1. External face features affecting the eye position
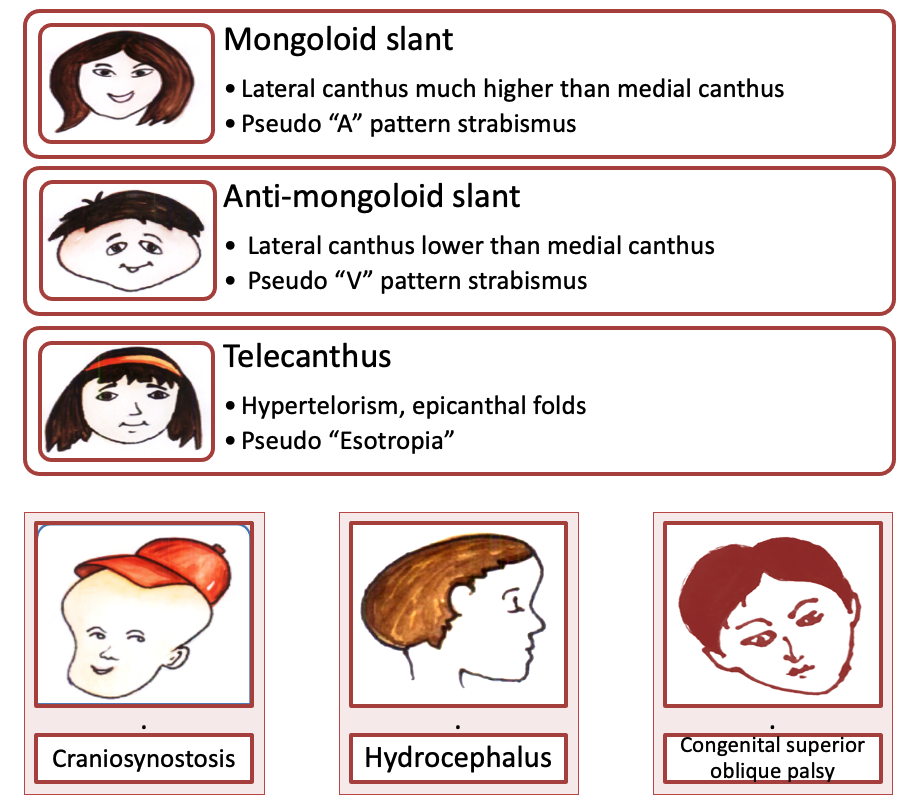
- Facial asymmetry and palpebral fissure shape changes alter the ocular position, possibly due to extra-ocular muscle heterotopy
- The common extra-ocular features affecting ocular position are craniosynostosis, hydrocephalus, facial fracture, mongoloid and anti-mongoloid slant, telecanthus, congenital superior oblique palsy (face fuller on the affected side), facial nerve palsy.
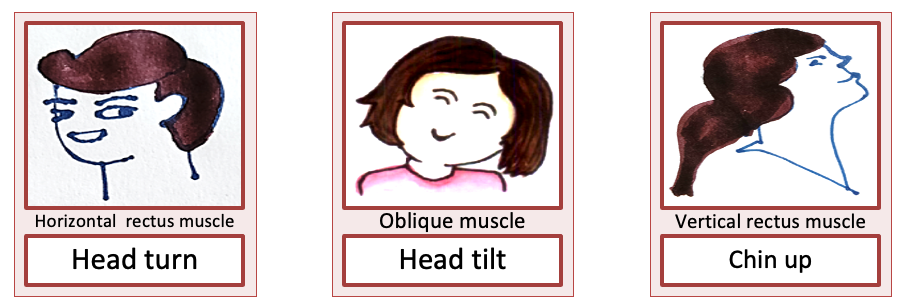
2. Head posture
- Head does what eye cannot do
- Look for abnormal head posture when a patient is reading best-corrected visual acuity with proper refractive correction. The target should preferably be at the eye level of the patient in order to avoid a false chin-up position
- Head tilt, turn, chin-up/down
- Head turn is the opposite side of the ear seen
- Measure with a goniometer
- Look for incomitant strabismus and nystagmus
- Keep patient’s head straight throughout the examination – eg. In patients with Duane syndrome, small change in head posture can cause large ocular deviation changes
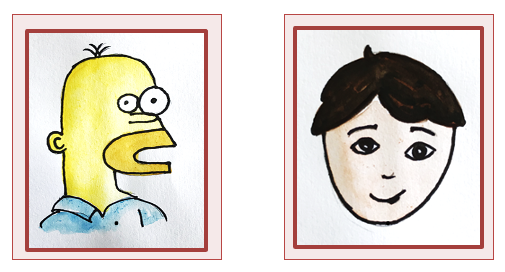
3. Ocular position
- Relation of the globe to orbit
- Look by worms/ birds’ eye view
- Proptosis, enophthalmos, hyper/hypoglobus
- Measure with an exophthalmometer
4. Sensory evaluation before motor assessment of strabismus
- To avoid disruption of fusion by multiple tests during motor examination, especially in cases of intermittent exotropia
- Visual acuity with and without glasses, binocular visual acuity, visual acuity in abnormal head posture, visual acuity with corrected head posture, near vision, diplopia assessment, double Maddox rod test, stereo-acuity
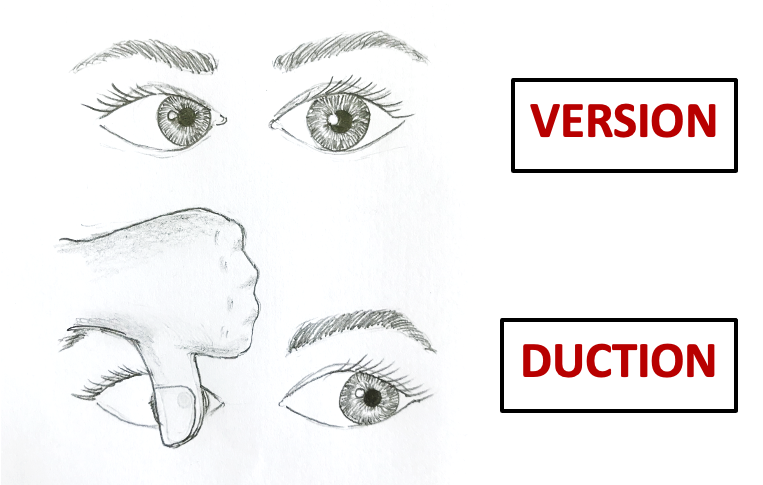
5. Extraocular motility
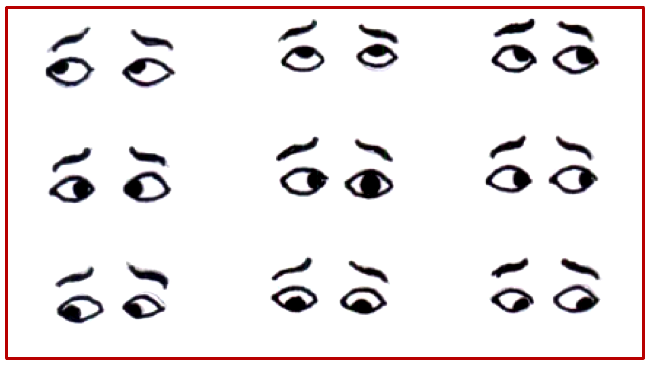
- Versions are examined with both eyes open and it tells us how well the eyes move in synchrony to each other in nine cardinal positions of gaze.
- Ductions are monocular movements and are examined with one eye occluded to evaluate the ability of the eye to move into extreme fields of gaze in the direction of action of muscle
- Never forget to check for ductions if versions are limited
6. Assessing obliques’ over/under the action
- A simple way to assess the over actions of inferior oblique is to compare the level of inferior limbus while the eyes are in dextroversion, dextro-elevation or levoversion, levo-elevation as the case may be.
- If the level of the inferior limbus is higher in the adducting eye it is suggestive of an inferior oblique overaction (IOOA) in that eye. Similarly the superior limbus levels are compared while assessing the superior oblique muscles.
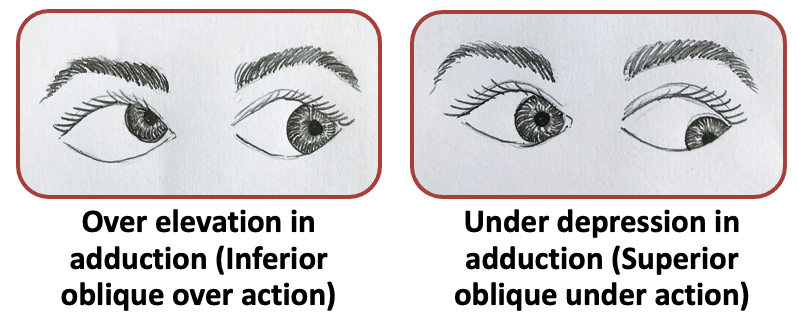
- When checking for oblique action, make sure the abducting eye is fixing, allowing the adducting eye to manifest over action/under action

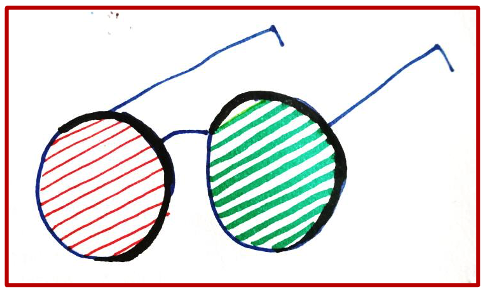
7. Spectacle correction
- Measure squint with proper spectacle correction
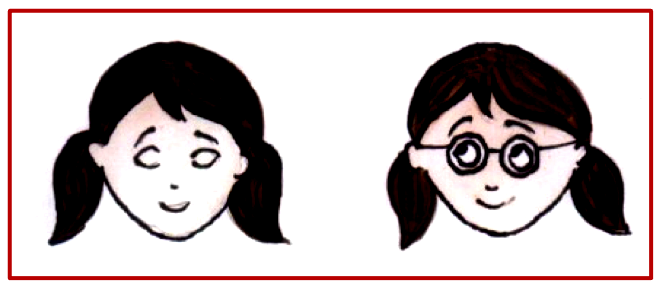
- High plus or minus spectacles (≥5 D) create a built-in prismatic effect in strabismic patients that must be taken into account when performing a cover test
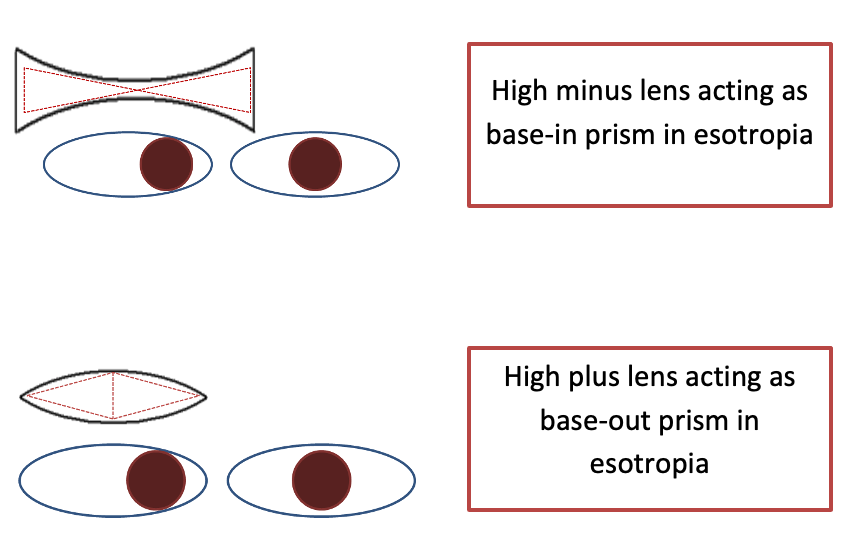
- “Minus” measures “more” in both exotropia and esotropia
- “Plus” measures “less” in both exotropia and esotropia
8. Measuring deviation
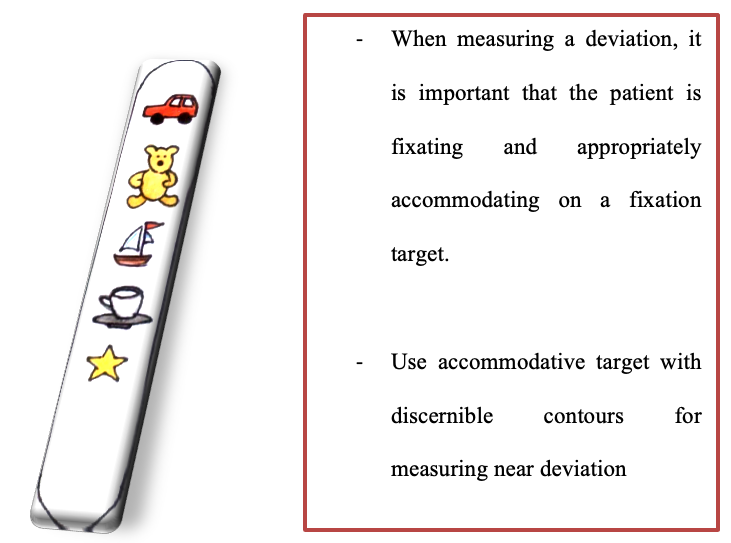
- Measure deviation in all nine gazes tilts (specifically for vertical tropias), and near
Prism position
- Incorrect positioning of prisms while performing cover tests can give variable measurements leading to erroneous surgical outcomes.
- Glass prisms in prentice position and, plastic prisms in frontal position
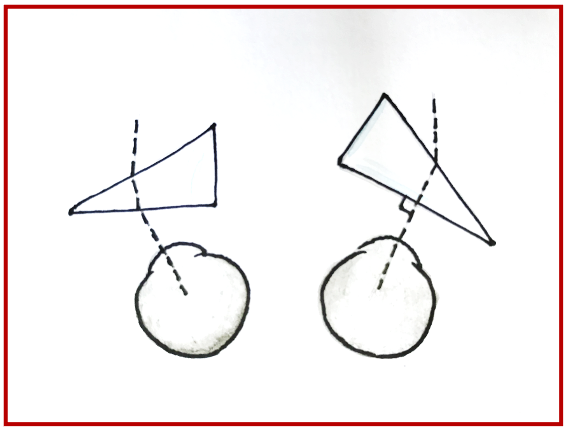
- Measuring in head tilt: Prism held with the base parallel to the lateral wall or floor of the orbit when measuring in head tilt.
9. Palpebral fissure changes and abnormal eye movements
Palpebral fissure changes
Narrowing, widening, retraction, lid lag in downgaze
Test depression without holding lids up first to note associated anomalies of lid movement.
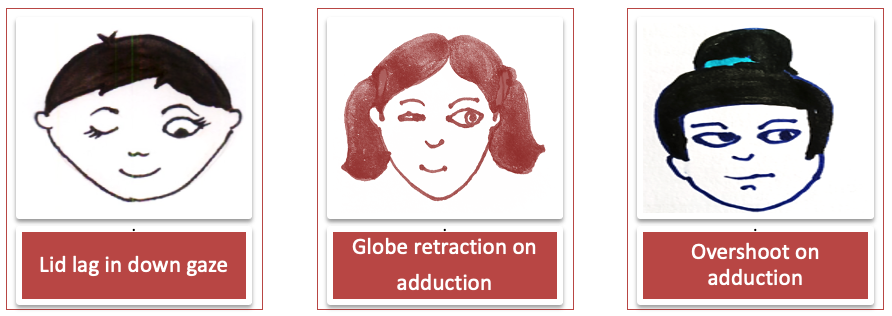
Abnormal eye movements
- Upshoots, down shoots, perverted convergence, nystagmoid movements
- Saccades: Horizontal and vertical, look for ocular-motor apraxia
- The briskness of the saccade is checked to differentiate paretic vs restrictive etiology of underaction
- Floating saccade → Paretic etiology
- Abrupt stop → Restrictive etiology
- Nystagmus if present should be described in detail
10. Torsion
- Assessed in all case of vertical tropias and pattern strabismus
- Torsion can be assessed objectively and subjectively
- Objective retinal torsion: The relationship of the fovea to the optic disc is determined using Indirect Ophthalmoscope. In patients with extorsion fovea is shifted below the inferior border of the optic disc, whereas in those with intorsion fovea is located higher than the midpoint of the optic nerve. However, the fundus view through the indirect ophthalmoscope is inverted resulting in fovea above the upper border of the disc in extorsion and fovea below the midpoint of the disc in intorsion.
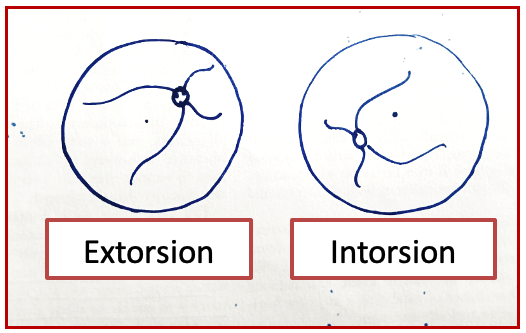
- Subjective torsion: Maddox Rod. A person with intorsion sees the top of a vertical line tilted temporally and extorsion will cause the top of a vertical line to appear to be shifted nasally.