Chief Complaint: A 67 years old female came with the complaint of sudden painless diminution of vision in the left eye for 1 day.
History of Present Illness: Sudden painless diminution of vision with associated floaters in the left eye for the last 1 day. There was no history of any trauma, redness, watering or discharge.
Past Ocular History: No history of any past ocular disease
Past Medical History/ History of Medication: The patient was diagnosed to have diabetes mellitus type 2 and essential hypertension five years back and was on medications for the same.
Family History: No significant family history was present
OCULAR EXAMINATION
Best Corrected Visual Acuity (Snellen)
- Right eye (OD): 6/6, N6
- Left eye (OS): 6/36, N18
Ocular Motility/Alignment: Full, free and painless in all gazes
Intraocular Pressure (IOP)
- OD: 16 mmHg
- OS: 18 mmHg
Pupils: OU Round, regular and reacting to light
Slit-lamp Exam:
|
OD |
OS |
|
|
Lid/Lashes |
Normal |
Normal |
|
Conjunctiva/sclera |
Normal |
Normal |
|
Cornea |
Normal |
Normal |
|
Anterior chamber |
Normal depth and quiet |
Normal depth and quiet |
|
Iris |
Normal |
Normal |
|
Lens |
NS1 and mild PSC |
NS1 and mild PSC |
Dilated Fundus examination
|
OD |
OS |
|
|
Vitreous |
PVD |
Subhyaloid haemorrhage at the macular area |
|
Disc |
VCDR 0.2 :1, HNRR |
VCDR 0.2 :1, HNRR |
|
Macula |
FR sharp |
Obscured by overlying subhyaloid haemorrhage, which was more dense near the inferior vascular arcades |
|
Vessels |
Normal calibre with maintained AV ratio |
Mild vascular tortuosity |
|
Periphery |
Normal |
Normal |

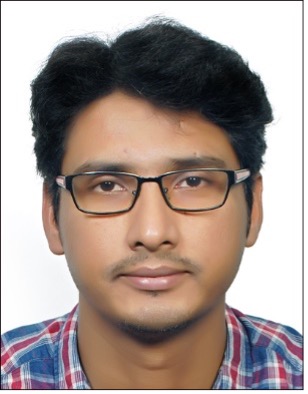
Figure 1: Colour fundus photograph of the left eye showing subhyaloid haemorrhage at the posterior pole involving the macula. Haemorrhage is more dense near the inferior arcade
Ancillary Investigations:
Fundus Fluorescein Angiography
Fundus fluorescein angiography (FFA) of the left eye (Figure 2. A and C) demonstrated areas of blocked fluorescence in the areas of subhyaloid haemorrhage. A pinpoint area of hyperflourescence was noted in the early phase in the inferotemporal area of the macula close to the inferior arcade. The hyperflourescence increased in size and intensity in the late phase – suggestive of leakage.
Indocyanine Angiography
Indocyanine angiography (ICG) (Figure 2. B and D) was advised as it can be more helpful in the visualisation of lesions in case of dense haemorrhage. A well-defined area of hypercyanescence is seen in the inferotemporal area of the macula along a retinal arteriole – more evident on ICG compared to FFA. There was no evidence of any branching vascular network adjacent to the lesion on ICG.
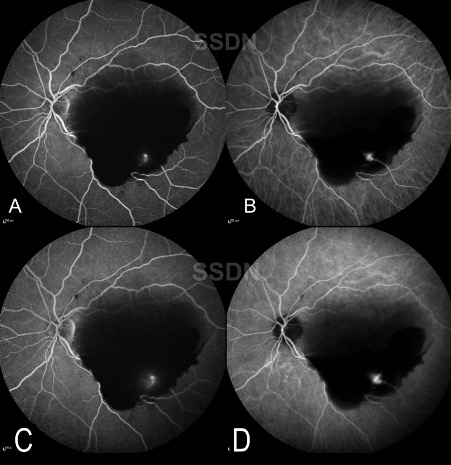
Figure 2: A) FFA showing pin-point hyperflourescence in the inferotemporal arcade along with blocked fluorescence due to overlying haemorrhage. B) ICG of the same eye showing a well-demarcated area of hypercyanescense in the inferotemporal arcade. No evidence of branching vascular networks can be seen. FFA and ICG showing leakage in the late phase ( B and D ).
Optical Coherence Tomography
Optical coherence tomography (OCT) of the macula in the foveal region (Figure 3) demonstrated increased reflectivity beneath the posterior hyaloid face along with backshadowing that obscured visualisation of the retinal layers – suggestive of subhyaloid haemorrhage, more intense at the inferior arcade and temporal to the fovea.
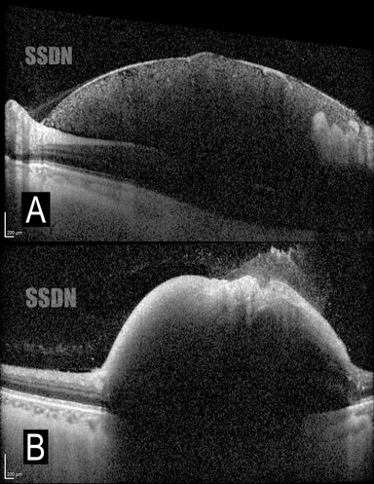
Figure 3: A) OCT scan of the macula in the foveal region showed subhyaloid haemorrhage. B) OCT scan at inferior arcade showed dome-shaped elevation overlying the retina with diffuse backshadowing obscuring the details of the underlying structure.
Differential Diagnosis:
- Proliferative Diabetic Retinopathy
- Retinal Telangiectasia
- Retinal Capillary Angioma
- Idiopathic Polypoidal choroidal vasculopathy
- CNVM with multi-layered bleed
Diagnosis:
Based on the clinical picture and the findings on FFA and ICG, a diagnosis of ruptured retinal macroaneurysm was made.
Clinical Course of the condition:
Based on the visual impairment, the clinical findings and the location of the subhyaloid haemorrhage, it was decided to perform a pneumatic displacement of the haemorrhage using 0.3 cc of 100% perfluoropropane (C3F8) gas along with an intravitreal injection of ranibizumab. During the immediate postoperative period, the subhyaloid haemorrhage was dislodged, resulting in dispersed heme in the vitreous cavity. At 1 month follow-up,the BCVA had improved to 6/6, N6 with the resolution of vitreous haemorrhage. The ruptured retinal arterial macroaneurysm could be visualised at the inferotemporal arcade with the clearing of the media (Figure 4.A). On HR-OCT, the involuted macroaneuryms appeared as an ovoid well-delineated structure with a solid homogenous internal reflectivity (Figure 5)(arrowhead). The patient was monitored regularly for 6 months with monthly visits, and the BCVA remained stable at 6/6, N6 at the final follow-up.
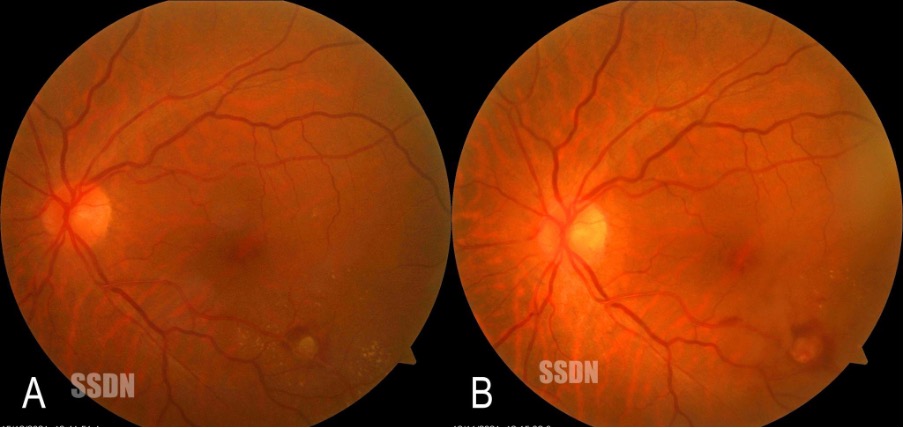
Figure 4: A) At 1-month follow-up, the subhyaloid and vitreous haemorrhage had cleared, and the ruptured RAM ( green arrow ) could be visualised at the inferotemporal arcade. B) At 2 months follow-up, the RAM had undergone involution with few specks of resolving retinal haemorrhage.
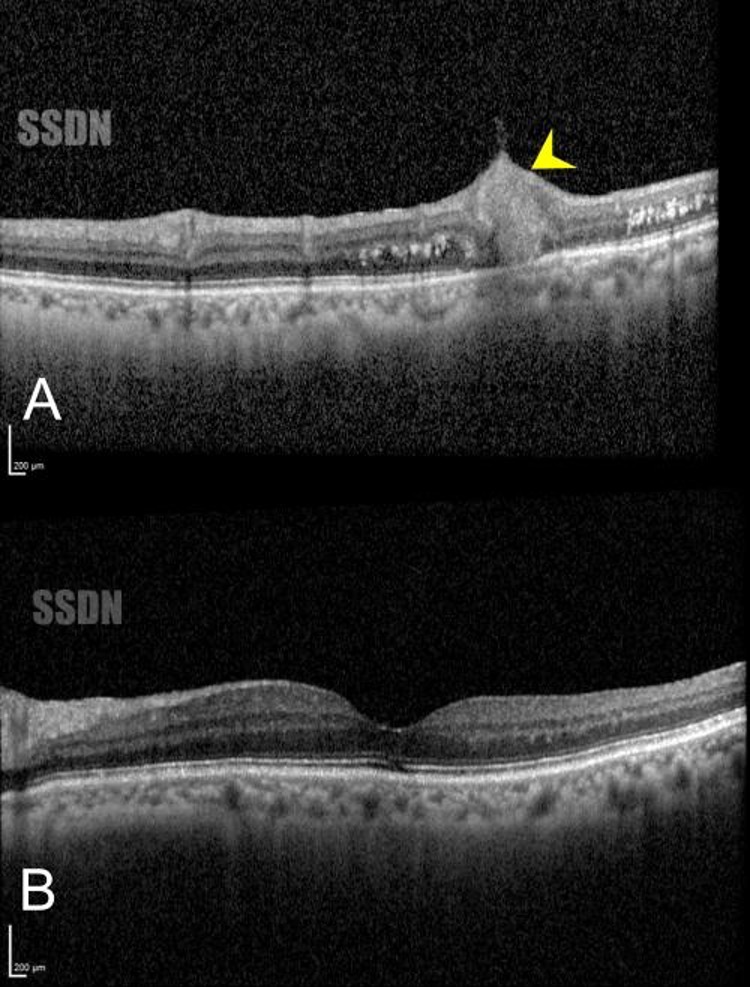
Figure 5: A) OCT scan through the ruptured RAM ( yellow arrowhead ) showing ovoid well-delineated structure with a solid homogenous internal reflectivity (arrowhead). B) OCT scan of the fovea was normal, with subtle EZ-IZ disruption noted.
DISCUSSION
Retinal Artery macroaneuryms are acquired, focal dilatations of the retinal arteries mostly affecting the second-order retinal arterioles.
Aetiology/Epidemiology
RAM is most commonly seen in the age group of 66 to 74 years, with a greater female preponderance. They are usually unilateral and solitary but may be bilateral in 10% of cases and multiple in 15-20% of cases. Systemic factors associated with RAM are hypertension, abnormal lipid profile and arteriosclerosis.
Pathophysiology
The main pathophysiology is not known yet, but it is believed to be due to the development of focal weaknesses in the arterial walls due to ageing and atherosclerotic changes.
Types of RAM:
- Hemorrhagic RAM
- Exudative RAM
- Mixed form
Clinical Features
The presentation of RAM is highly variable, and visual acuity varies depending on the location and severity of haemorrhage or exudation. Patients are usually asymptomatic, and RAMs are discovered on routine check-ups. However, patients may present with diminution of vision if haemorrhage or oedema involves the macula or in case there is a breakthrough haemorrhage with multi-layered heme or vitreous haemorrhage.
Ancillary Investigation
Fundus Fluorescein Angiography
FFA of RAM usually shows early hyperflourescence in the arterial phase. The late phase may show staining of the vessel wall and marked leakage. There may be blocked fluorescence in case of vitreous or subhyaloid or subretinal haemorrhage.
Indocyanine Green Angiography
ICG angiography is more helpful in identifying RAMs in case of dense overlying haemorrhage due to the use of infrared light. RAMs on ICGA appear as pinpoint areas of hypercyanescence in the early phase and with leakage in the late phases.
Optical Coherence Tomography
OCT scans can detect macular edema associated with exudative RAM. When the scan is directed through the macroaneurysm reveals an abnormal saccular expansion of the arterial vessel wall along with an enlarged lumen located in the inner retinal layers. OCT scans are very helpful in detecting the exact location of haemorrhage in a ruptured RAM, also delineating between subhyaloid and subILM bleed - useful guide to plan the treatment approach.
Treatment
Treatment of RAMs depends on the presentation and involvement of the disease.
Observation
In case of haemorrhage or exudation that doesn’t involve the macula, patients can be observed with follow-up at 1 month and thereafter every 1-3 months until resolution. Asymptomatic RAM with a good visual acuity not threatening the macula can safely be observed as spontaneous involution is commonly seen in most cases. Studies have found no significant difference in the final visual outcome of such cases with either observation or treatment.
Laser photocoagulation
Laser photocoagulation can be performed in selected cases of RAM with focal exudation or haemorrhage. The laser is directed over the macroaneurysm with long-duration burns to hasten the involution and decrease exudation.
Intravitreal Anti-VEGF
Intravitreal anti-VEGFs such as bevacizumab / Ranibizumab can be given in cases of macular oedema associated with RAM. Anti-VEGF injections also help in the faster involution of RAM lesions.
Pars Plana Vitrectomy
PPV can be considered in cases with non-clearing vitreous or SUBILM bleeds involving the macula. It can also be done in a few cases with dense premacular haemorrhage to reduce the chances of epiretinal membrane formation and the toxic effects on the retina.
Nd: Yag Hyaloidotomy
In the presence of fresh onset subhyaloid haemorrhage, Nd: YAG hyaloidotomy can be performed to hasten the visual recovery. The laser is directed at the posterior hyaloid membrane in the most dependent part to enable the dissipation of the subhyaloid haemorrhage into the vitreous, thereby facilitating its clearance.
Pneumatic Displacement
In cases of submacular haemorrhage, pneumatic displacement using perflouropropane or sulfur hexafluoride can be used Pneumatic displacement is facilitated by prone positioning to displace the submacular haemorrhage away from the macula, thereby hastening visual recovery and reducing complications arising due to the presence of subretinal blood.
Submacular Surgery
Submacular surgery with or without tissue plasminogen activator along with gas tamponade is indicated at times with a clotted or dehemoglobinized organized heme at submacular region where the submacular space is accessed by a retinotomy followed by drainage of the accumulated blood.
Retinal Arterial Macroaneurysm |
|
|
Etiology
|
Signs
|
|
Symptoms
|
Differentials
|
|
Investigations
|
Treatment
|
References
- Rabb M, Gagliano D, Teske M. Retinal arterial macroaneurysm.Surv Ophthalmol. 1988;33:73-96.
- Panton RW, Goldberg MF, Farber MD. Retinal arterial macroa-neurysms: risk factors and natural history. Br J Ophthalmol.1990;74:595-600
- Han Joo Cho, Taek Kwan Rhee, Hyoung Seok Kim, Jung Il Han, Dong Won Lee, Sung Won Cho, Jong Woo Kim. Intravitreal Bevacizumab for Symptomatic Retinal Arterial Macroaneurysm. American Journal of Ophthalmology. 2013;155:898-904.
- Ashley M. Speilburg, Stephanie A. Klemencic. Ruptured retinal arterial macroaneurysm: Diagnosis and management. Journal of Optometry. 2014;7:131-137.
- Emily Y. Chew, Robert P. Murphy. Acquired Retinal Macroaneurysms. Ryan’s Retina (2018). Elsevier.