Conjunctiva is a fine, translucent mucous membrane that joins and covers the anterior surface of eyeball and posterior side of the eyelids. It covers the posterior surface of the lids and reflects to cover the anterior part of the sclera, then becomes continuous with the corneal epithelium. At the lidmargin conjunctiva is continuous with the skin.
The name “conjunctiva” has originated from the term “conjoin” which means “to join”
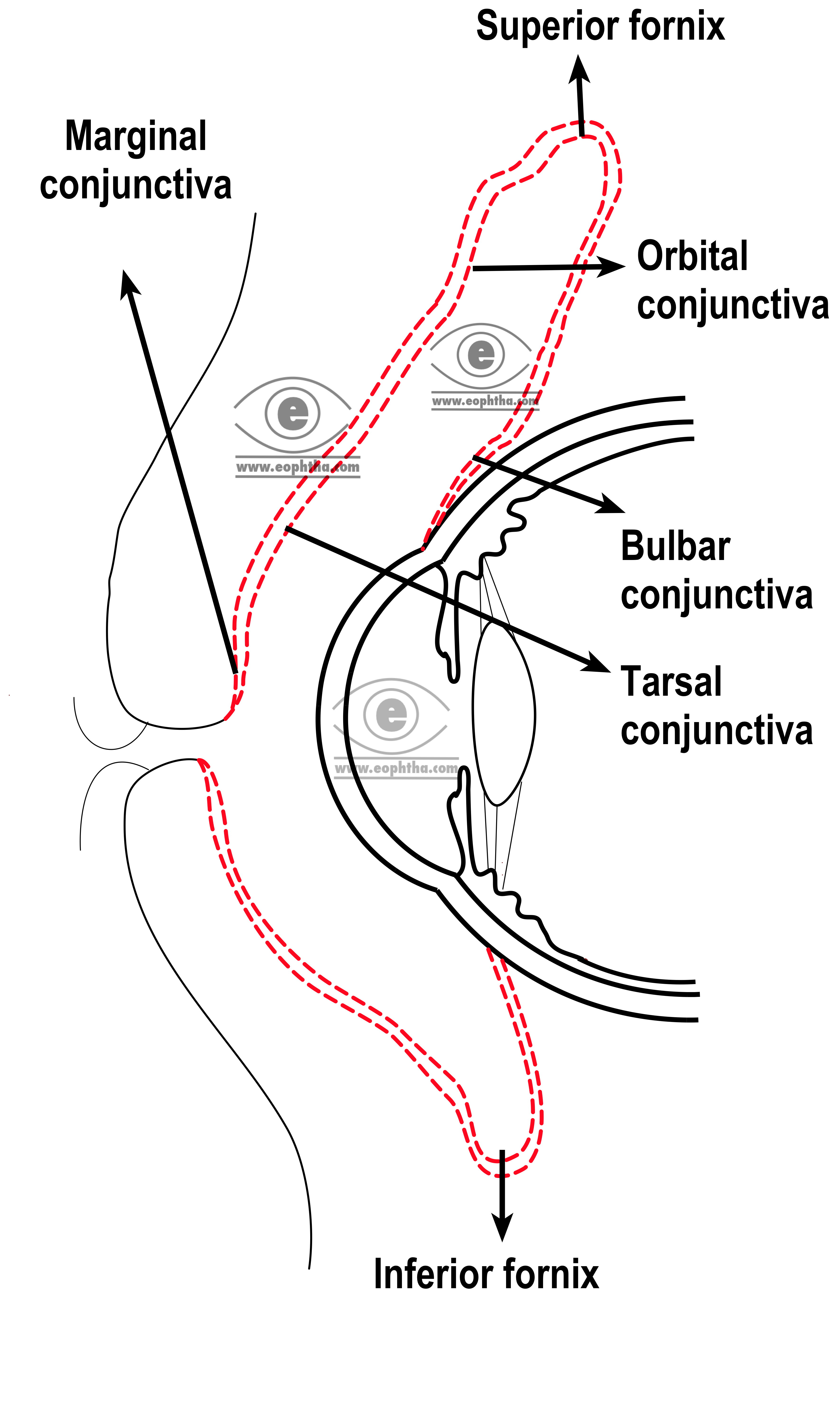
Parts of the conjunctiva:
Broadly conjunctiva is divided into palpebral conjunctiva, fornices, and bulbar conjunctiva.
Palpebral conjunctiva:It is the part of the conjunctiva that lines the undersurface or posterior surface of the eyelid.
Latin wordpalpebraemean “an eyelid”
The palpebral conjunctiva is again subdivided into marginal conjunctiva, tarsal conjunctiva, and orbital conjunctiva. The marginal conjunctiva is a transitional zone between the skin of the eyelid and the conjunctiva proper. It starts from the intermarginal strips of the eyelid as a continuation of the skin. It is made up of stratified epithelium. Marginal conjunctiva continues into the back or posterior surface of the lid for a short distance of 2 mm, up to a shallow groove or fold, where it merges with the conjunctiva proper. This groove is called sub tarsal sulcus or sulcus subtarsalis.
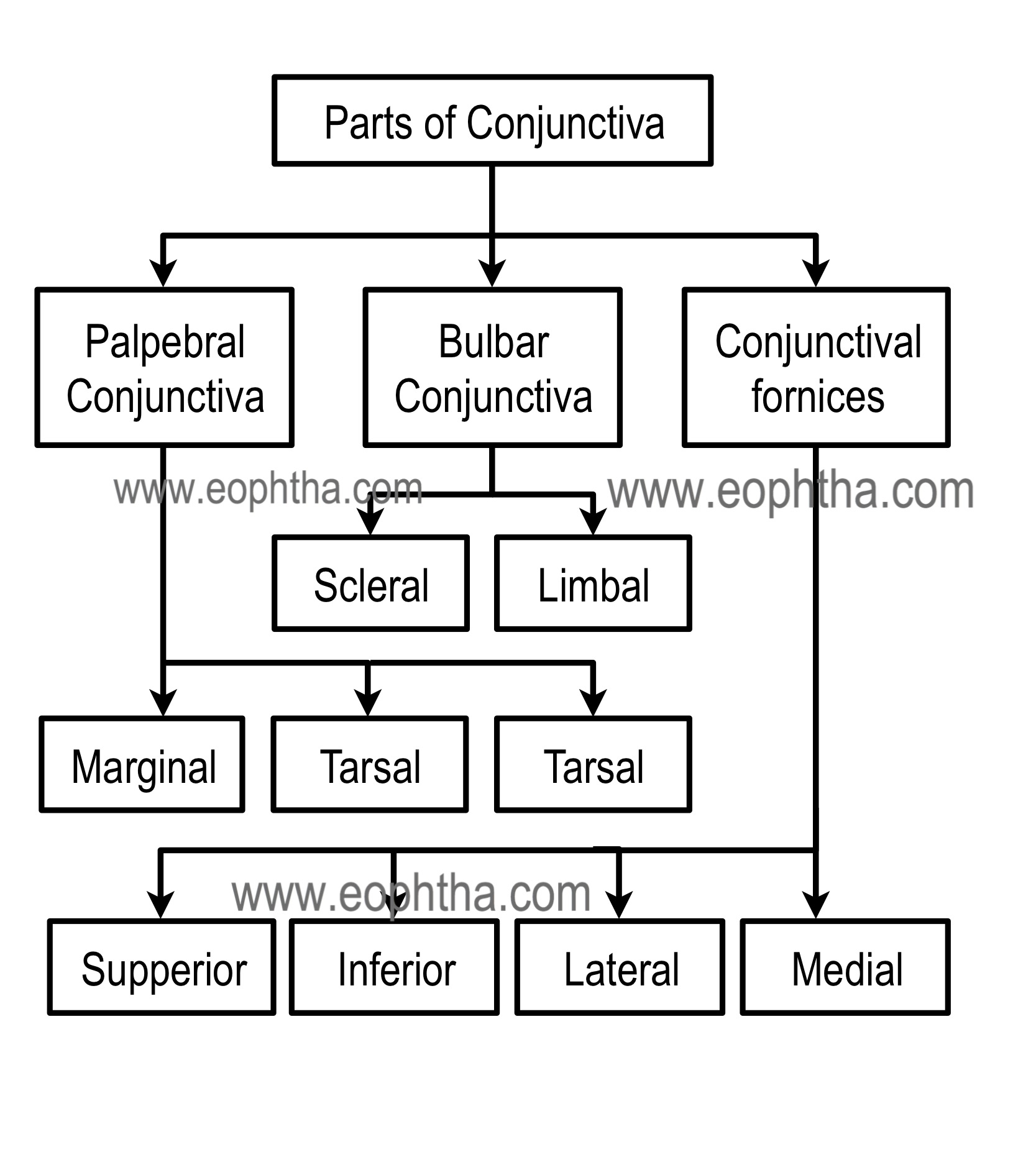
Sulcus subtarsalisorsubtarsal sulcusis a groove situated 2 mm away from lid margins. This groove is a common site of foreign body lodgment. Here perforating branches of marginal arcade pierce the tarsal plate to supply the conjunctiva.
Tarsal conjunctiva is very vascular and adherent to the tarsal plates. Adherence is less marked in lower than the upper eyelid where it is fully adherent to the whole tarsal plate. Tarsal glands are visible through the transparent tarsal conjunctiva as a yellow line running parallel to each other in a vertical direction. The orbital conjunctiva is loosely covering between the tarsal plate and fornix. It is thrown into horizontal folds during eye movements. In the upper eyelid, it lies over Muller’s muscle.
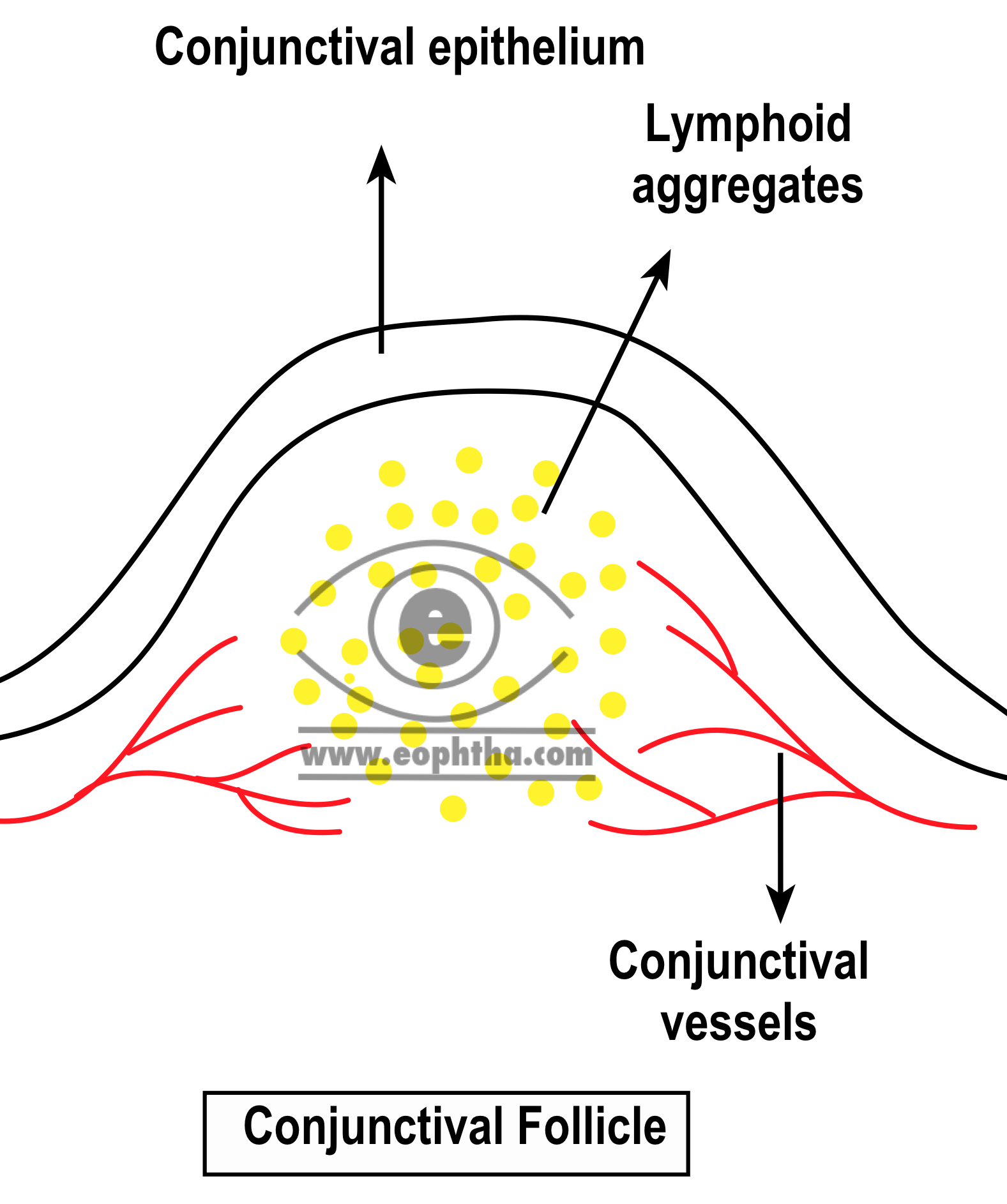
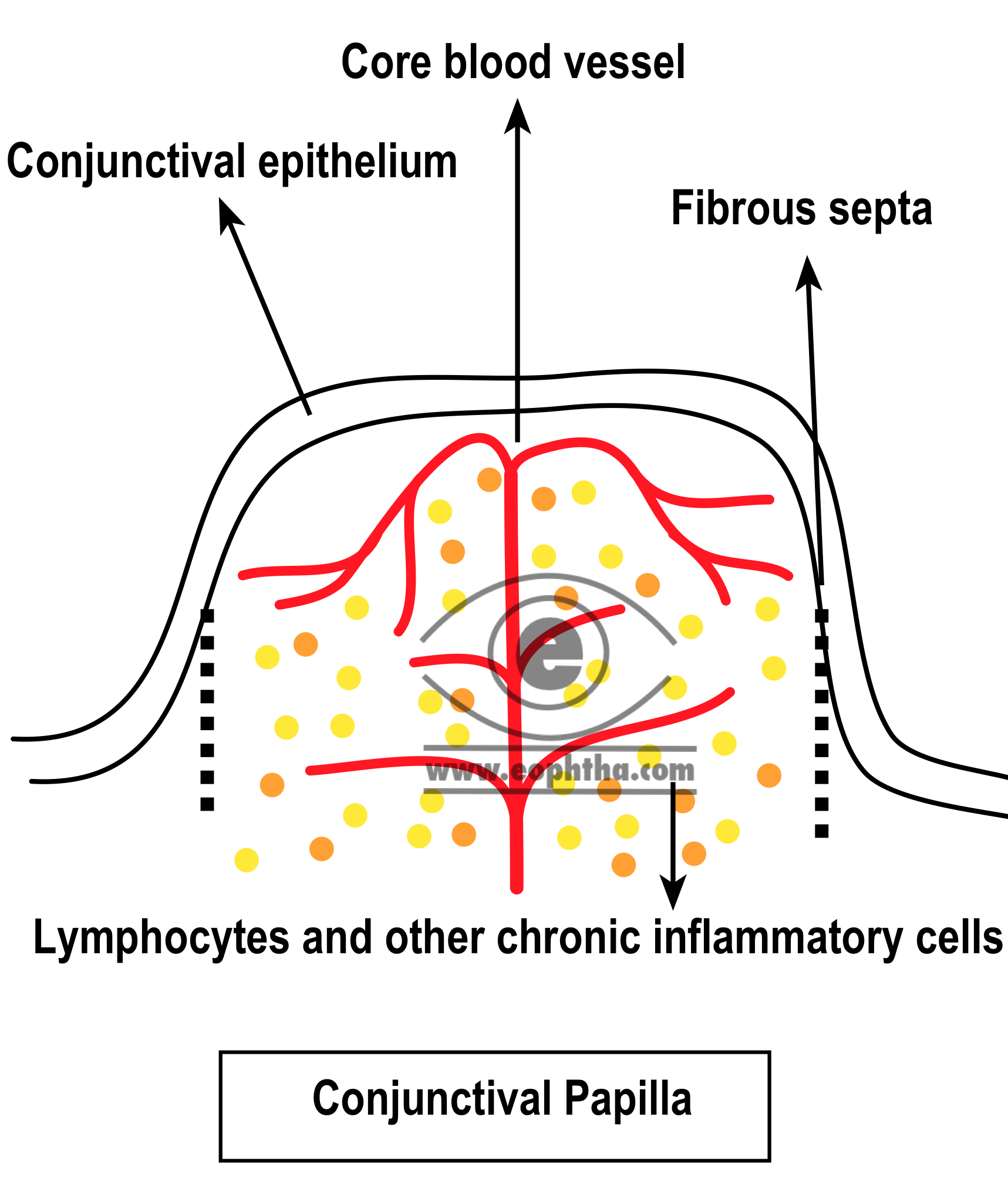
Folliclesandpapillaeare seen in the palpebral part of the conjunctiva. The palpebral conjunctiva is an area where reactive pathology of the conjunctiva may be seen clinically. There are two types of changes that can occur in this region: follicle formation and papilla formation.
Follicles are thought to be identical to lymphoid follicles found elsewhere in the body. Follicle formation is characteristic of viral and chlamydial infections as well as toxic conjunctivitis due to the application of certain topical medications.Papillaeare composed of chronic inflammatory cells such as lymphocytes and plasma cells and are distinguished from follicles by the presence of blood vessels at their center. Giant papillae are found in certain allergic diseases (e.g., vernal catarrh)and after long-term use of contact lenses, keratoprostheses, ocular post enucleation prostheses, and cosmetic shells.
Conjunctiva of the Fornix:It is fold lining the cul-de-sac formed by conjunctiva covering the posterior surface of the lids to the conjunctiva covering the anterior surface of the globe. The conjunctiva here is comparatively thicker and loosely attached in order to allow free movement of the globe. It is divided into 4 regions
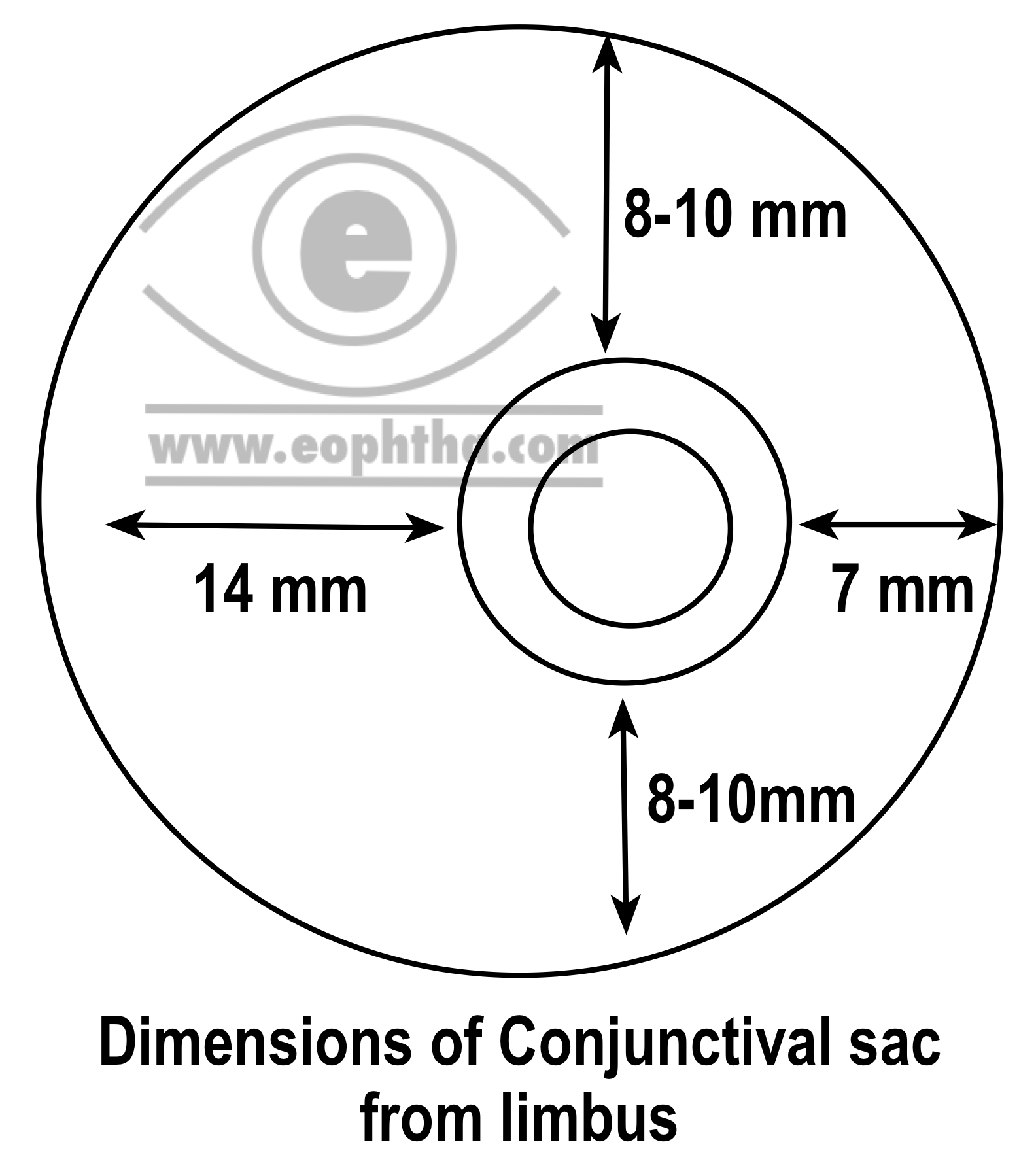
- Superior fornix lies between the upper lid and the globe. It extends 8 to 10 mm from the upper border of the limbus.
- Inferior fornix lies between the lower lid and the globe. It extends up to a distance of 8 mm below the lower part of the limbus.
- Lateral fornix lies between the lateral canthus and the globe. It extends for a distance of 15 mm form the lateral part of the limbus.
- The medial fornix is the shallowest and contains the caruncle and the plica semilunaris.
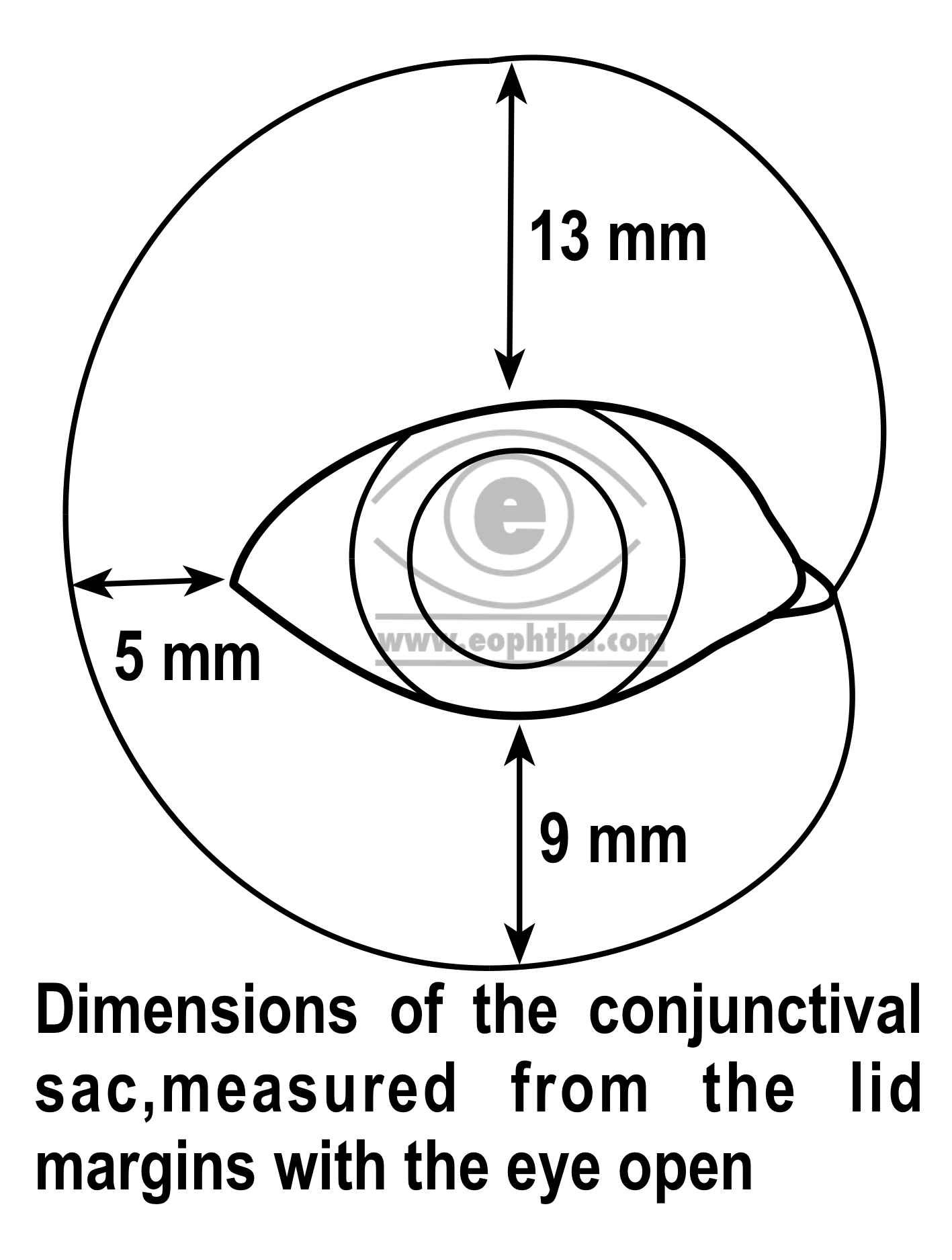
Conjunctival sac:The conjunctiva while lining the structures like the posterior part of the lids and anterior part of the globe forms a sac that opens at the palpebral fissure. The conjunctival sac contains about 7µl of tear fluid but has the capacity to accommodate fluid up to 30 µl.
Bulbar conjunctiva:It is the thinnest of all the parts of the conjunctiva and so transparent that underlying white sclera and vessels are seen clearly. It is loosely attached except for a zone of 3mm near the limbus and near insertions of the recti muscles. Limbal conjunctiva is the part of the bulbar conjunctiva which covers the limbal region and fuses with the corneal epithelium.
In limbus, conjunctiva, tenon’s capsule and sclera fuse together. As the conjunctiva in this region is less mobile, a firmer hold of the globe can be obtained with the help of forceps at the time of surgery.
The microscopic structure of conjunctiva:
Microscopically conjunctiva consists of three layers- epithelium, adenoid layer, and a fibrous layer.
1. Conjunctival Epithelium:
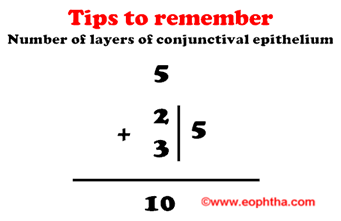
At the junctions of the skin of the lids and marginal conjunctiva (mucocutaneous junction), keratinized squamous epithelium of the epidermis transforms into the nonkeratinised squamous epithelium of conjunctiva. Morphology of conjunctival epithelium varies from region to region. The different regions of the conjunctiva and their epitheliums are described below.
|
Conjunctiva |
Number of layers |
Cells in the layers |
|
Marginal |
5 layers of 5 layered non-keratinized stratified squamous epithelium |
Superficial layer: Squamous cells |
|
Middle three layers: Polyhedral cells |
||
|
Deepest layer: Cylindrical cells |
||
|
Tarsal |
2 layers of Stratified cuboidal epithelium |
Superficial layer: Cylindrical cells |
|
Deepest layer: cuboidal cells |
||
|
Fornix and bulbar |
3 layers of Stratified, squamous epithelium |
Superficial layer: Cylindrical cells |
|
Middle layer: polyhedral cells |
||
|
Deepest layer: Cuboidal cells |
||
|
Limbal |
10 layers of stratified squamous epithelium |
Superficial layer: squamous cells |
|
Middle layer: polygonal cells |
||
|
Basal- cubical |
The lid margins are covered anteriorly by dry, keratinized epithelium, which merges into the moist, nonkeratinized epithelium posteriorly covering the tarsus. In many ocular surface disorders, the normal epithelium is modified and becomes nonsecretory and keratinized. This pathologic transition is called squamous metaplasia.
Goblet cells:Goblet cells are seen throughout the conjunctiva lying in between the cells of the conjunctival epithelium. These cells are actually unicellular glands which secret mucin. They are believed to arise from the basal layer of epithelium. They gradually enlarge, become larger as they reach the surface of the conjunctiva. On reaching the surface they discharge their mucin content and finally shed away. These cells are round and oval in shape and 10-20 µm in size.
These cells are called goblet cells because of their goblet-like shape. Goblet is footed cup intended to hold a drink. It is intended for drinking during a ceremony. In the ultramicroscopic examination, apical portion of the cell is shaped like a cup, as it is distended by a large number of mucin granules whereas its basal portion is shaped like a stem for lack of these granules
Goblet cells may produce up to 2.2 mL of mucus daily. Mucus is essential for ocular surface integrity as it lubricates and protects the epithelial cells. Mucin reduces the surface tension of the tear film to ensure its stability.
Melanocytes:Melanocytes are primarily seen in the limbus, fornix, plica semilunaris, caruncle and at the sites of perforation of the anterior ciliary vessels. Sometimes they give the conjunctiva a brownish tinge.
Langerhans cells:Langerhans cells are actually dendritic cells, immune cells that form part of the immune system. Their main function is to process antigen material and present it on the surface to other cells of the immune system. Thus they function as antigen-presenting cells. The highest density of Langerhans cells has been found in tarsal conjunctiva followed by fornix and bulbar conjunctiva. The number of cells decreases with age. These cells contain rod-shaped or "tennis-racket" shaped cytoplasmic organelles known as Birbeck granule, which stains positively for ATPase.
The Langerhans cell is named afterPaul Langerhans, a physician and anatomist from Germany, who discovered the cells at the age of 21 when he was a medical student.
2. Substantia propria or conjunctival submucosa:
It consists of a superficial lymphoid layer and a deeper fibrous layer. The conjunctival epithelium rests on a connective tissue layer called the substantia propria. This tissue has enormous anti-infectious potential. Numerous mast cells (6000/mm3), lymphocytes, plasma cells, and neutrophils are normally present in this layer
Lymphoid layer:
The lymphoid layer consists of many lymphocytes that are scattered to form this fine connective tissue reticulum. This layer is thickest in fornices and terminates near sulcus subtarsalis. So the marginal conjunctiva is devoid of this layer.
- Lymphoid layer is absent in newborn. This layer first appears in fornices at 3 to 4 months of age.
- Lymphocytes, primarily T lymphocytes are found abundantly in conjunctiva. They are present in substantia propria and epithelium in a ratio of 2:3.Lymphoid aggregations similar to mucosal associated lymphoid tissue (MALT) found in gut and bronchi, are also seen in conjunctiva. These lymphoid aggregations which consist of T & B lymphocytes are known as conjunctiva associated lymphoid tissue (CALT).
Mast cells:
Mast cells are granulocytic cell-like basophils. The conjunctiva contains a high number of mast cells in substantia propria. The total number of mast cells in the conjunctiva and adnexal tissue will be around 50 million. Allergic conjunctivitis is a typical mast cell-mediated hypersensitivity reaction. In patients with allergic conjunctivitis, the mast cells have been found in conjunctival epithelium also.
The surface of the mast cell is coated with IgE antibody. There are about 10000 to 50000 IgE receptors in one mast cell of which 16% are occupied. Exposure of appropriately sensitized IgE coated mast cell to an airborne allergen is the initiating stimulus for the drama of allergy. The allergen binds to two separate IgE molecules creating a dimer that initiate a chain of reactions in the mast cell plasma membrane, and the mast cell membrane ruptures leading to extrusion of the contents of the cell to the surrounding tissue. The contents of the mast cell act like mediators of allergic reactions. These mediators are histamine, prostaglandin, eosinophilic granule major basic protein, eosinophil chemotactic factor, platelet activating factor. These mediators and many other cell mediators stimulate the proliferation of fibroblasts and recruitment of many cell types in the conjunctiva. These events play an active role in development of papillae in patients with VKC.
3. Fibrous layer:
This layer contains the vessels and nerves of conjunctiva and glands of Krause. Except for the tarsal part of conjunctiva, where it is very thin and blends with the tarsal plates, the fibrous layer is thicker than the lymphoid layer.
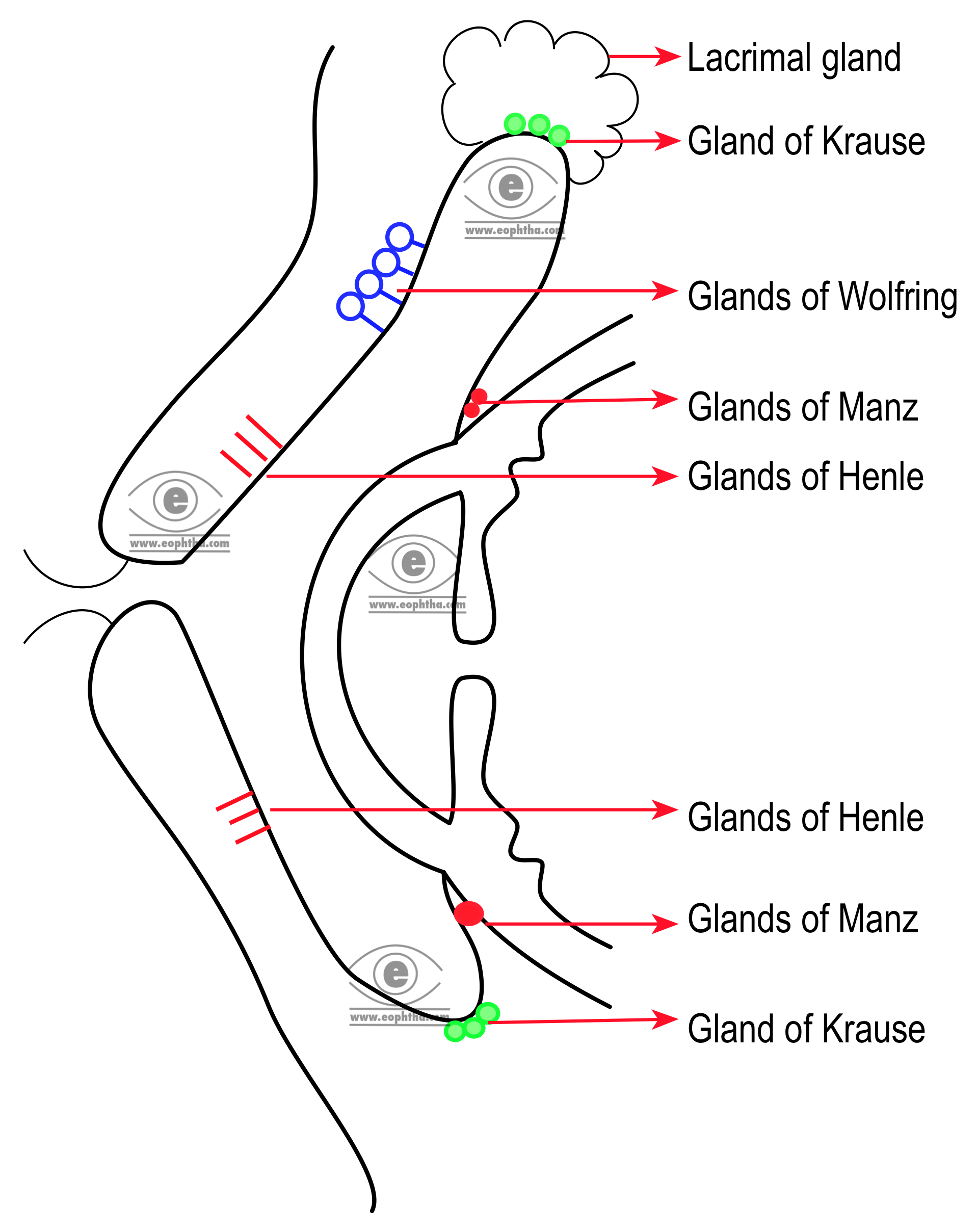
Accessory lacrimal glands:
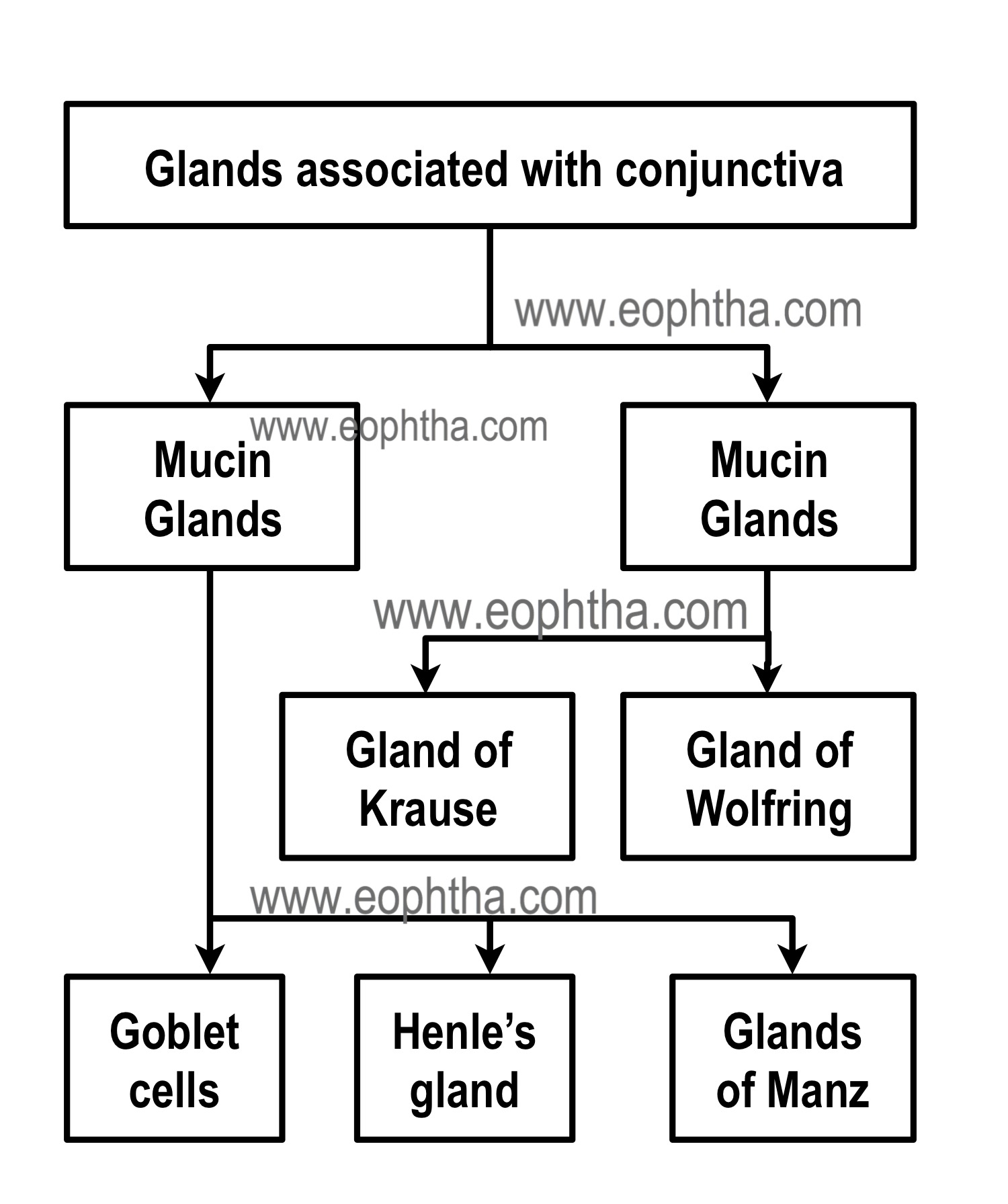
Glands of Krause:The glands of Krause lie in deep subconjunctival tissue of the upper and lower fornices. They are about 42 in number in the upper fornix and 6 to 8 in the lower fornix. In the upper fornix, they lie between the palpebral part of the lacrimal gland and the tarsal plate. Microscopically structures of these glands are similar to main lacrimal glands. Their ducts unite to form a long duct which opens into the fornix.
Glands of Krause is named after German anatomistCarl Friedrich Theore Krause. Interestingly, his son, Wilhelm Krause’s name is eponymously associated with “end-bulbs of Krause”, a cutaneous receptor found in conjunctiva, lips, tongue and genitals.
Glands of Wolfring or Ciaccio:Glands of Wolfring are larger than the glands of Krause. There are 2 to 5 in the upper lid and 1-3 in the lower lid.
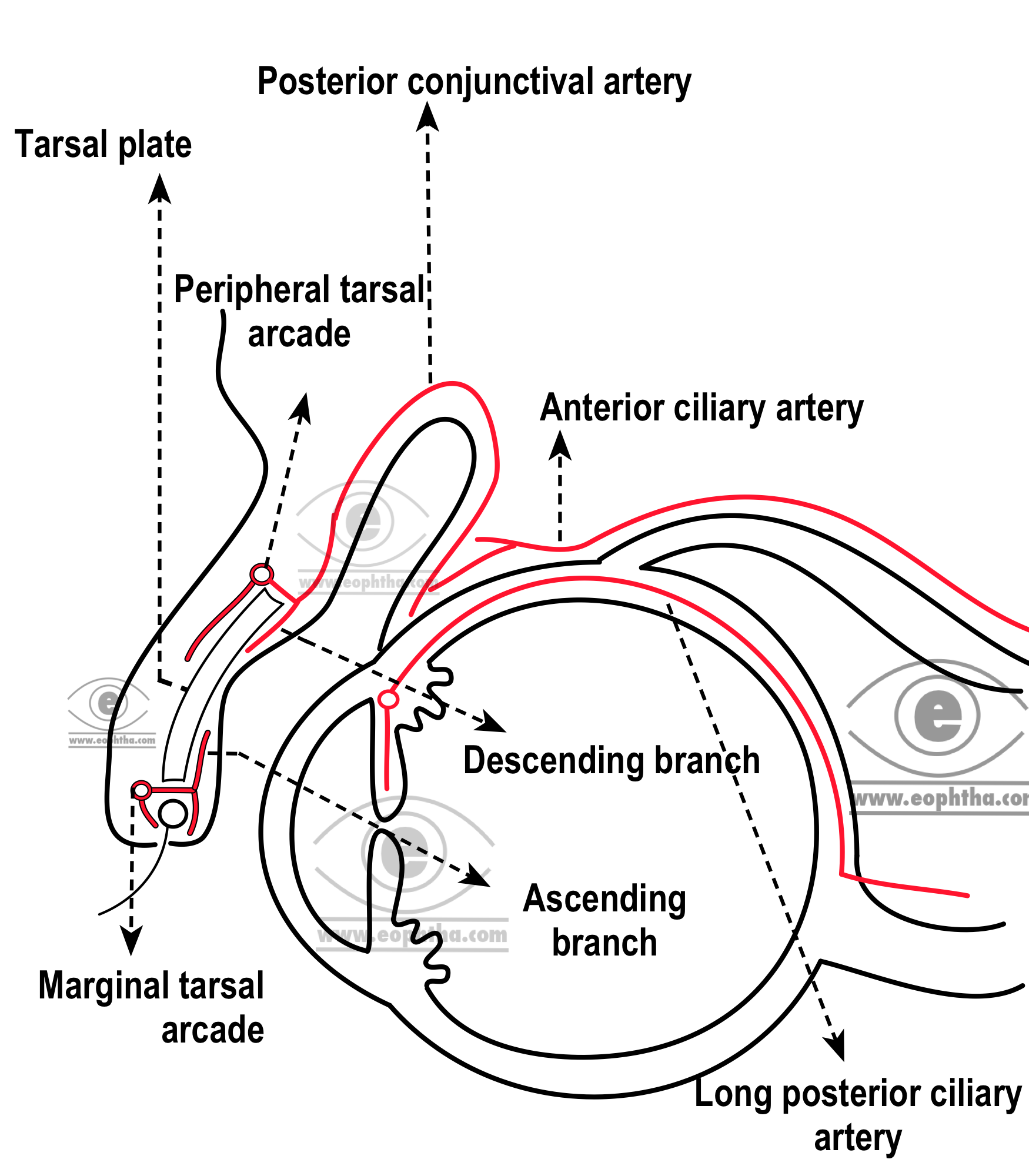
Blood supply of Conjunctiva:
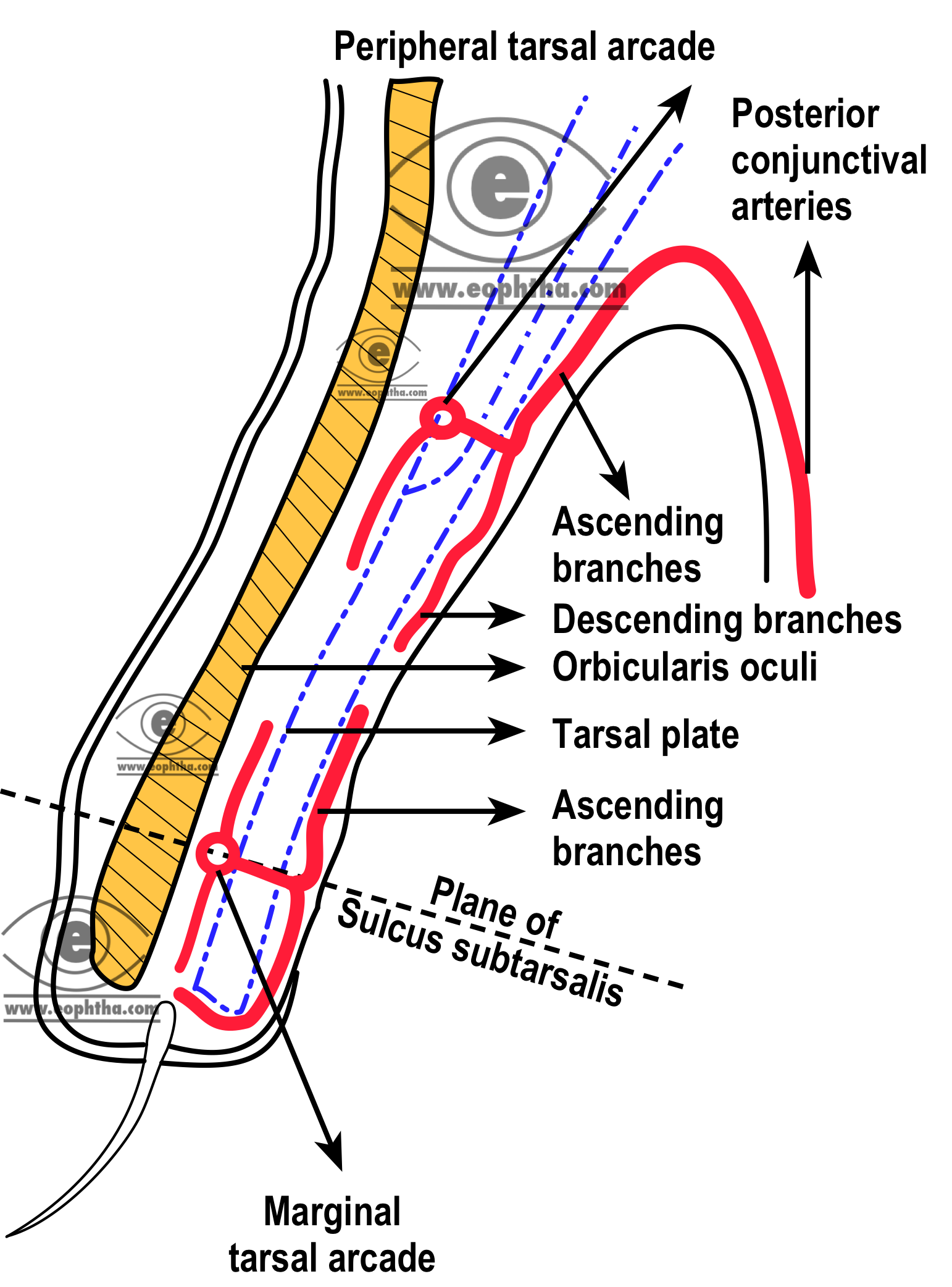
Arterial supply of conjunctiva derives from (1) peripheral Tarsal arcades, (2) marginal Tarsal arcades (3) The anterior ciliary arteries
Bulbar conjunctiva is the only tissue in body, where constituent blood vessels are visible
Palpebral arcades:There are two palpebral arcades which are the major source of the blood supply of conjunctiva. These are marginal tarsal arcade & peripheral tarsal arcade. Marginal tarsal arcades are larger than peripheral tarsal arcade. The medial and lateral palpebral branches of the nasal and lacrimal arteries of the lid supply the eyelid. (Lateral palpebral arteries are the branches ofLacrimal arteries and medial palpebral arteries derive separately or together from the main ophthalmic artery or dorsal nasal arteries). The superior and inferior branches from these arteries enter the eyelid by piercing orbital septum. Each branch of the medial palpebral artery then anastomoses with corresponding lateral palpebral artery and this is how they form the marginal arcade.
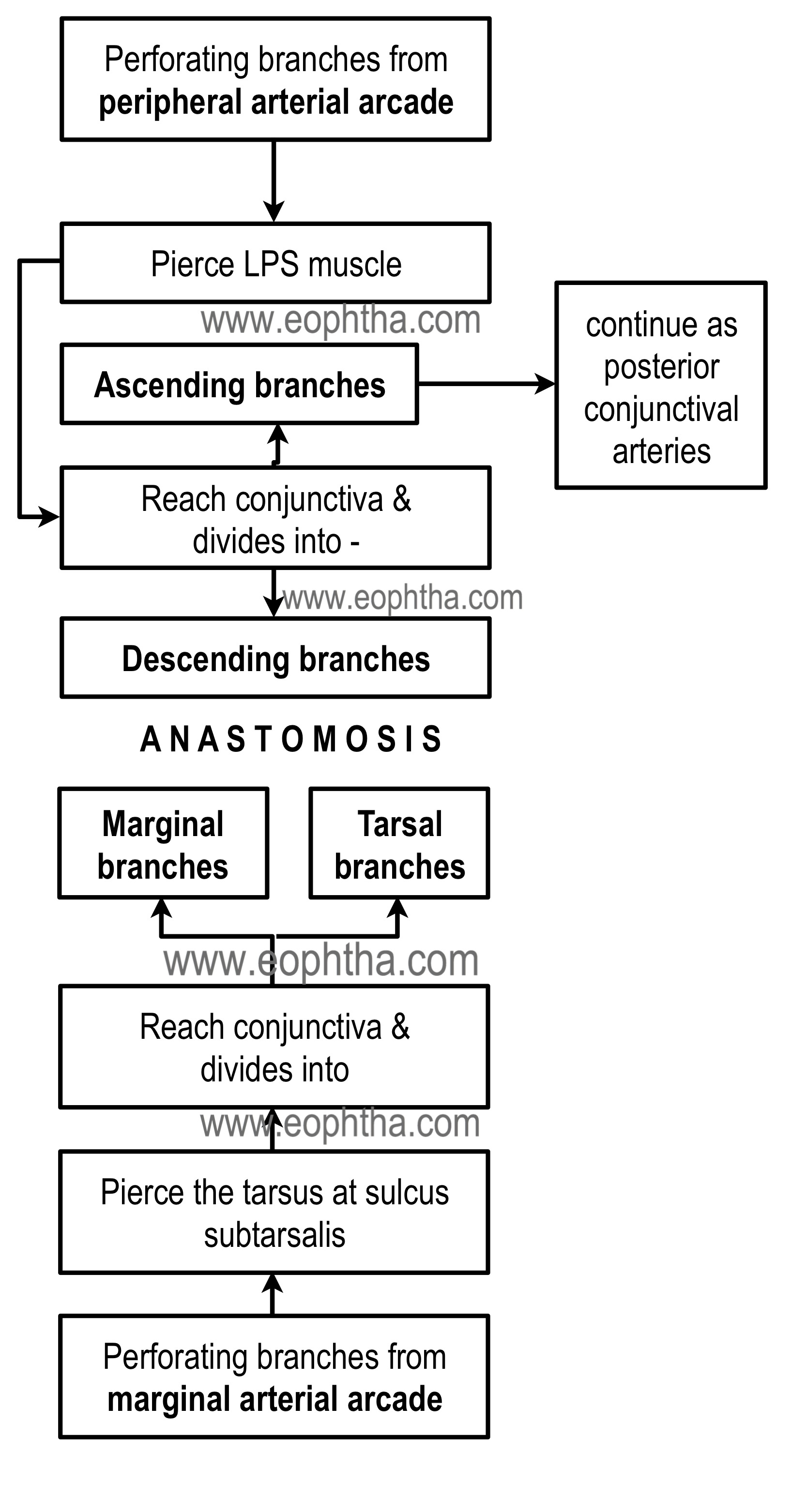
Marginal Arcade:Marginal tarsal arcade lies in the submuscular plane in front of the tarsal plate, 2mm away from the margin of the eyelids. Perforating branches of the marginal tarsal arcade pierce the tarsal plate at the region of sulcus subtarsalis and enter the conjunctiva to supply the palpebral part of the conjunctiva.
Marginal arcade lies in close proximity to the lid margin & peripheral tarsal arcade lies near the peripheral marginal arcade
Peripheral marginal arcade lies near the peripheral border of the tarsal plate. Peripheral tarsal arcade is formed by the superior branch of the medial palpebral artery, in front of the upper margin of the tarsal plate. Perforating branches of the peripheral tarsal arcade pierce the Mullers muscle, reach the conjunctiva and give off two branches –ascending and descending. Descending branches supply the tarsal conjunctiva and also anastomoses with vessels from the marginal arcade and ascending branches pass into the superior fornix to continue around the fornices to the bulbar conjunctiva as the posterior conjunctival arteries.
The anterior ciliary arteries travel along the tendon of the rectus muscles and give off anterior conjunctival arteries just before piercing the eyeball. The anterior ciliary arteries send branches to the pericorneal plexus and to the surrounding regions of the bulbar conjunctiva in the limbal area.
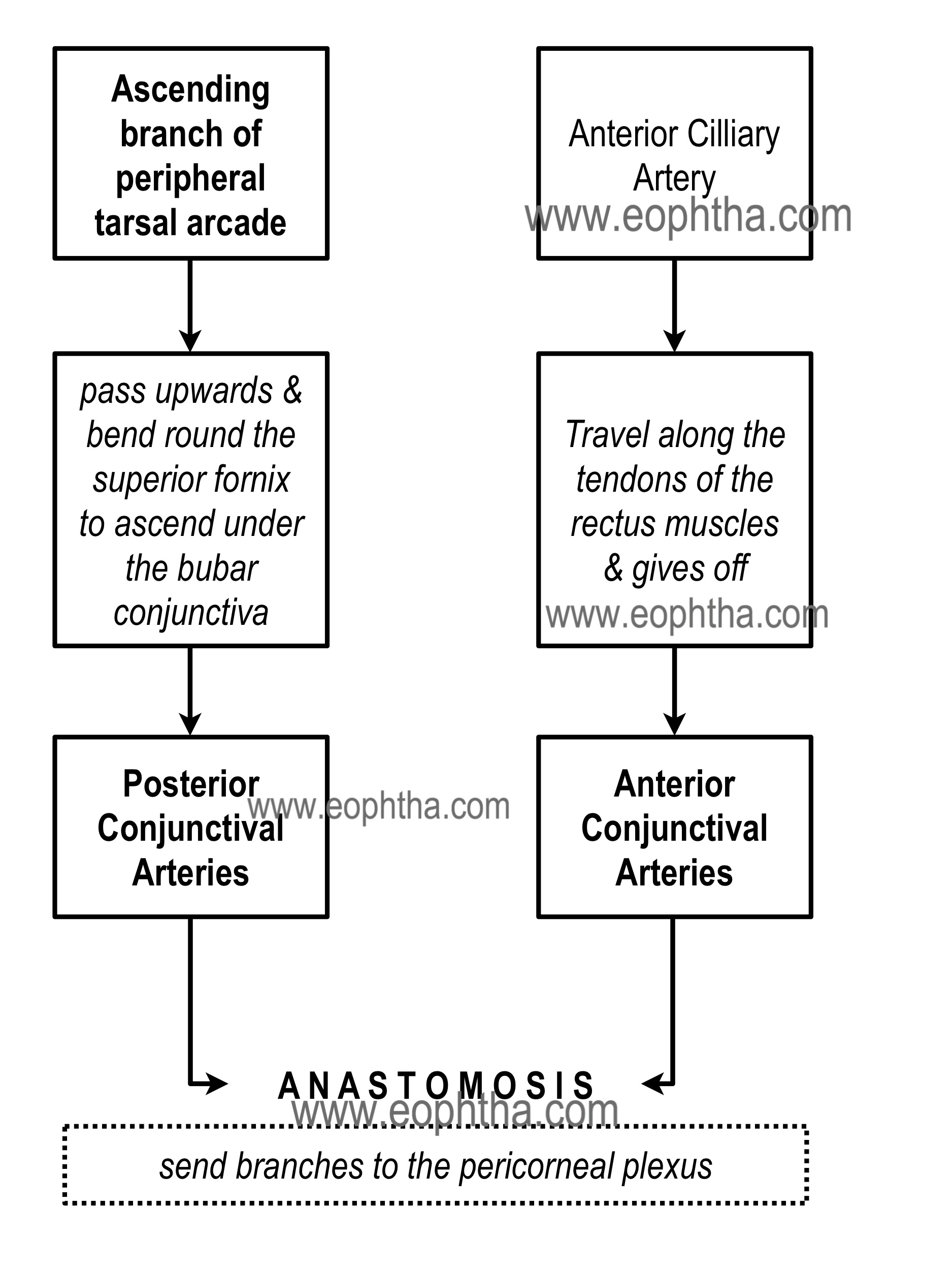
Free anastomosis occurs in this area between the anterior conjunctival vessels and the terminal branches of the posterior conjunctival vessels. Thus, the superficial and deep systems of vessels are closely connected in the limbal area. Clinically, this is an area of diagnostic importance. The superficial posterior vessels become engorged during inflammation or infection to give the bulbar conjunctiva bright red appearance that fades from the fornix toward the limbus.1 In keratitis or iritis, the deeper ciliary vessels are hyperemic, which leads to a characteristic circumcorneal injection that blanches with pressure.
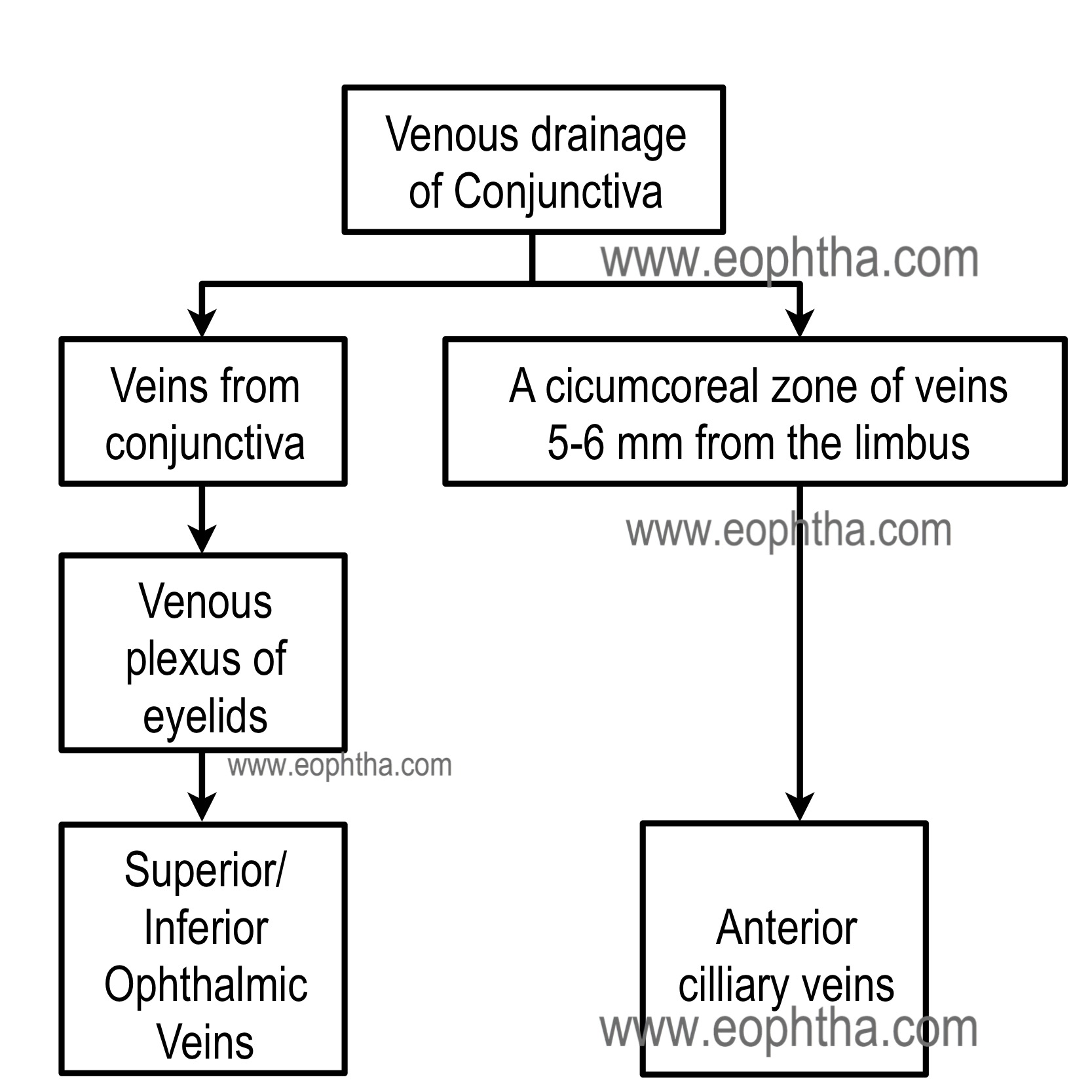
The venous supply of conjunctiva is summarized in the figure below. The conjunctival veins are more in number than conjunctival arteries.
The nerve supply to the conjunctiva is derived from the first division of the trigeminal nerve. The nerves to the lid supply most of the conjunctiva. These nerves comprise the infratrochlear branch of the nasociliary nerve, the lacrimal nerve, the supratrochlear and supraorbital branches of the frontal nerve, and the infraorbital nerve from the maxillary division of the trigeminal nerve. The limbal area is supplied by branches from the ciliary nerves. All nerves form a network in the conjunctiva and terminate either peripherally in various forms of specialized endings or on blood vessels and epithelial cells. The majority of nerve endings in the conjunctiva are free, unmyelinated nerve endings. They form a sub-epithelial plexus in the superficial part of the substantia propria. Many of these fibers end on blood vessels, and others form an intraepithelial plexus around the base of epithelial cells and send free nerve endings between cells.
|
Part of conjunctiva |
Blood supply |
Nerve supply |
|
Palpebral Conjunctiva, Tarsal Conjunctiva |
Marginal tarsal arcade and descending branches of the peripheral tarsal arcade |
Superior: Supraorbital, supratrochlear, infratrochlear, and lacrimal nerves Inferior: Lacrimal and infraorbital nerves |
|
Fornices |
Peripheral tarsal arcade |
Superior: Supraorbital, supratrochlear, infratrochlear, and lacrimal nerves Inferior: Lacrimal and infraorbital nerves |
|
Bulbar |
Anterior conjunctival and posterior conjunctival arteries |
Ciliary nerves |
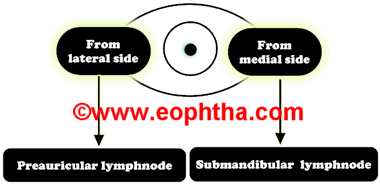
Lymphatics
Lymphatics in the palpebral region drains into the lymphatics of eyelids. In bulbar conjunctiva, lymphatics from lateral side drain into the superficial preauricular lymph nodes & lymphatics from medial side drain to deep submaxillary nodes.