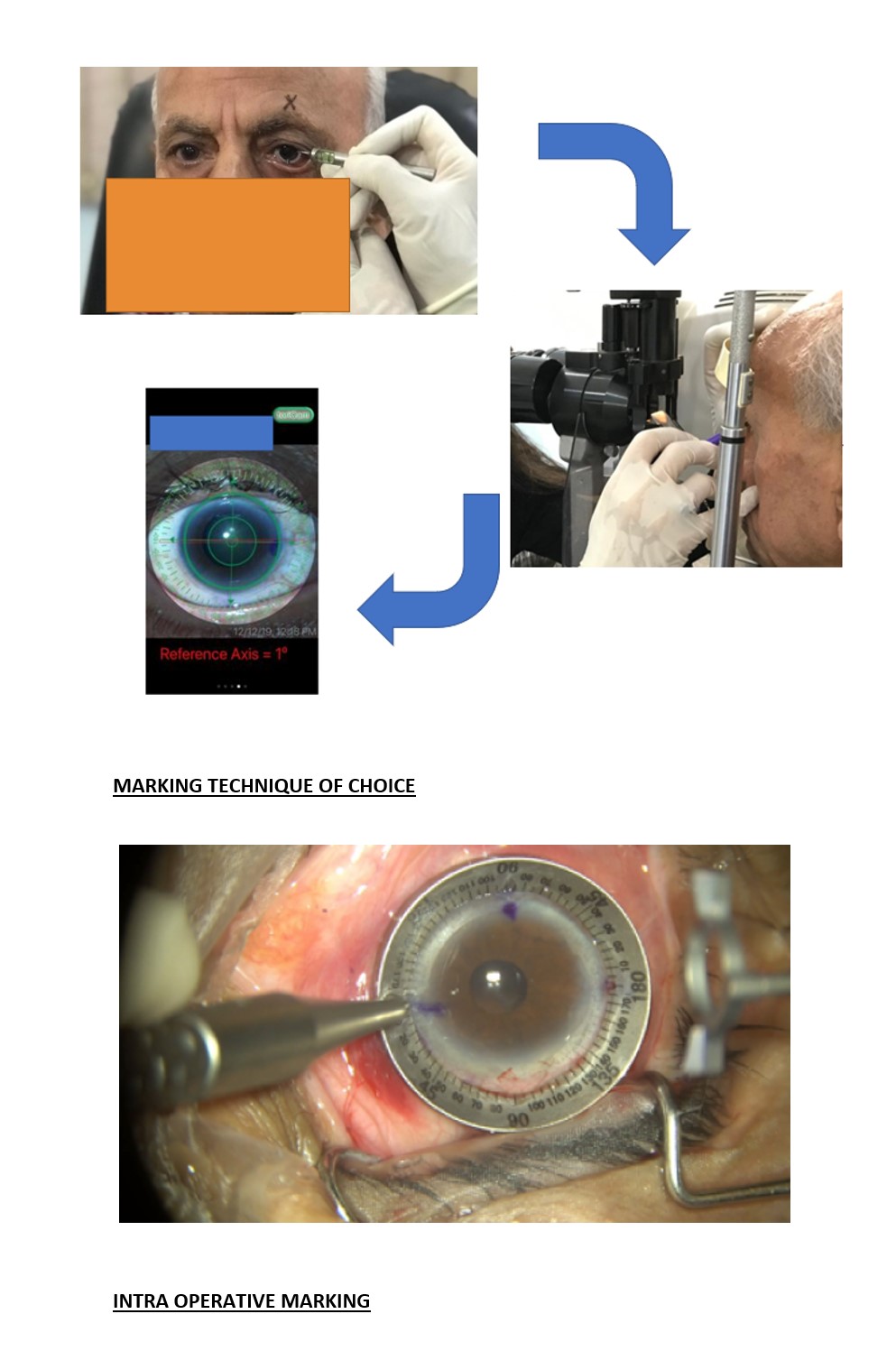
Not everyone has the opportunity or the funds to buy the latest mark/alignment tracking technology available in the market. But fear not! If you still follow the basic marking methods, be rest assured you are 99% on the mark! Various methods like the bubble marker, marking a vessel with a 26G needle or landmark vessel/edge marking on a slit-lamp are all methods that work well respectively in each surgeon’s hands.
Smartphone apps like TORICam, etc, are FREE and readily available that not only document the eye via a photograph but also using your phones pre-installed gyrometer evaluates the accuracy of your mark.
Intraoperatively it is a must to remark before you start the surgery and also locate and mark your final IOL alignment destination.
10. Intraoperative Pearls
The first and foremost important pearl is identifying and re-establishing your marks before you start your surgery. It is good practice to keep your calculated toric sheet IN FRONT OF YOU during your surgery, keeping ORIENTATION IN MIND. It is very important to know your incision site, size and final IOL placement axis and make marks accordingly. Another very important recommendation is a 5 to 5.5mm Capsulorrhexis which ensures a 360-degree overlap of the 6mm optic of the IOL. A smaller and a larger IOL is often the cause of Post Op Rotations and Other Complications.
One of the Top Pearls for intraoperative alignment is knowing your IOL design and managing your incision size after you do a thorough cortical wash and capsular polishing by a technique of your choice. Fill the bag with OVD and coat the endothelium with protective OVD before you inject the IOL and rotate 10-15degrees short of your final intraoperative mark. After which, do a thorough viscoelastic wash, and under hydro, rotate the IOL at your final destination for perfect alignment.
It is important to remove all OVD and also to remove all cortical matter before placing IOL in the desired axis. Also, do not over hydrate or look for a very tight eye on closure, as this would be undesirable and a reason for post-operative rotation. Also, avoid leaving air bubble in the anterior chamber as this too can lead to complications post-op.
Post Operative Trouble Shooting
As mentioned before TORIC IOLs are 99% planning for success and 1% battling failure, and if all these tips are followed, your choice of IOL and alignment is apt, then the only trouble shooting you may face is IOL Rotation, which you have already counselled your patient for! It may be best to wait 10 -12 days post-operatively till some degree of stability is ensured in these cases and then take them up for the proposed redialling if necessary. A few software’s online like myastigmatismfix.com are free to use and reliable methods of getting your rotations corrected.
Conclusion
TORIC IOLs is soon becoming the standard of care prescription IOLs in most practices throughout the WORLD. This is largely because of the quality improvement in visual outcomes noticed by surgeons and patients alike! Though a lot of planning is needed to achieve precision in results, the results are quite gratifying and rewarding with referrals in your practice! Hope these top pointers go in achieving similar outcomes for all that practice them.
