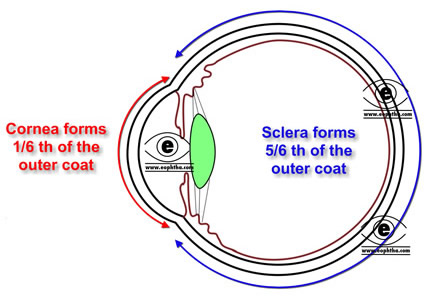
The cornea is the transparent tissue that covers the front of the eye.It forms anterior 1/6th of the outer fibrous coat of eyeball.
The word cornea has come from “Kerato”. The term “Kerato” in greek means horn or shield like. Ancient Greek used to believe that cornea is derived from same material like that of thinly sliced horn of animal.
Embryology:
| Structure | Derived from |
|---|---|
| Corneal epithelium | Surface ectoderm |
| Stroma, Descmet’s membrane, endothelium | Paraxial mesoderm |
Topography:
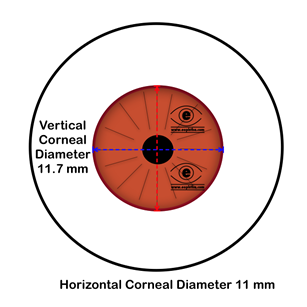
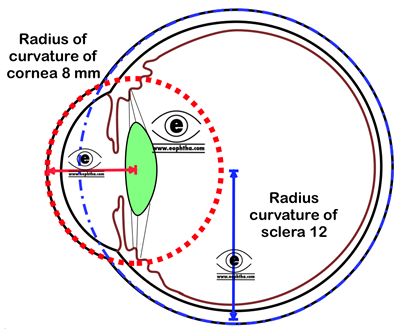
Anterior surface of the cornea is elliptical whereas posterior surface is spherical with average diameter 11.5 mm. Horizontal diameter of the anterior surface (HCD) is 11.7 mm and vertical diameter (VCD) is 11mm.Of them HCD is of clinically important.The radius of curvature of cornea is 8 (7.8 mm).It is the result of differences in radius of curvature in the vertical horizontal meridians which causes astigmatism.
Microcornea = when HCD is less than 10mm
Macrocornea = when HCD is more than 13 mm
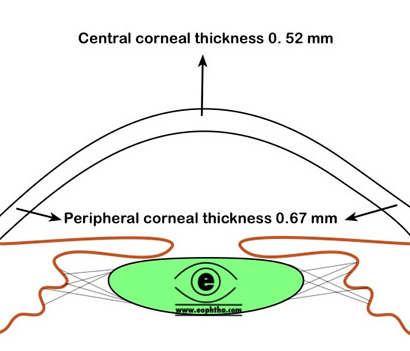
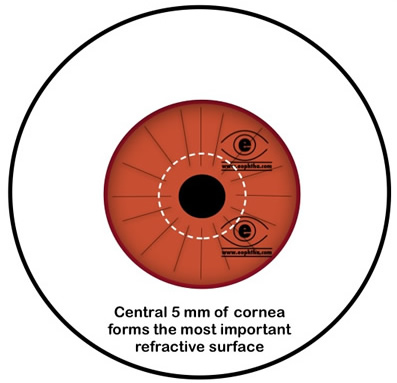
The central corneal thickness is 0.52 mm, whereas periphery is 0.67 mm thick. Central corneal thickness has direct influence in IOP measurement. The central 5 mm of the cornea forms the most powerful refracting surface of the eye. The refractive power of the cornea is 45D which is 3/4th of the total refractive power of eye. The refractive index of cornea is 1.376.
|
Refractive indices of different media through which light enters the eye |
|
|---|---|
|
Air |
1.00 |
|
Tear fluid |
1.33 |
|
Cornea |
1.37 |
|
Aqueous humor |
1.33 |
|
Lens |
1.42 |
|
Vitreous |
1.33 |
Microscopic Anatomy of cornea:Cornea is composed of five layers. The layers are as follows:
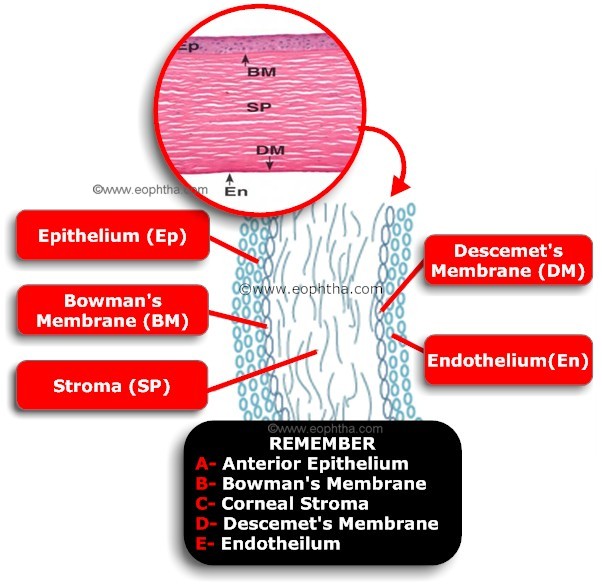
| Layers | Thickness (in µm) | Composition |
|---|---|---|
| Epithelium (Ep) | 50 | Stratified Squamous Epithelium |
| Bowman's Membrane (BM) | 8-14 | Compact layer of unorganised collagen fibres |
| Stroma (SP) | 500 | Orderly arrangement of collagen lamellae with keratocytes |
| Descemet's Membrane (DM) | 10-12 | Consists of basement membrane materials |
| Endothelium (En) | 5 | single layer of simple squamous epithelium |
Corneal Epithelium:
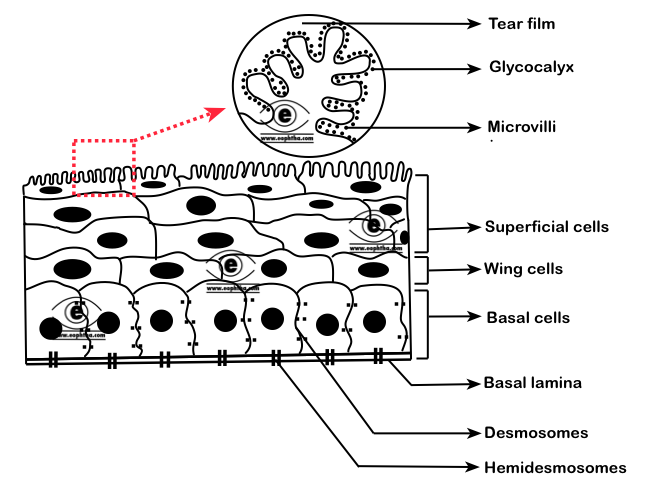
Epithelium represents 10 percent of the corneal thickness. Corneal epithelium is a stratified squamous nonkeratinised epithelium.
| Stratified | Multilayered,has 5-6 layers |
|---|---|
| Squamous | Superficial or apical cells are flattened |
| Nonkeratinised | cells are nucleated and do not contain keratin (Keratinised epithelium are found in dry areas of body like skin and nonkeratinised epithelium are found in moist areas) |
The cells in the epithelium are held together with the help of desmosomes and with the basal lamna with the help of hemidesmosomes and other filaments .
Recap: Desmosomes link two cells together; Hemidesmosomes attach one cell to the extracellular matrix
The surface corneal epithelial cells has numerous microvilli and microplicae and these cells secrete glycocalyx which helps in adhesion and stability of the tear film. Epithelium can be divided into superficial squamous cell layer, the middle wing cell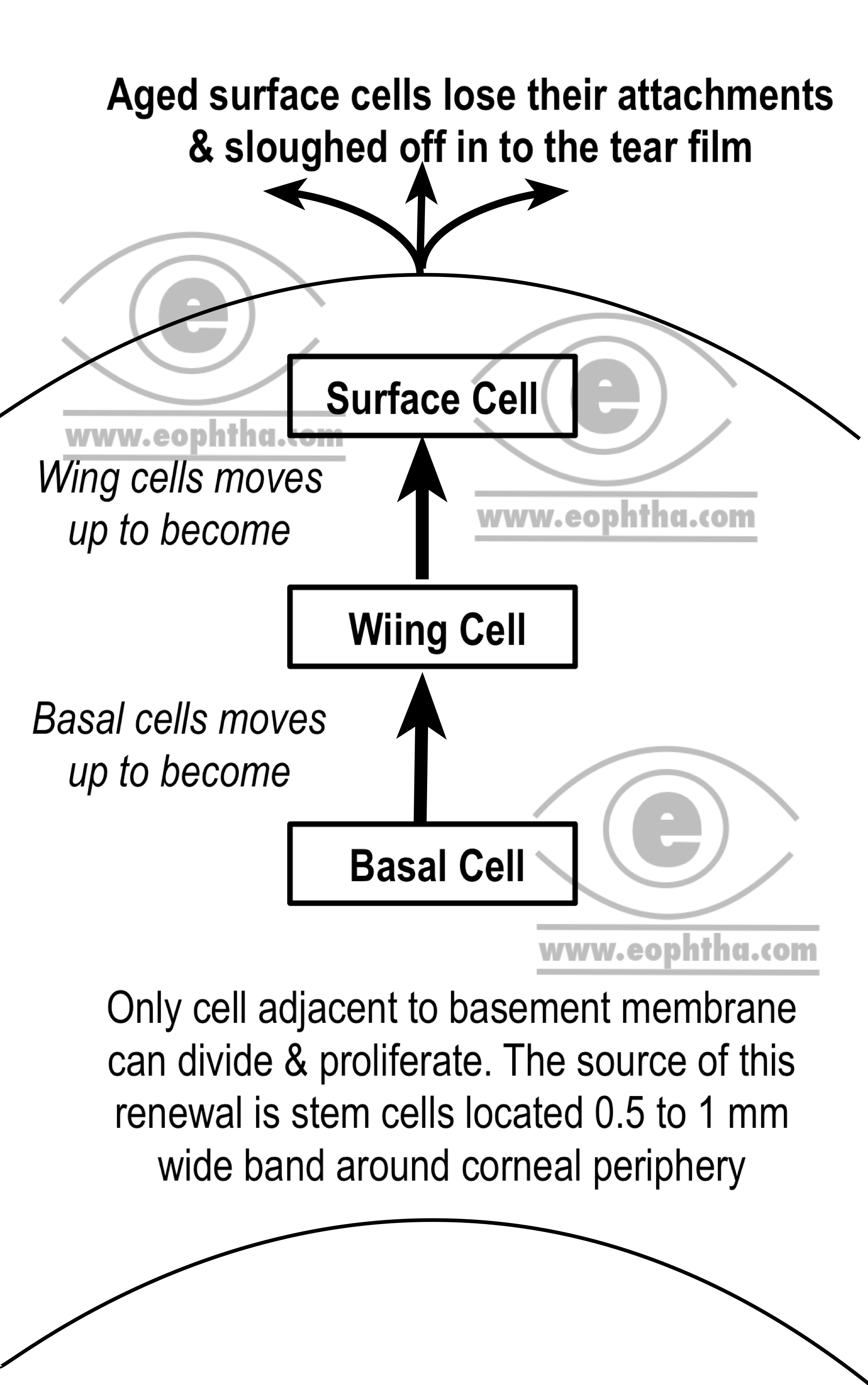
Epithelial stem cells are the undifferentiated pluripotent cells which serve as an important source of new corneal epithelium. They are found in limbal basal epithelium of palisades of Vogt.Click hereto read more about limbal stem cells.
The basal cells are attached to the basement membrane or basal lamina with the help of hemidesmosomes. The basal lamina is an extracellular secretory product of the basal epithelial cells. The main function of this basal lamina is to attach corneal epithelium with the stroma. One destroyed it takes about 6 weeks for basal lamina to regenerate.
|
Layers of epithelium |
Description |
Mitotic activity |
|---|---|---|
|
Basal Cell |
Single layer of columnar cells found adjacent to basal layer |
- |
|
Wing cell |
2-3 layers of cells with elongated process |
- |
|
Surface cells |
3 layers of flattened epithelial cells with microvilli in contact with the tear film. |
+ |
It takes normally 7 days for replacement entire corneal epithelium
Bowman's Membrane:
Bowman's Membrane is named after English anatomist and ophthalmologist William Bowman. It is an acellular tough membrane like zone situated in between corneal epithelium and stroma. It is 8-14 µm thick and composed of randomly arranged collagen fibers. Though the collagen fibers are finer than those found in corneal stroma and randomly arranged, these collagen fibers are continuous with that of anterior stroma. That’s why many authors consider it as a modified region of anterior stroma. Because of the compact arrangement of collagen fibers, it is comparatively resistant to trauma. However, once destroyed it cannot be regenerated.
|
Remember!! Bowman’s membrane is not a basement membrane like Descemet’s membrane |
Corneal Stroma/Substantia propria:
The stroma or substantia propria, which occupies about 90% of the total corneal thickness, is composed of collagen fibrils, keratocytes and extracellular ground substances. Collagen components constitute more than 70% of the dry weight of cornea. Collagen fibrils with uniform 25- to 35-nm diameter are arranged in flat bundles called lamellae. The lamellae extend from limbus to limbus and are oriented at various angles to one another. Collagen fibers form approximately 300 lamellae in corneal stroma. Two important of corneal collagen fibers, which accounts for the transparency of cornea, are-
- Collagen fibers are highly uniform in diameter (25-35 nm)
- The distance between two corneal fibers is also highly uniform (41.5nm)
Corneal transparency is mainly dependent on the arrangement of these collagen fibers in stroma. Mean diameter of individual collagen fiber and mean distance between collagen fibers are almost same and both of them are less than half of the wavelength of visible light (400-700nm).As a result scattering of an incident ray of light by a collagen fiber is cancelled by interference from other scattered rays of light (destructive interference).
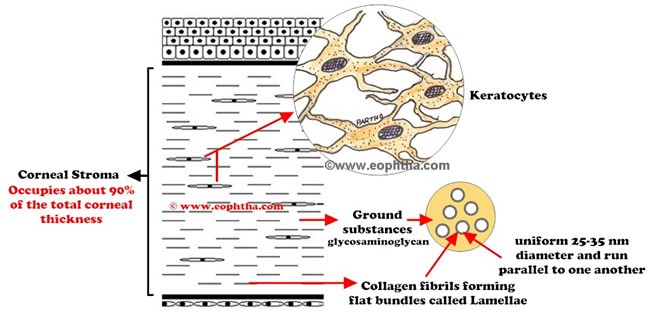
Corneal clouding in corneal odema occurs due to accumulation fluid which increases the distance between the collagen fibers.
Extracellular matrix or ground substances found in cornea are mainly glycosaminoglycan. The primary glycosaminoglycans of the stroma are keratin sulfate (forms 65% of the total glycosaminoglycan content) and chondroitin sulfate. Amongst the cellular components, Keratocytes (corneal fibroblasts) are the major cell type of the stroma. They occupy 3-5% of the stromal volume. They are spindle shaped and in cross section, found scattered in between the lamellae of collagen fibers. They synthesize collagen and extracellular matrix components and thus maintain the stroma.
Descemet’s membrane:
Descemet’s membrane is the thick basement membrane secreted by the endothelium. It is produced constantly and so it thickens throughout life (3 µm at birth and increases to 10 µm in adult). Descemet's membrane does not adhere strongly to the stroma, and so, it can be surgically dissected as a sheet. Though no elastic fibers are present, the Descemet’s membrane exhibit elastic property due to the particular arrangement of collagen fibers. The membrane terminates near limbus as Schwalbe’s line.
In case of Descemet’s Membrane detachment or tear, the membrane curls towards the stroma (inwards) because of the elastic property of Descemet’s membrane. The lens capsule, which is also a basement membrane has similar tendency, but curls outwards-towards anterior chamber.
Unlike the attachment of Bowman’s membrane and corneal stroma, Descemet’s membrane is comparatively weakly attached to corneal stroma and this surface is sharply defined. Descemet’s membrane is a tough layer which is resistant to enzymatic degradation by phagocytes and toxins.
In corneal ulcer, Descemet’s membrane remains intact and often herniates out as a result of increased intraocular pressure, which known as Descematocele.
Corneal endothelium:
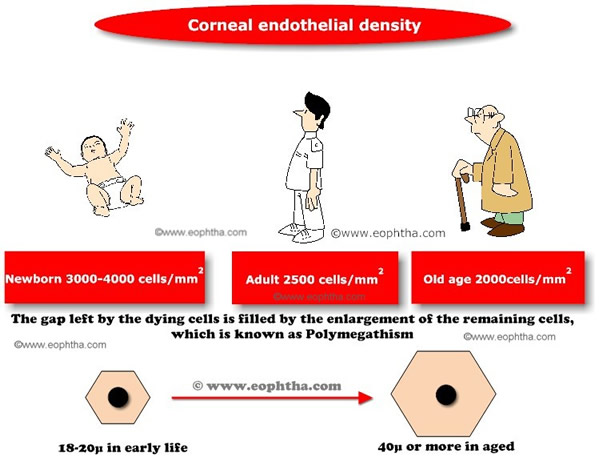
The name endothelium is misnomer. Basically, corneal endothelium is a simple squamous epithelium. The shape of the individual cells is hexagonal which forms continuous mosaic pattern, best seen in specular microscopy. The endothelial cells are interconnected with each other with various junctional complexes like zonula occludans, macula occludans and macula adherens. These cells possess ion transport system which is known as endothelial pump. These endothelial pumps regulate the water content of corneal stroma.
Endothelial cells cannot divide or replicate. With ageing, the cell density of the endothelium decreases which is compensated by an increase in cell size (Polymegathism) or shape (Pleomorphism).As these endothelial cells are involved in corneal hydration (which helps in maintenance of corneal transparency), endothelial cell density below 800 cells/mm2 leads to corneal decompensation.
Corneal response to injury:
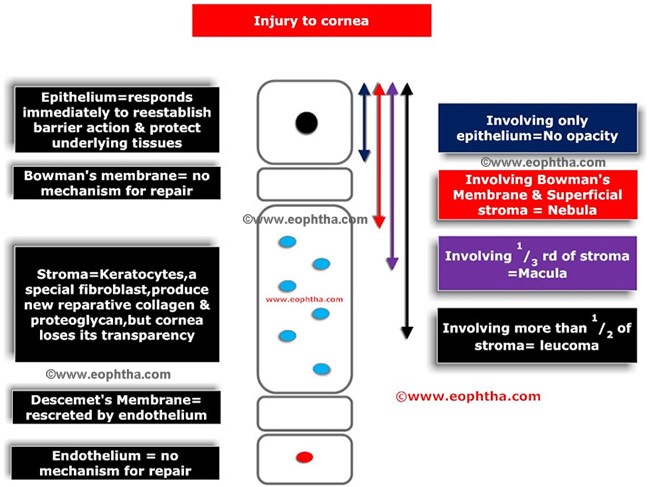
When an injury occurs in corneal epithelium, basal cells are moved to the damaged area and subsequent cellular proliferation from basal layers fills the defect. Bowman's membrane does not regenerate. The wound in Bowman's membrane is replaced by stroma like fibrous tissue or epithelium. In response to trauma to corneal stroma, there is increase in number of keratinocytes and the ground substances and collagen fibrils secreted by the keratinocytes. However the stromal tissue thus produced is different-diameter of the newly formed stromal collagen is larger (comparable to those found in sclera) than the normal stromal collagen. Also the newly formed collagen fibrils are not well organised and lack the normal tensile strength of the collagen fibrils. The response of various layers of cornea to trauma or injury is summarized below.
Blood supply to cornea:
In normal condition, cornea does not contain any blood vessels. Anterior ciliary artery, a branch ophthalmic artery forms a vascular arcade in the limbal region and helps in corneal metabolism and wound repair by providing nourishment. Absence of blood vessel in cornea is one of the contributing factors for its transparency.

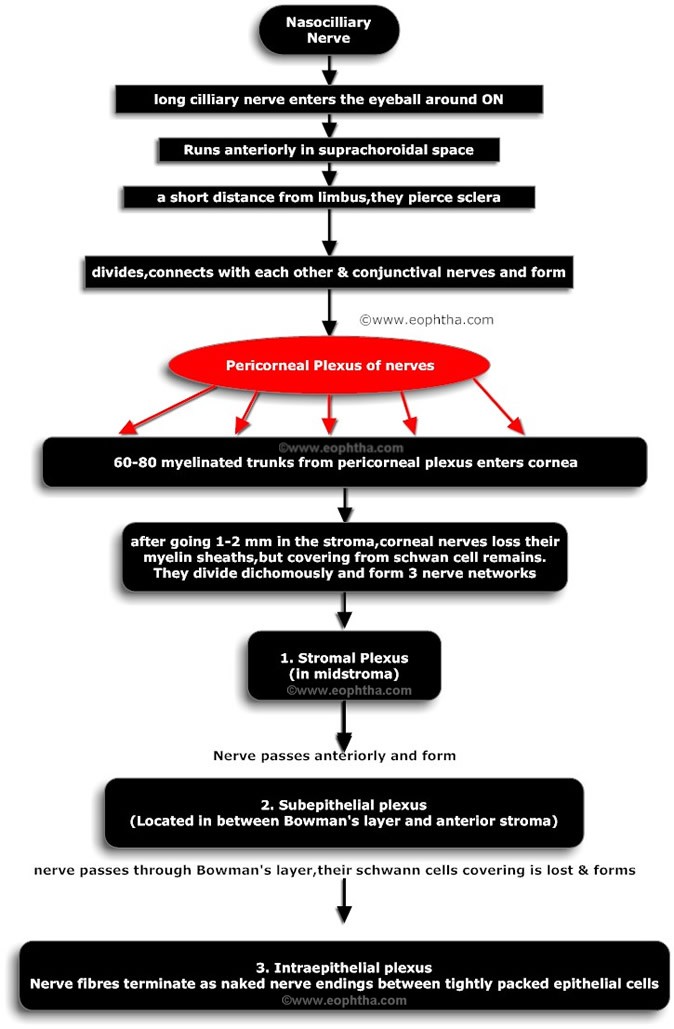
Nerve supply of Cornea:
Cornea is one of the highly sensitive tissue of human body. Density of the nerve ending in cornea is about 300 times of that of skin. An area of 0.01 mm2 cornea may contain as many as 100 nerve endings. Cornea is primarily innervated through the ophthalmic branch of the trigeminal nerve. The ophthalmic division of the trigeminal nerve has three parts: the frontal nerve, the lacrimal nerve, and the nasociliary nerve. The nasociliary nerve provides sensory innervation to the cornea. The pathways of innervation are described in figure below.
Pathological conditions which lead to loss of corneal epithelium, cause severe pain due to exposure of corneal nerve ending.
While doing slit lamp examination, you may have seen corneal nerves as thin fibers in corneal periphery. In normal condition, corneal nerves are mainly visible in periphery as the diameters of the corneal nerves are larger in periphery as compared to center.
Infection or reactivation of latent herpes simplex virus located in trigeminal ganglion affecting eye reduces corneal sensation due to damage to the nerve endings.
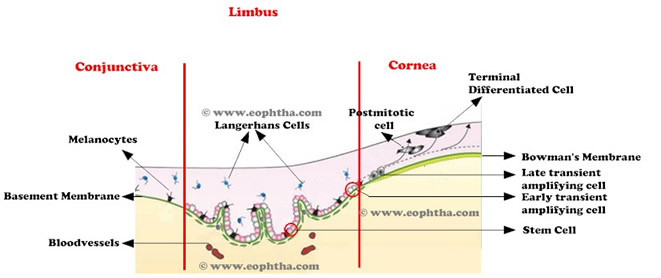
Limbus:
Pallsade of Vogt is radially oriented fibrovascular ridges that are mainly concentrated along upper and lower limbus. They lie just peripheral to the terminal capillary loops of limbus.Limbus is an annular transition zone which separates the anatomically contiguous, yet phenotypically different cells of the conjunctival and corneal epithelium.Limbus has a distinct histological architecture. It differs from conjunctiva in that it is devoid of goblet cells, and unlike the corneal epithelium, it has Langerhan's cells, melanocytes, and underlying blood vessels.
| Limbal Zone | Boundary |
| Corneal Side | By a line drawn between the termination of Bowman's layer and Descemet's membrane |
| Conjunctival or Scleral Side |
By a parallel line approximately 1 mm peripherally. This line runs just outside Schlemm's canal |
At limbus,
- Corneal epithelium becomes bulbar conjunctival epithelium
- Bowman's membrane becomes continuous with the lamina propria of the conjunctiva and tenon's capsule.
- Stroma becomes sclera
- Descemets membrane becomes schwalbe's line.
- Endothelium lines the trabecular meshwork and becomes continuous with the anterior surface of the epithelium
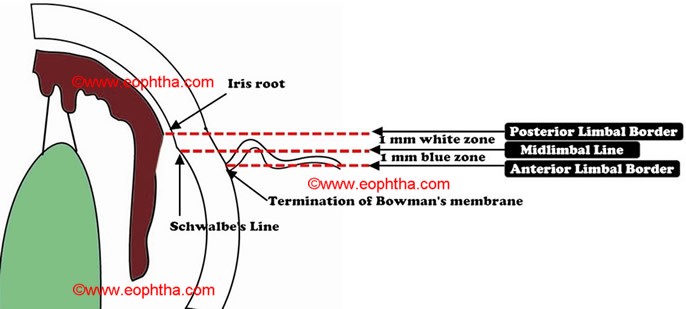
Surgical limbus:
Surgical limbus is a 2mm wide zone. For ease of description this zone can be divided into:
- Anterior limbal border is represented by insertion of conjunctiva into peripheral cornea, which overlies the termination of Bowman’s membrane.
Under microscope, anterior limbal border can be identified as a zone in clear cornea where fine conjunctival vessels are terminating.
- Blue zone: Posterior to anterior limbal border, there is a blue zone which terminates in midlimbal line. This zone extends for 1 mm superiorly and 0.8 mm inferiorly.
Under microscope, blue limbal zone can be identified as bluish translucent area, after dissecting overlying conjunctiva and tenon’s capsule from anterior limbal border
- Midlimbal line overlies the Schwalbe’s line which is termination of Descemet’s membrane. It is the junction of blue and white zone of limbus.
- White zone: It starts at midlimbal line and extends for 1 mm and terminates in posterior limbal border. This zone overlies the trabecular meshwork.
- Posterior limbal border: Posterior limbal border is situated 1mm posterior to the midlimbal line. It overlies the scleral spur and iris root.
The colour differences of the limbal region occurs because of interdigitation of the corneal fibers into scleral fibres
Surgical incision:
- An incision in blue limbal zone can cause Descemet’s membrane stripling.
- Midlimbal line is the preffered site of incision
- If incision is posterior to the posterior limbal border, it can cause excessive bleeding & hyphama due to injury to the cilliary body.
- An incision in white limbal zone can cause injury to the trabecular meshwork.
- Clear corneal incision is made in front of the anterior limbal border that is at the most anterior aspect of the blue zone.
Limbal Stem Cells:
Limbal epithelial stem cells are the undifferentiated pluripotent cells which serve as an important source of new corneal epithelium. They are found in limbal basal epithelium of palisades of Vogt.
Only 5% to 15% of the cells in the limbus are stem cells
The basal cells of limbal epithelium comprises the limbal stem cells.The salient features of these stem cells are-
- They are the precursor for all other cells of the tissue
- They have a self maintaining population
- They accounts for only a small portion of total cells of the tissue
- In vivo,they show slow cycling,but when placed in cell culture,they demonstrate high potential to proliferate.
- They can not be differentiated with rest of the cells of tissue.
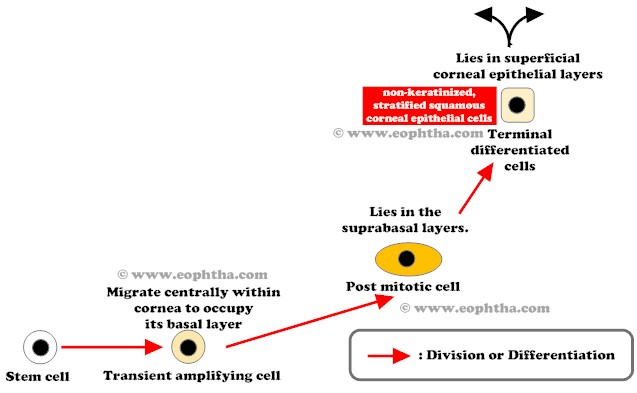
Life cycle of stem cells:
Stem cells in the limbus divide to produce a daughter stem cell and a transient amplifying cell. These transient amplifying cells migrate within the cornea to lie in basal layer of corneal epithelium. Further cellular divisions of transient amplifying cells produce postmitotic cells, which lie in the suprabasal layers. Progressive differentiation of postmitotic cells produce terminally differentiated cells, which lie in the superficial corneal epithelial layers. These terminally differentiated cells are non-keratinized, stratified squamous corneal epithelial cells. These cells are continually sloughed away from the corneal surface and replaced by maturing, underlying cell layers.

.PNG)