Synonyms: Stilling–Turk–Duane syndrome.
Duane Retraction Syndrome is a type of congenital cranial dysinnervation which occurs in 1-4% of strabismus cases. It has varied presentation mostly involving variable horizontal duction deficits, with narrowing of the palpebral fissure and globe retraction on attempted adduction, occasionally accompanied by upshoot or down shoots
Etiopathogenesis
Various theories have been proposed earlier for the cause of DRS but currently, the most accepted theory is that of innervational anomalies which leads to all the features of DRS. It is considered to be a part of congenital cranial dysinnervation syndrome as it’s a developmental anomaly of the 6th cranial nerve or its nucleus leading to innervational deficiency of lateral rectus muscle which might be associated with secondary innervational abnormality with Medial rectus. The lack of normal innervations of lateral rectus was proved by electromyographic 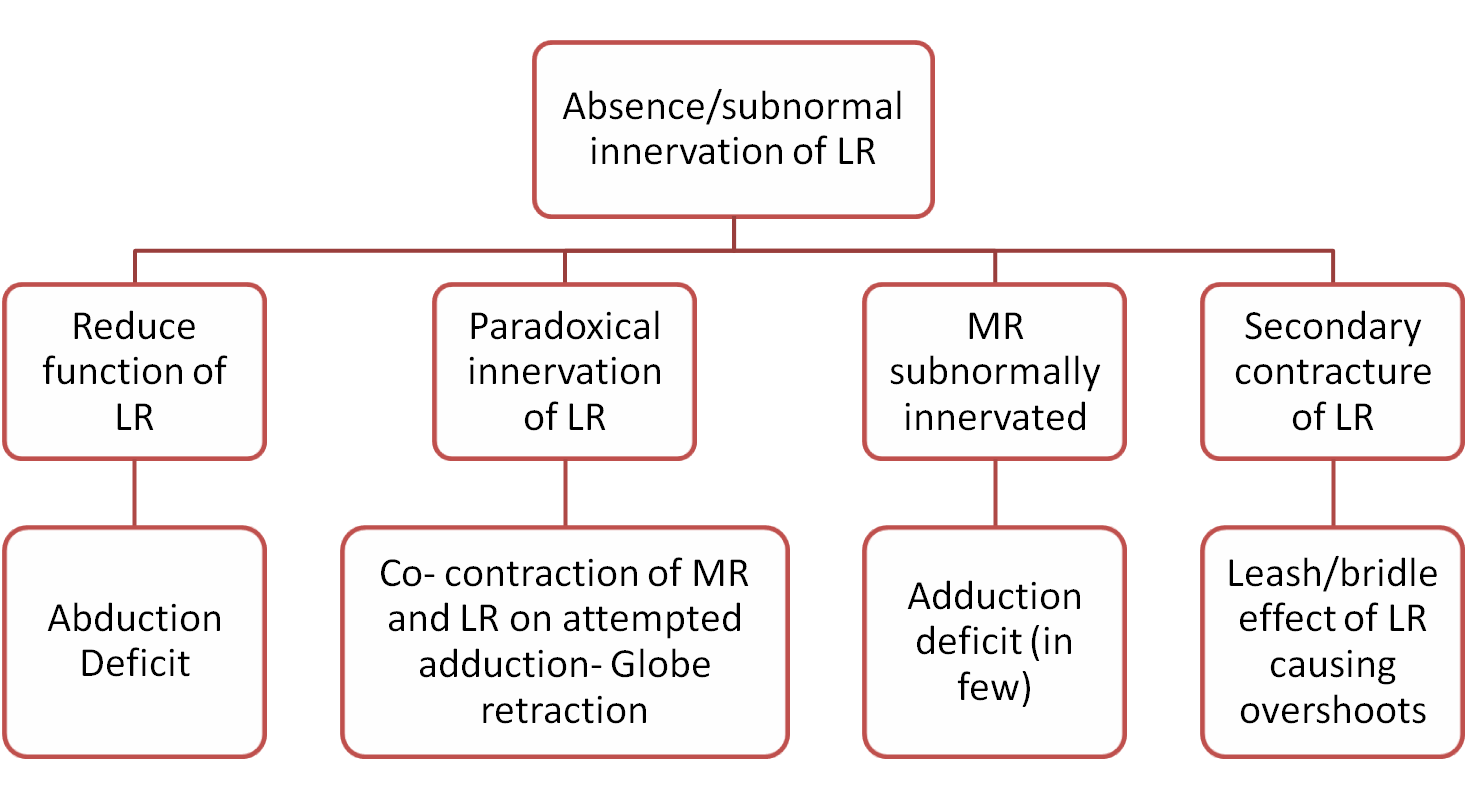 studies. It is also associated with paradoxical innervation of medial rectus by the third cranial nerve. Various synergistic innervations of vertical muscles have also been noted. The pathogenesis can be summarized as follows,
studies. It is also associated with paradoxical innervation of medial rectus by the third cranial nerve. Various synergistic innervations of vertical muscles have also been noted. The pathogenesis can be summarized as follows,
Genetic role it is commonly sporadic with the possible gene responsible are PHOX2A, HOXA1, and ROB03 and around 10 % have been found to be familial with autosomal dominant inheritance with a mutation in CHN1, DURS1, and SALL4. The pathogenesis of DRS is responsible for various combinations of clinical features that are found in DRS.
Classification:
The two most common system of classification is as follows
Huber’s classification based on EMG findings
|
Type I (70-80%) |
Type II(7%) |
Type III(15%) |
|
|
AHP |
Face turn to the same side |
Face turn to the opposite side |
May or may not be there |
|
EOM |
Marked limitation of abduction with minimally defective adduction |
Marked limitation of adduction with primary position exotropia of the affected eye, abduction normal or slightly limited |
Limitation or complete absence of adduction and abduction |
|
PALPEBRAL FISSURE HEIGHT |
Narrowing on adduction and widening on abduction |
Narrowing on attempted adduction |
Narrowing on attempted adduction |
|
GLOBE RETRACTION |
On adduction |
on attempted adduction |
on attempted adduction |
|
EMG FINDINGS |
Paradoxical innervations of the LR with maximum impulses on adduction and defective impulses in an attempted abduction. MR was found to have normal electric behavior |
LR showed peak impulses on abduction and a second paradoxical impulse on attempted adduction, while the electrical activity of MR was normal |
simultaneous innervations of MR and LR in primary gaze, adduction, and abduction |
This classification was further modified and subgroups based on alignment in primary gaze as A, B, and C indicating esotropia, exotropia, and orthotropia respectively.
Classification of DRS based on primary gaze deviation
- Esotropic DRS
- Exotropic DRS
- Orthotropic DRS
Other Variants of DRS
A.Congenital adduction deficit with synergistic divergence: Sometimes also known as type 4 DRS. It could be considered a variant of Huber’s type 2 DRS. It is characterized by an adduction deficit with paradoxical abduction on attempted adduction. It may be associated with large exotropia, head turn to the opposite side and abducting nystagmus on attempted adduction
B. Vertical retraction syndrome: A rare entity characterized by a variable amount of limitation of elevation or depression associated with globe retraction or decrease in palpebral fissure height. The affected eye can be either orthotropic, hypertrophic or hypotropic. Some proposed it as type 5 DRS.
C. Y-pattern deviation: Also proposed as type 6 DRS addition in Huber’s classification. This is characterized by co-contraction of inferior rectus along with lateral rectus giving a Y-pattern by causing the elevation in an attempted abduction.
D. Inverse Duane’s syndrome: A rare form which is characterized by limited abduction which may be accompanied by retraction of the globe, narrowing of palpebral fissure and pseudoptosis on attempted abduction
Acquired or Pseudo-DRS: features of inverse DRS secondary to various acquired causes like,
|
Mechanical |
Neurogenic |
|
Trauma and orbital fracture involving medial orbital wall |
Head injury |
|
Bony orbital metastasis |
Intracranial surgery |
|
Orbital surgery or squint surgery |
Brainstem tumors such as glioma, skull base meningioma |
|
Thyroid myopathy |
|
|
Myocysticercois |
|
|
Conjunctival surgery causing scarring eg.- pterygium surgery |
Clinical features :
1.Demography: Despite being congenital, the age of presentation may be variable. Female preponderance is noted in many studies. The majority are unilateral in occurrence.
2. Hypermetropia is noted in most of the patients and anisometropia is the common cause of amblyopia.
3. Abnormal head posture: Face turn is commonly noted in unilateral esotropic and exotropic DRS. AHP is to maintain a Binocular single vision. Sometimes, in orthotropic DRS also, the patient can keep AHP to avoid visual discomfort due to upshoots or down shoot.
4. Deviation Esotropia is the most common type of deviation noted. And the amount of deviation is usually small. Measurement of deviation by a cover test is important in all gazes with no head posture even in orthotropic DRS to get it accurately and also not to miss any pattern strabismus which commonly seen in bilateral orthotropic DRS.

Figure1 Left Eye Esotropic DRS

Figure2 Left eye esotropic DRS on adduction showing narrowing of palpebral fissure height (PFH)

Figure3 Left eye esotropic DRS showing abduction deficit and increase in PFH
5. Extraocular movements (EOM)is a very important clinical feature. The limitation of abduction is most common. The deficit in extraocular movement is not related to deviation in the primary gaze which is mostly very small and this is because of the underlying adduction deficit.
6. Anomalous eye movements and globe retraction :
Upshoot and down shoot are of two types-
A. Sudden overshoot is commonly associated because of mechanical “leash/bridle effect” due to sudden slippage tight lateral rectus muscle during adduction. If it occurs even with very small movement in adduction, it is called as “knife-edge effect”. To look for it, with the involved eye in adducted position, draw an imaginary straight line parallel to the intermediate canthal line from the pupillary center of the fellow eye and note the position of other eye. In the case of upshoot, the eye moves up and the pupil and limbus are not in the same position as other eye. Similarly, in down shoot, the affected eye shows a downward movement.

Figure: 4 showing upshoot of the left eye in attempted adduction along with narrowing PFH
B. Gradual upshoot or down shoot: there is a gradual vertical movement of the eye as eye turn from abduction to adduction and this is due to the international effect in which there are anomalous paradoxical innervations of lateral rectus by the oculomotor nerve. These patients will have vertical tropia even in primary gaze.
Globe retraction is noted in DRS when there is co-contraction of the both LR and MR in attempted adduction. It is clinically observed and measured by the amount of reduction in PFH (figure:4).
Association of DRS
Ocular associations
|
External ocular features |
Anterior segment |
Posterior segment |
|
|
|
Systemic associations
|
Associations |
Features |
|
Goldenhar’s syndrome |
Limbaldermoid, preauricular skin tags, incomplete development of ear, nose, soft palate, lip and mandible |
|
Klippel-Feil syndrome |
Short neck, low hairline at the back of the head, scoliosis, deafness, cleft palate |
|
Holt–Oram syndrome |
Hypoplasia or aplasia of digital rays or radius associated with congenital heart disease |
|
Wildervanck syndrome |
Combination of Klippel –Feil anamoly, DRS and hearing loss |
|
Congenital Arthrogryposis multiplex |
Multiple joint contracture leading to various skeletal deformity |
|
Rubinstein- Taybi syndrome |
Short stature, intellectual disability, broad thumbs, and first toe, cardiac and renal anomalies |
Differential diagnosis
1. Infantile esotropia – can be differentiated from esotropic DRS as follows
|
Infantile esotropia |
Esotropic DRS |
|
|
Age at presentation |
Earlier age- from birth to 6months |
Later age- mostly after 5 years |
|
EOM |
Apparent limitation of abduction |
Limitation of abduction noted in the affected eye |
|
Globe retraction |
Absent |
Usually present |
|
Change in PFH |
Absent |
Usually present |
|
Overshoots |
Absent, associated Inferior oblique overaction is present in most of the cases |
Usually present |
|
Abducting saccades |
Normal |
Slow |
2. Abducens nerve palsy Congenital form appears like esotropic DRS, and all congenital 6th nerve palsies are DRS unless proven otherwise. Differentiating points are
|
Congenital 6th Nerve Palsy |
Esotropic DRS |
|
|
Age of presentation |
Earlier- mostly by 2 years |
Later – mostly after 5 years |
|
Angle of deviation |
large and corresponds with EOM limitation |
Usually less and not corresponding to the EOM limitation |
|
Globe retraction |
Very minimal and mostly in long-standing cases |
Seen prominently |
|
PFH changes |
Not much change even in long-standing cases |
Usually seen |
|
Overshoots |
Rarely seen in long-standing cases |
Often present |
|
Pattern |
V-pattern |
An outward curved rotation like X-pattern |
Management of DRS
Predictability of surgical outcome is low as compared to conventional strabismus surgery, hence it is important to have a clear-cut indication for surgery. Following are
Indications for Surgery :
- Primary gaze deviations
- Gross anomalous head posture
- Cosmetically unacceptable severe globe retraction, upshoot or downshoots
The goal of surgery-
- Expanding the field of binocular single vision
- Eliminating the compensatory AHP
- Reducing the upshoot and downshoot
- Improve the ocular motility
While planning surgery it is important to look for contracture or fibrosis of both medial rectus and lateral rectus. Hence, various force duction test (FDT) has a role. One important variant of FDT is theForce degeneration test of Romero-Apis.
It is useful to demonstrate the anomalous innervation of the LR muscle. It is done once it is confirmed by other FDT test that there are no normal or subnormal active innervations of LR. It confirms LR innervation during adduction and the missing LR innervations on abduction and thus helps in deciding the plan of surgery.
Procedure:Ask the patient to look halfway between primary position and adduction and then using forceps try to move eye passively further towards adduction. If the LR muscle has anomalous innervations, it will co-contract, and hence a restriction will be felt in forceps.
Again from the same midway position between primary gaze and adduction, the patient is asked now to abduct the eye while using forceps examiner tries to adduct the eye again. Attempt to abduct will relax MR and if LR has anomalous innervation, the LR co-contraction also goes away and it will be easier to move the eye in adduction by forceps.
SURGICAL OPTIONS :
The surgical treatment options are
|
To correct primary gaze deviation |
The recession of the appropriate horizontal rectus muscle of the affected and/or the sound eye |
|
Globe retraction |
The recession of both horizontal recti (more in one muscle) Y Split of LR |
|
Upshoots/Downshoots |
Y Split of LR LR inactivation by periosteal fixation. |
|
Improve Abduction |
Vertical rectus transposition |
Depending upon the various clinical features noted in a particular case of DRS the surgery has to be tailored and customized.
Management of Individual type of DRS
Esotropic DRS
Medial rectus recession: unilateral or bilateral ( symmetrical or asymmetrical bilateral recessions) corrects primary gaze esotropia
To improve abduction: Half tendon vertical rectus transposition ( Hummelsheim procedure ) with or without augmentation sutures Superior rectus transposition (figure 5) to Lateral rectus with or without augmentation

Figure5: diagrammatic representation of SRT
In presence of LR anomalous activity ( co-contraction / globe retraction/shoots) VRT and SRT are not advocated
Globe retraction: Recession of MR and LR simultaneously
Upshoots/ down shoots : ( mechanical )
Y split of LR –The splitting of the ends of the lateral rectus muscle into a Y-configuration is a unique idea first advocated by Jampolsky. Lateral muscle slips off leading to down shoot or upshoot of the globe. The bifurcation of the muscle decreases the upward or downward rotation of the globe because the halves are positioned to stabilize the muscle’s position on the eye as shown in the figure below. Each muscle arms are vertically transposed such that the two arms are spread apart a total of 20 mm and each arm is recessed appropriately.

Figure- 6 showing mechanism of down shoot due to LR slippage

Figure 7 showing how Y splits works
Though in general, resections/plications are not recommended in DRS but LR resection in select cases proves useful.
LR resection with the recession of MR should be done only if adduction is normal with minimal abduction limitation and no other anomalies of globe retraction and overshoots. It is useful in ET of around 25 PD.
To summarise
|
Management of Unilateral esotropic DRS |
||
|
Without co-contraction or overshoots |
With co-contraction |
|
|
<15 PD |
SRT MR recession |
MR recession with LR recession alone LR recession with Y- split |
|
>15 PD |
SRT or augmented SRT with MR recession Bilateral MR recession |
|
|
Management of BIilateral esotropic DRS |
|
|
Without co-contraction or overshoots |
With co-contraction |
|
Bilateral MR recession alone Bilateral MR recession with SRT |
MR recession with LR recession with or without Y splits for upshoot or down shoot |
Exotropic DRS
Usually seen in Hubers type 3 and type 2 DRS. Exotropic DRS is commonly associated with overshoots and globe retraction.
Possible surgical options are
Lateral rectus recession - unilateral or bilateral ( symmetrical or asymmetrical bilateral recessions) corrects primary gaze exotropia
For large XT with co-contraction: LR is completely inactivated either by Supramaximal recessions of LR or periosteal fixation of LR. With the latter abduction is lost and VRT will be needed along with it. ( partial or full VRT )
Periosteal fixation – the principle of this procedure in DRS is the deactivation of an inappropriately-innervated muscle and thus conversion of a complicated abnormal co-contraction case into more straightforward paralytic strabismus. The procedure involves detaching the muscle from its insertion and re-attaching it to the periosteum of the orbital wall. (Figure-8)

Figure 8: Diagrammatic representation of periosteal fixation of LR to the lateral orbital wall.
To summarise
|
Management of Unilateral/ Bilateralexotropic DRS |
||
|
With normal LR activity |
Without normal LR activity |
|
|
No overshoots or globe retraction |
LR recession |
LR periosteal fixation with or without pVRT The supramaximal recession of LR with or without pVRT |
|
With overshoots |
LR recession with Y-splits |
|
Orthotropic DRS :Surgery is indicated only if there is severe co-contraction or overshoots. The possible surgical options as described above are 1. For co-contraction of globe-recession of both LR and MR in the affected eye in the presence of co-contractions 2. For overshoots- Y-split on LR.
Conclusion
DRS is a non-progressive congenital cranial dysinnervation syndrome. The diagnosis is based on clinical features. There are many surgical options and have to be customized according to the clinical features noted in the patient.
Suggested reading
1. Jampolsky A. Duane’s retraction syndrome in Rosenbaum A, Santiago A. Clinical strabismus management. Philadelphia: Saunders; 1999. p. 325-346. 2. Özkan SB. Pearls and pitfalls in the management of Duane syndrome. Taiwan J Ophthalmol 2017;7:3-11. 3. Gaur N, Sharma P. Management of Duane retraction syndrome: A simplified approach. Indian J Ophthalmol 2019;67:16-22. 4. Kekunnaya, R.,Negalur, M.Duane retraction syndrome: causes, effects, and management strategies. Clinical Ophthalmology, 2017.Volume 11, 1917–1930. 5. Kekunnaya R, Kraft S, Rao VB et al., Surgical management of strabismus in Duane retraction syndrome. J AAPOS 2015;19:63-69 6. Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol 2012;130:195-201

1.jpg)