1. Is there something we can do before ordering a visual field in neuro-ophthalmology?
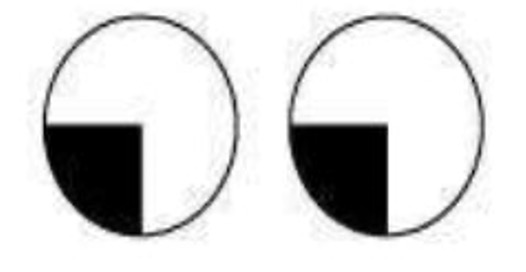
Confrontation visual field testing is an important clinical examination, especially when it comes to neuro-ophthalmology cases. A simple test can give us clues as to what may be the underlying cause of patients’ symptoms. The test is done presuming the visual field of the examiner is normal. Both the patient and the examiner should be seated at an equal height at a distance of 1 meter. The right eye field is tested by asking the patient to close their left eye and the examiner closes his/her right eye. The first question the examiner must ask the patient, if they are able to see the examiner’s face clearly, without any parts missing. The examiner then moves a pin-point target from out to in all 4 quadrants, while instructing the patient to continuously look into the examiner’s eye. When the patient sees the object, they inform the examiner, who is then able to compare when they themselves saw the object. Normally, superior and nasal fields extend 600, inferior fields extend 700, and temporal fields extend 1000
2. Who needs visual field testing?
Certain clues on history and examination tell us if a patient needs a neurological field test. Following are certain scenarios:
- Sudden painless decrease in vision- unilateral or bilateral
- Patient complaining of field defect
- Headache with nausea and vomiting along with visual symptoms
- Notice field defect while taking vision – patient misses optotypes on either temporal or nasal side when testing the vision of either eye
- Signs of optic nerve dysfunction – RAPD, impaired color vision, optic disc edema (unilateral or bilateral), temporal pallor of the optic disc, optic atrophy
3. There is more to visual field testing than only 24-2!
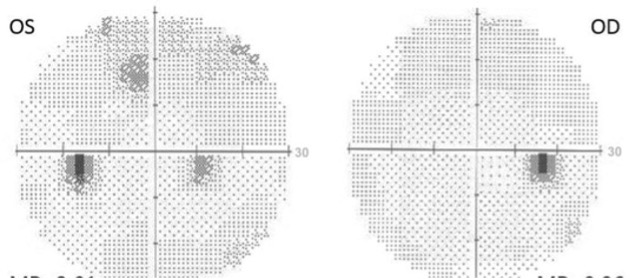
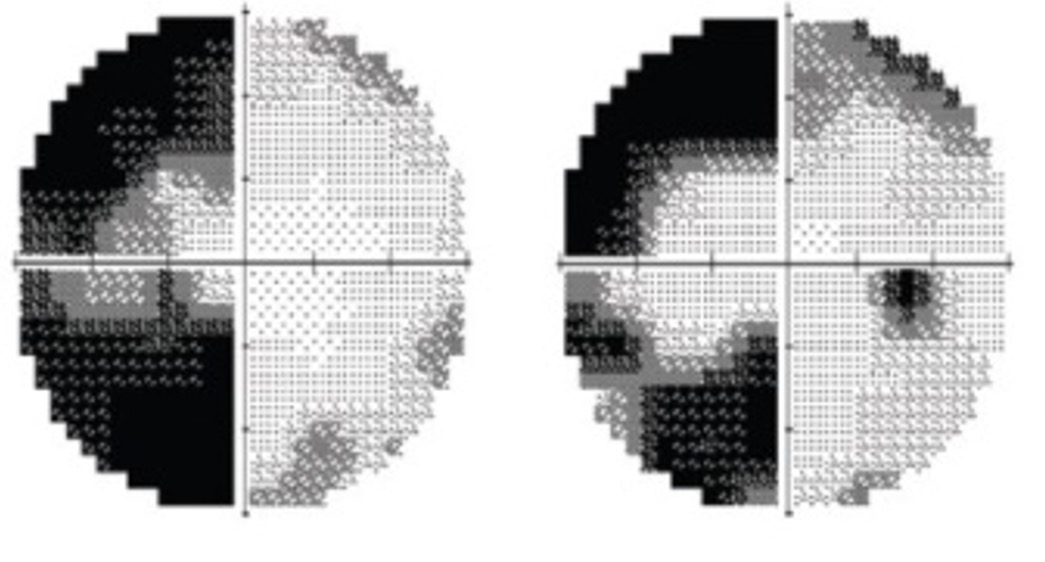
Once visual field testing is indicated, it is important to know which field to order. Humphrey automated perimetry 30-2 SITA standard is preferred over the 24-2 SITA fast usually ordered in glaucoma patients, as it provides even testing points both nasally and temporally. This helps us to identify temporal field loss better, and further tells us if the defects are symmetrical or not (congruous or incongruous). Most of the 30-2 tests are also ordered with a 10-2, especially when there is bilateral optic disc edema or partial optic atrophy. 10-2 field tests the central 10 degrees (68 points), and picks up central/paracentral scotomas. Options of 60-2 and 120-2 are also available for full neurological field testing, however are done rarely.
4. Patient can’t see? We’ll give them a target that they can.
It is important to note that some patients who may be suffering from a neuro-ophthalmological disorder may have poor vision. In this instance, the ophthalmologist can request for the perimetry to be done with larger size targets. This can increase the reliability of the test, and allow us to reach a diagnosis.
5. Now comes the interpretation of the test. Let’s read the printout!
It cannot be reiterated enough how important it is to correctly read a visual field test printout. Though when it comes to a neurological field report, reliability indices may remain low. However, we need to ensure the patient's name and age are correct and the patient has a full refractive correction in place during the test. Also, we must correctly identify the eye being reported.
6. How do the patients see, or not see? Various patterns.
Neurological field defects usually respect the vertical meridian. There are exceptions.
- Altitudinal field defect (unilateral usually) – seen in non-arteritic anterior ischemic optic neuropathy
- Blindspot enlargement – normal blind spot is 150 temporal to fixation, 1.50 below the horizontal meridian, and it measures 7.50 vertically and 50 horizontally. Enlargement is seen in papilledema (bilateral optic disc edema secondary to raised intracranial tension)
- Central scotomas – Help to identify toxic optic neuropathy, nutritional optic atrophy, and hereditary optic neuropathies.
- Non-specific pattern – optic neuritis, compressive optic neuropathy
7. Why? To localize lesions in the visual pathway.
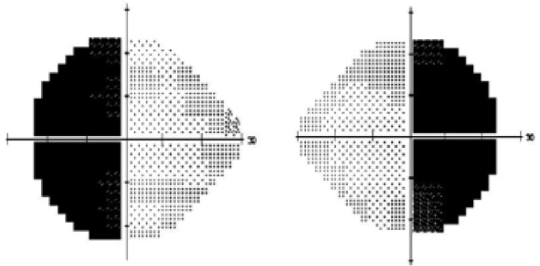
- Prechiasmatic – there is no crossing over of optic nerve fibres, and defects will be uniocular.
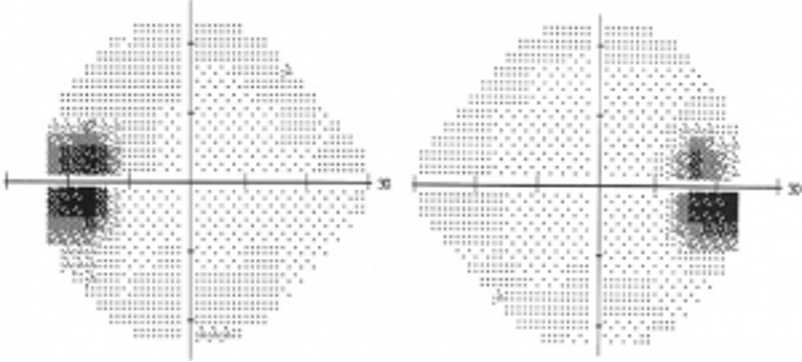
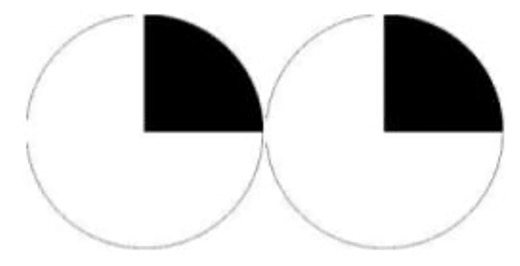
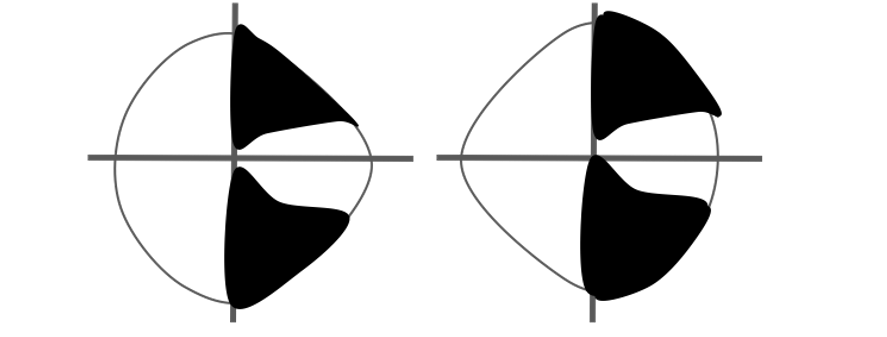
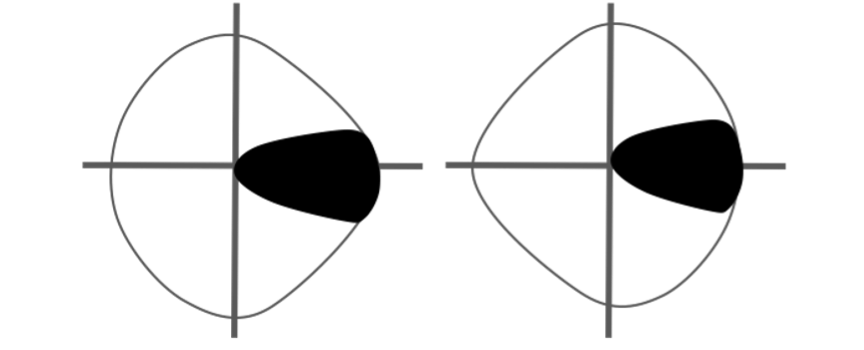
- Chiasmatic – usually defects are bitemporal, secondary to compression of chiasma. Lateral compression of the chiasma can lead to binasal hemianopia. Anterior lesions at the junction of optic nerve and chiasma may lead to an ipsilateral central scotoma and contralateral superior temporal quadrantanopia.
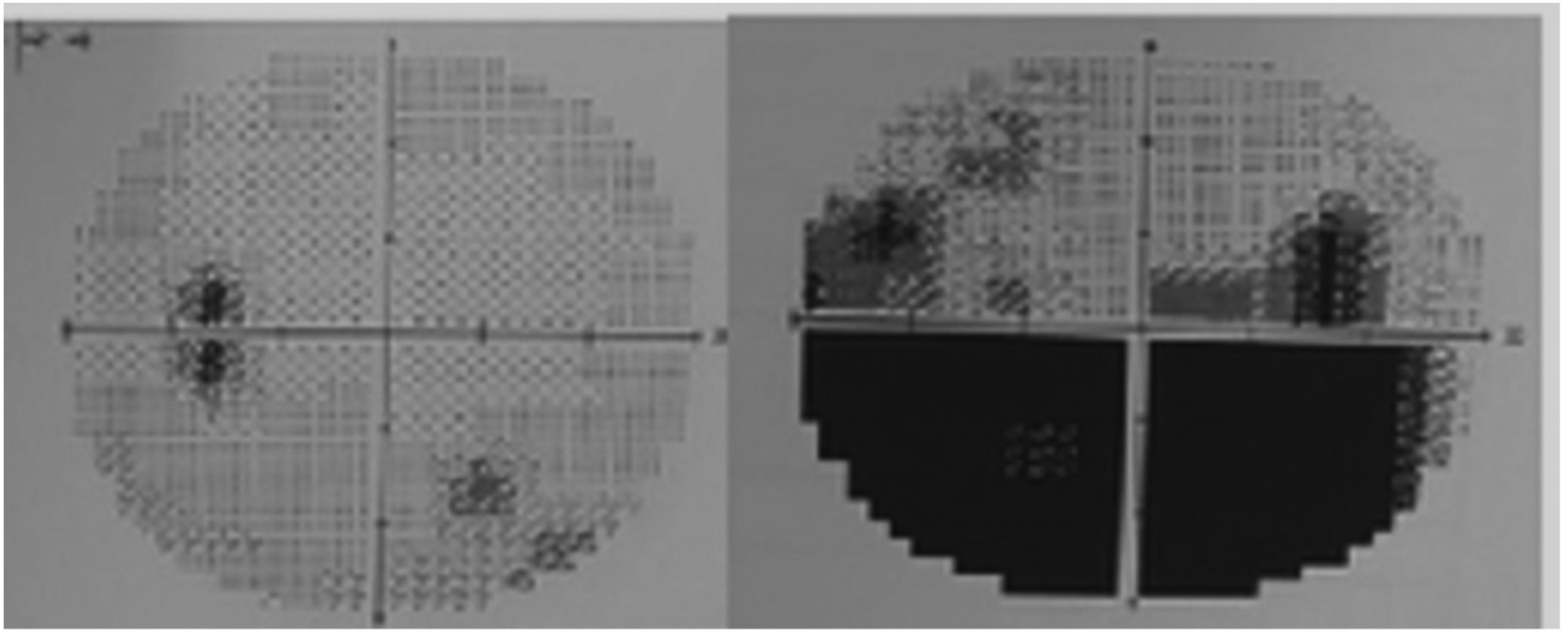
- Postchiasmatic – these are same-sided field defects, termed homonymous hemianopias. Those that are incomplete and asymmetrical are termed incongruous. The more posterior the lesion, the more congruous the defect becomes.
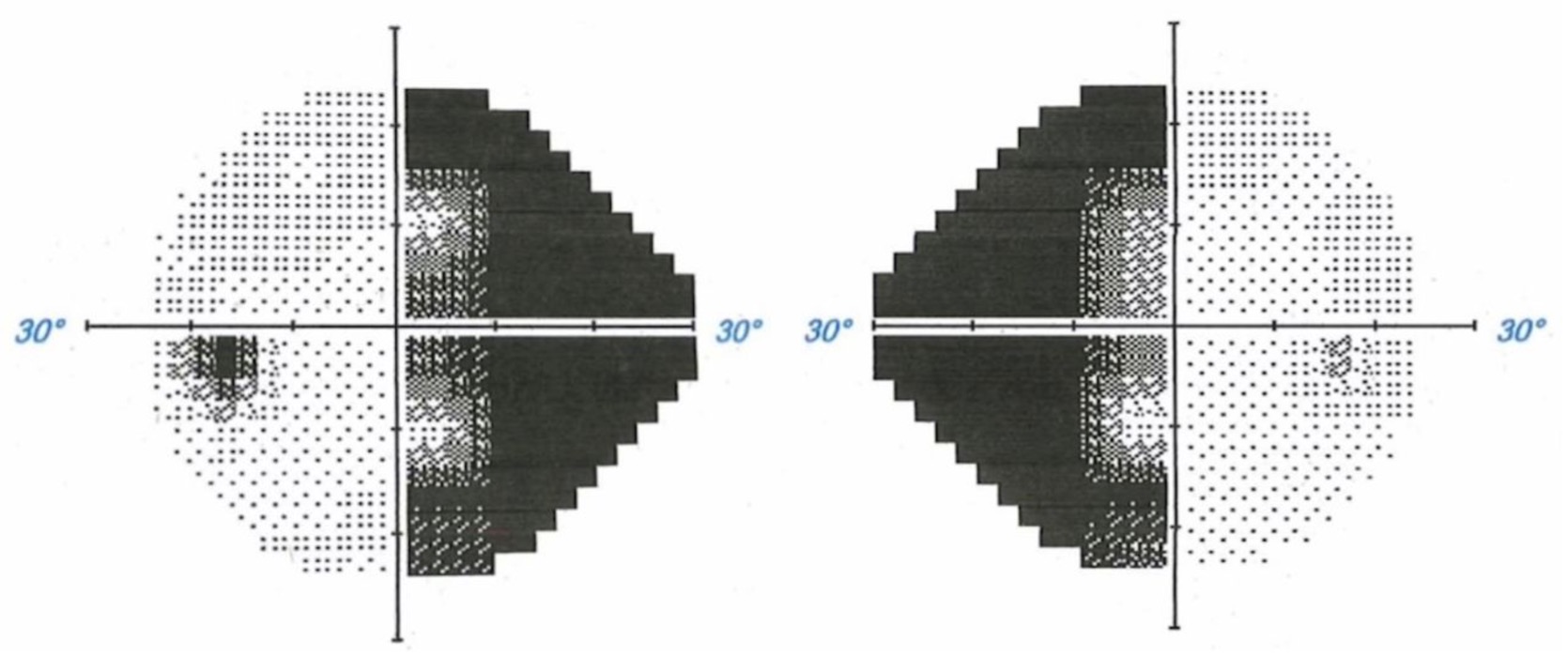
- Quadrantanopia – when the optic radiations going through the temporal (Meyer’s Loop – pie in the sky) and parietal lobe (Baum’s Loop- pie in the floor) are affected
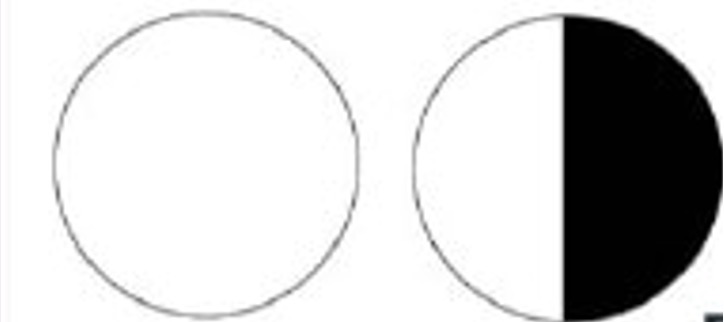
- Macular sparing – the stroke of posterior cerebral artery circulation. Occurs due to anastomotic vascular supply from contralateral circulation.

8. Rare types of neurological field loss
- Junctional scotoma of Traquair – ipsilateral optic nerve at the junction with chiasma without affecting the decussating nasal fibers of the contralateral eye.
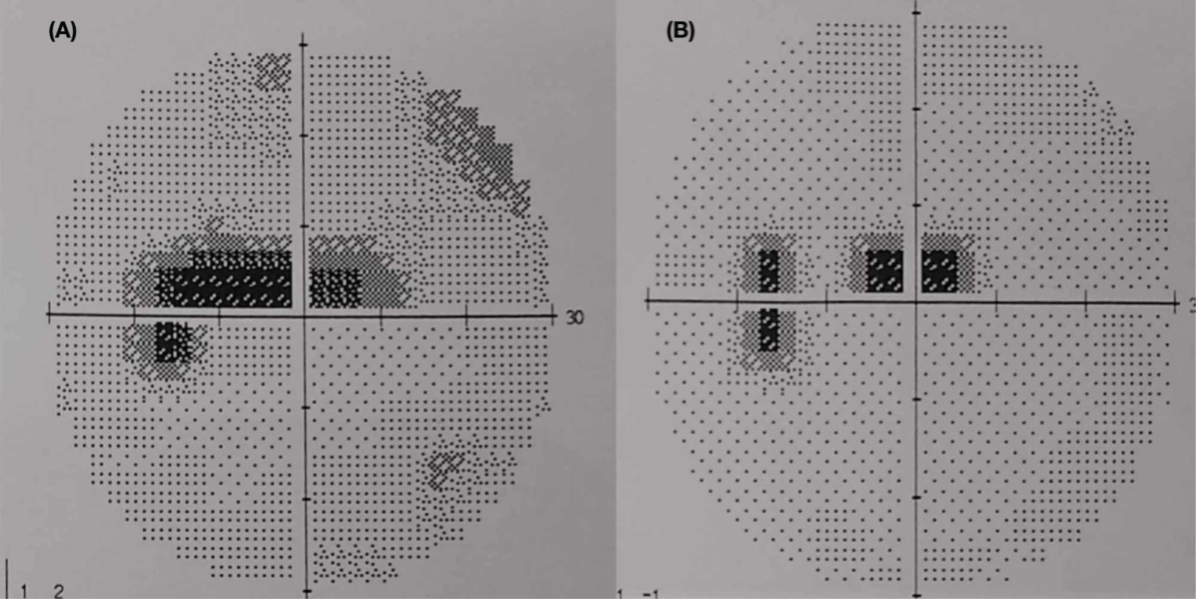
- Sectoranopia – involvement of the lateral geniculate body. It has a dual blood supply by the anterior and posterior choroidal arteries. Involvement of the anterior choroidal artery results in a superior and inferior wedge defect, while in the involvement of the posterior choroidal circulation will lead to a defect between these two areas.
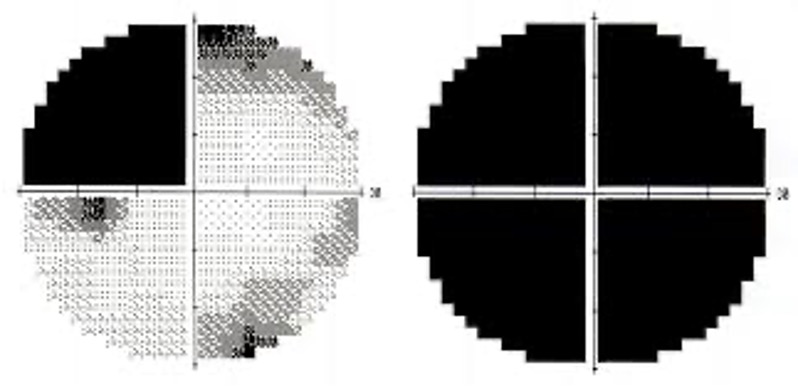
- Homonymous scotomatous defects – central 30-degree defect with sparing of peripheral field. It occurs to due to the tip of occiput injury which is not compensated by the dual circulation.
- Monocular temporal crescent (half-moon syndrome)– occurs as a field defect of 30 degrees of the farthest peripheral temporal field which is not overlapped by the contralateral eye’s nasal field. Occurs in the contralateral eye when there is the involvement of the anterior-most part of the calcarine cortex
- Temporal crescent-sparing defect – when the anterior-most point of the calcarine cortex is spared, then there is homonymous hemianopia sparing the unpaired temporal crescent.
9. When to order and follow up?
Suspicion of the neurological cause of visual symptoms warrants a visual field test at the initial visit. These tests are important for diagnosis and also for monitoring the disease condition. For example, in the setting of homonymous hemianopia, the diagnosis of an intracranial space-occupying lesion is made for which surgery may be performed. Following this, serial visual field tests can help ascertain any recurrence of the tumor. This test can also be used as a prognostic indicator in certain situations. Progressive worsening of visual fields in idiopathic intracranial hypertension implies poor visual outcomes.
10. How it helps in further evaluation and management?
Depending on what pattern of field loss is present, subsequent investigations are ordered. In case of altitudinal field defects, a thorough systemic evaluation is needed to evaluate for prothrombotic risk factors, and an MRI is avoided. In non-specific field defects associated with optic disc edema, an MRI brain and orbit with contrast may be needed to look for optic neuritis. If there is central scotoma, then evaluation of toxic and nutritional neuropathy is needed. In hemianopias, again an MRI of the brain is needed to rule out a space-occupying lesion or a vascular cause.
.jpeg)