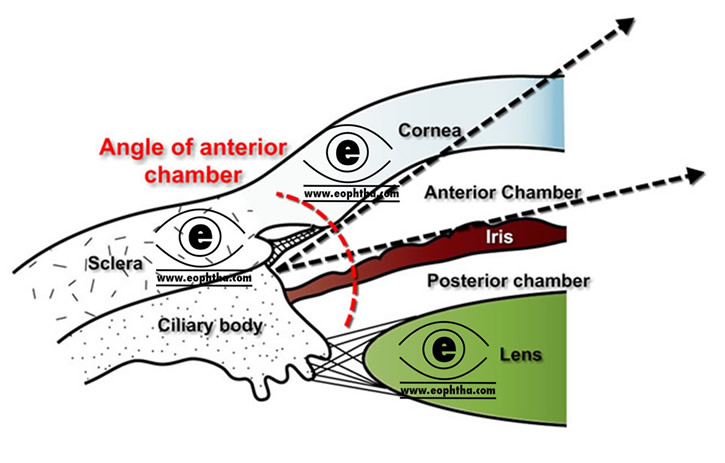
Anterior chamber is an angular space bounded anteriorly by the posterior (inner) surface of the cornea and posteriorly by the anterior surface of the iris and a part of cilliary body.
Boundary of anterior chamber:
|
Anteriorly |
Posteriorly |
|
Inner surface of the cornea |
Lens, |
Anterior chamber is 3 mm deep and it contains 0.25 ml of the aqueous humour. Anterior chamber depth is shallower in the hypermetropic eye than the myopic eye. It is also shallower in children and in older people.
Anterior Chamber at a glance
- Volume: 220 µL.
- Chamber Volume decreases by 0.11 µL/year life
- Depth: 3.15mm (2.6- 4.4mm)
- Chamber depth decreases by 0.01mm/year of life.
- Chamber depth is shallower in the hypermetropic than myopic .Chamber deepens by 0.06mm for each diopter of myopia.
- Chamber depth is slightly diminished during accommodation, partly by increased lens curvature & partly by forward translocation of the Lens.
- Wide angle of anterior chamber denotes the eye in which the angle between iris and surface of the trabecular meshwork is between 20 to 45 degrees. Angles less than 20 degrees are termed as narrow angles.( Becker- Shaffer's diagnosis and therapy of glaucomas)
Parts of anterior chamber:
Scleral sulcus and scleral spur:
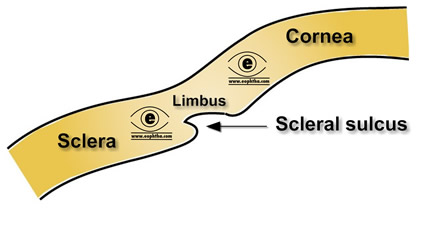 Limbus is the transition zone between the cornea & sclera. On the inner surface of the limbus, there is an indentation or groove, which isknown as the scleral sulcus. This scleral sulcus has a sharp posterior margin- the scleral spur & a sloping anterior wall which extends to the peripheral cornea.The ciliary body is attached to the scleral spur and there exists a potential space, the supraciliary space, between ciliary body and the sclera. Iris inserts into the anterior side of the ciliary body and the part of the ciliary body between root of iris & scleral spur is known as ciliary band.
Limbus is the transition zone between the cornea & sclera. On the inner surface of the limbus, there is an indentation or groove, which isknown as the scleral sulcus. This scleral sulcus has a sharp posterior margin- the scleral spur & a sloping anterior wall which extends to the peripheral cornea.The ciliary body is attached to the scleral spur and there exists a potential space, the supraciliary space, between ciliary body and the sclera. Iris inserts into the anterior side of the ciliary body and the part of the ciliary body between root of iris & scleral spur is known as ciliary band.
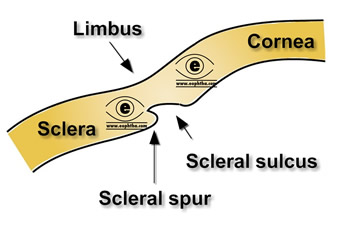 Scleral spur is composed of a group of fibres known as scleral roll. Scleral roll is composed of 75-80% collagen + 5% elastic tissue. This circular structure prevents ciliary muscle from causing Schlemm’s canal to collapse.
Scleral spur is composed of a group of fibres known as scleral roll. Scleral roll is composed of 75-80% collagen + 5% elastic tissue. This circular structure prevents ciliary muscle from causing Schlemm’s canal to collapse.
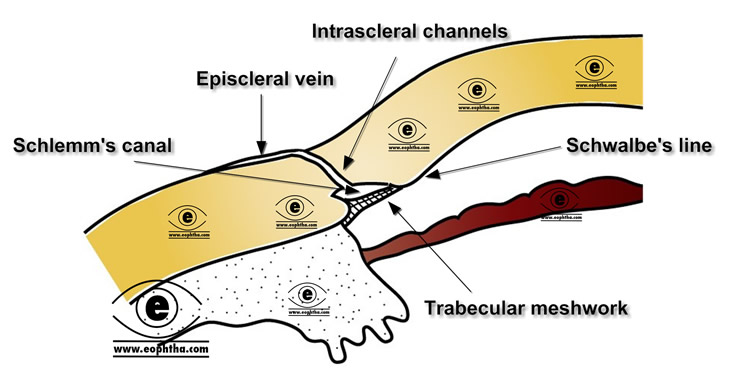
Canal of Schlemm:
A sieve or net like structure, the trabecular meshwork, bridges the scleral sulcus converting it into a tube, which is known as schlemm’s canal. It is a circular canal with a diameter of 190 to 350 microns, in the sclera which lies posterior to the sclerocorneal junction.as mentioned, it can be compared with a tube situated in side the sclera surrounding limbus. Though rarely there can be a plexus rather than a discrete canal. It is also called sinus venous sclerae. On cross section it is oval in shape and lined by endothelium. It communicate with anterior chamber through the trabecular meshwork internally. On the scleral side the c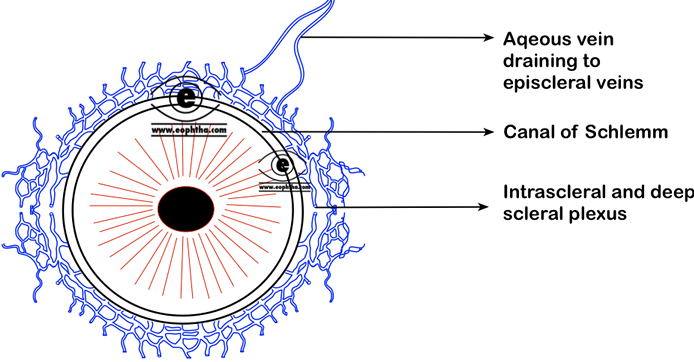 anal of Schlemm is perforated by approximately 25 to 30 aqueous collector channels which branch into intrascleral and deep scleral plexi. In conventional route of outflow, aqueous moves into the canal of Schlemm through trabecular meshwork and from their reaches episcleral veins via collector channels that traverse limbal sclera. episcleral veins drain into the ophthalmic veins and thus in general circulations.
anal of Schlemm is perforated by approximately 25 to 30 aqueous collector channels which branch into intrascleral and deep scleral plexi. In conventional route of outflow, aqueous moves into the canal of Schlemm through trabecular meshwork and from their reaches episcleral veins via collector channels that traverse limbal sclera. episcleral veins drain into the ophthalmic veins and thus in general circulations.
Historical Perspective:
Schlemm’s canal is named after a German anatomist; Friedrich Schlemm. Interestingly, he was also the first person to describe the corneal nerves.
Remember:Canal of Schlemm is not a rigid tube and at higher intraocular pressure it often collapses. It can be opened up by a pull on the scleral spur ( exerted by longitudinal ciliary muscle fibres). Cholinergic drugs are used to facilitates the aqueous drainage by opening up the canal based on this mechanism.
Trabecular meshwork:
Trabecular meshwork is a spongy, sieve like tissue. It is roughly a triangular structure bounded anteriorly by periphery of the cornea and posteriorly scleral spur and anterior surface of the ciliary body. Trabecular meshwork is pale tan to dark-brown in colour,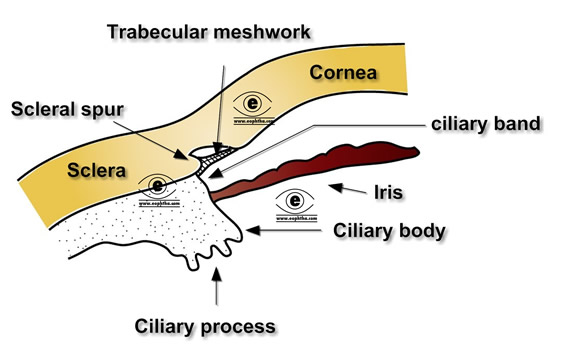 varying with pigmentation of the tissue, which is darker posteriorly.
varying with pigmentation of the tissue, which is darker posteriorly.
Trabecular meshwork can be divided into three parts.
Uveoscleral meshwork: It is the most internal part of trabeculum. It is characterised by thick band of connective tissue and large pores. These thick bands originates from iris root and extends upto Schwalbe’s line.
Corneoscleral meshwork: Corneoscleral meshwork forms the middle of the trabeculum and it is the most extensive part of this sieve like tissue. Corneoscleral meshwork extends from the scleral spur to the anterior wall of the scleral sulcus and contains elliptical openings or pores. These pores gradually reduce in size as trabecular sheets approach the Schlemm canal.
Juxtacanalicular meshwork: juxtacanalicular meshwork differs histologically from other trabecular mesh works. It is single layered amorphous tissue which is believed to provide maximum resistance to aqeous humor tissue outflow. It borders the canal of Schlemm.
Juxtacanalicular trabecular meshwork is sometimes referred to as the cribriform layer
Schwalbe’s line:
When trabecular meshwork inserts in to the periphery of cornea, a ridge is created, known as Schwalbe’s line. It also marks the prominent end of Descemet’s membrane of the cornea.
 Posterior embryotoxon: Posterior embryotoxon denotes to a condition with a prominent, anteriorly displaced Schwalbe line. On clinical examination, posterior embryotoxon appears as an irregular, white line just anterior to the limbus. Posterior embryotoxon occurs in approximately 10% of normal eyes.
Posterior embryotoxon: Posterior embryotoxon denotes to a condition with a prominent, anteriorly displaced Schwalbe line. On clinical examination, posterior embryotoxon appears as an irregular, white line just anterior to the limbus. Posterior embryotoxon occurs in approximately 10% of normal eyes.
Gonioscopy:
Gonioscooy is the examination of angle of anterior chamber. Normally structures of angle of anterior chamber is not visible through cornea because of the optical phenomenon known as total internal reflection. Because of the total internal reflection light that is reflected from the anterior chamber angle is bent internally within the cornea at the cornea–air interface and thus not visible to eyes directly. With the help of a goniolens we can eliminate this effect and place the resultant lens–air interface at a different angle and observe the light reflected from the structures of the angle.
Historical perspective:
The term "gonioscopy" was coined by Trantas, who in 1907, examined the angle of anterior chamber by indenting limbus in a patient of Keratoglobus. However credit for invention of goniolens goes to Salsman(1914)
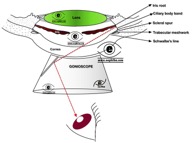 In gonioscopy, from anterior to posterior, the identifiable anterior most structure is Schwalbe's line, which appears as a thin, bright line . The second structure is trabecular meshwork which is often classified clinically to anterior and posterior. The posterior trabecular meshwork is more pigmented and appears darker than the anterior.peripheral to the trabecular meshwork, canal of Schlemm is seen, often as a red band ( if blood is present in the canal). Next visible structures are scleral spur and ciliary body band. The iris root represents the insertion of iris on the ciliary body and the ciliary body band is the part of the ciliary body visible between iris root & scleral spur. The width of the ciliary body band depends on the level of iris insertion. In myopic eyes, the iris is larger and thinner and is usually inserted more posterior on the ciliary body. Thus ciliary body band is wider in myopic eyes. On the other hand, in hyperopic eyes, the iris is thicker and its insertion is more anterior than in emmetropic eyes, resulting in a narrower ciliary body band ( also narrower angle).Click hereto visit our ophthalmic instrument section, to read more about gonioscope and others.
In gonioscopy, from anterior to posterior, the identifiable anterior most structure is Schwalbe's line, which appears as a thin, bright line . The second structure is trabecular meshwork which is often classified clinically to anterior and posterior. The posterior trabecular meshwork is more pigmented and appears darker than the anterior.peripheral to the trabecular meshwork, canal of Schlemm is seen, often as a red band ( if blood is present in the canal). Next visible structures are scleral spur and ciliary body band. The iris root represents the insertion of iris on the ciliary body and the ciliary body band is the part of the ciliary body visible between iris root & scleral spur. The width of the ciliary body band depends on the level of iris insertion. In myopic eyes, the iris is larger and thinner and is usually inserted more posterior on the ciliary body. Thus ciliary body band is wider in myopic eyes. On the other hand, in hyperopic eyes, the iris is thicker and its insertion is more anterior than in emmetropic eyes, resulting in a narrower ciliary body band ( also narrower angle).Click hereto visit our ophthalmic instrument section, to read more about gonioscope and others.
The structures seen during gonioscopy can be memorised with the help of mnemonic " I can see till Schwalbe's line" ( posterior to anterior) see ophthalmologymnemonicsection
Irregular, thread like processes arising from iris are seen in angle of anterior chamber during gonioscopy and they bridge the angle. These are known as iris processes . Usually these processes terminate near the scleral spur.
Iris processes are also called pectinate ligaments