Introduction:
Keratoconus is a degenerative non-inflammatory disease of the cornea. It presents generally at puberty with progressive corneal steepening & thinning, most typically inferior to the center of the cornea. Keratoconus is characterized by progressive Myopia, both regular and irregular astigmatism in mild cases and vision compromising ectasia in advanced disease. It is usually bilateral and asymmetrical. The incidence of keratoconus is 1 in 2000. Patients often present with complaints of distorted, blurred vision, glare, light sensitivity and history of frequent change of glasses.

PATHOGENESIS:
Despite extensive research the etiology and exact pathogenesis of keratoconus is still not clearly established. It has been associated with atopic disease and chronic eye rubbing like in patients with Down’s Syndrome & Atopic dermatitis.
There has been a possibility of genetic and hereditary disposition. It has been associated with systemic diseases like the Ehler-Danlos syndrome, osteogenisis imperfect leading to a speculation that it may be part of a connective tissue disorder. Long term contact lens wear with resultant corneal warpage has also been implicated as a possible cause for keratoconus.
Biochemical abnormalities:
Studies in patients with keratoconus have demonstrated an increased activity by proteases that breakdown the collagen cross-linkages in the corneal stroma. There is a simultaneous reduced expression of protease inhibitors. The ratio of keratin sulfate to dermatan sulfate is altered in the stromal matrix when compared to normal corneas.Patients with keratoconus have also shown enzymatic changes in the epithelium with increased expression of lysosomal and proteolytic enzymes.
DIAGNOSIS OF KERATOCONUS:
Early signs
- Scissoring of retinoscopic reflex
- Distortion of placido disc mires
- Keratometry- shows irregular astigmatism where the principal meridian are not 90* apart and mires cannot be superimposed.
- Direct ophthalmoscopy from a distance shows an oil droplet reflex
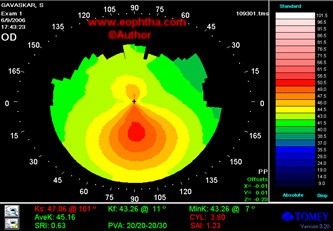
- Typical inferior steepening on topography
These early signs occur even before the appearance of classic corneal signs .
Clinical characteristics
- Munson’s sign-Angulation of the lower lid margin when the patient looks down
- Vogt’s striae- fine, vertical deep stromal striae which disappear with external pressure
- Fleischer’s ring –Epithelial iron deposits at the base of the cone
- Stromal scarring in advanced keratoconus
Acute Hydropsresults from rupture of the descemet’s membrane and the overlying endothelium in a keratoconic eye. Aqueous enters the corneal stroma through the ruptured DM and causes a stromal swelling and a spongy elevated area of with overlying bullous edema of the epithelium. Visual acuity drops considerably with congestion of adjacent conjunctiva .Spontaneous resolution occurs in few months with resultant scarring.
Management would consist of supportive therapy in the form of lubricant drops, hypertonic saline and soft contact lens .Steroid drops can be used if the eye is congested.
Thermokeratoplasty has been tried by Aquavella & group. They believe shrinkage of the collagen with resultant flattening of the hydrops helps in early healing of the ruptured DM.
Systemic associations
Down’s syndrome
Ehlers-Danlos syndrome
Osteogenesis Imperfecta
Mitral valve prolapsed
Ocular associations
Retinitis Pigmentosa
Leber’s Congenital Amaurosis
Microcornea
Aniridia
Corneal Degeneration
Congenital Cataract
Ectopia lentis
Lenticonus
Macular coloboma
Retinal dysplasia
Floppy eyelid syndrome
MANAGEMENT OF KERATOCONUS:
The management of keratoconus depends on the stage of the disease the patient presents with. The various modalities available today can be broadly divided into nonsurgical & surgical.
NON-SURGICAL MODALITIES:
Spectacles can be used in early stage of the disease before irregular astigmatism sets in.
Contact lenses are the main stay of nonsurgical management in moderate & advanced keratoconus. Contact lenses used in keratoconus can be broadly classified into-
Rigid gas permeable lenses:They are the main stay of optical management of keratoconus. The contact lens resurfaces the irregular cornea & the intervening fluid lens corrects the irregular astigmatism to provide good quality of vision. However the disadvantage with these lenses is that they have standard lens design with fixed optical zones and do not give an ideal fit in patients with keratoconus
Piggy-back lenses:they are known as piggy back because a RGP Lens is fitted on top of a soft contact lens. These lenses provide excellent comfort and good vision. The down side to this fit is the need to have two lenses care systems.

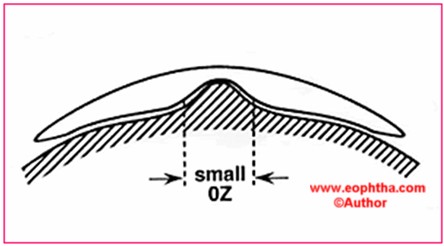
Rose-K Contact lenses:As the cornea becomes more conical, the base curve steepens only in the area of the cone and hence the difficulty in fitting contact lenses. The Rose-k lenses are made with complex geometry to fit any type of cone. The optical zone is reduced to snuggly fit the cone & the peripheral curve is computer designed to fit the rest of the irregular cornea. It demonstrates the benefits of a smaller optical zone to fit the cone contour. The design results in little tear pooling at the base of the cone and show an even distribution of tears under the lens. It has a large inventory and is easy to fit. .The Rose K™ system has set optical zones to maximize vision while maintaining good corneal health.
Contact lens design can be made in any diameter with spherical back surface, toric back, front, bitoric or peripheral toric design. In patients with very steep and sagging cones, fitting is very difficult since the cornea steep in the periphery and flat in the area away from the cone. With the Advanced Corneal Technology (ACT) available in the Rose K2 system the lens can be steepened at the area of the cone. With ACT, 3 grades of steepening can be made at the 6 0’ clock positions which provide good stability to the lens. Rose K lenses are made of Boston ES, a special material with high oxygen permeability.
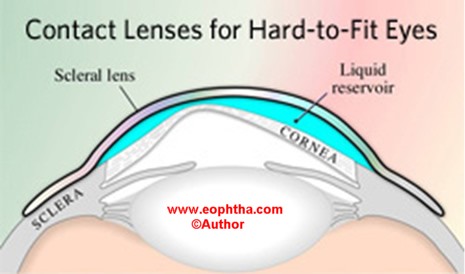
Scleral Contact Lenses:They are made of a special polymer called Itaflurocon. They characteristically vault over the cornea and limbus and are supported entirely by the sclera. The fluid lens smoothens the irregular cornea and provides good vision. It also prevents dessication due to its very high oxygen permeability. The small pores on the lens provide adequate exchange of tears. The disadvantage with these lenses is that they are difficult to use. They are large lenses which are cumbersome to the patients .
Boston Scleral Contact lenses(BSLP):BSLP lenses are made of Flurosilicone Acrylate Polmers with DK values of 87 and 130. Its diameter ranges from15.5mm to 20mm.the space created over the cornea is filled with non-preserved, buffered sterile saline. The shape of each lens is based on a master design template. The shape of the haptic scleral bearing is controlled by spline a function which is adjusted to create the desired fitting relation ship even in advanced cones. The limitation to the use of these lenses are that the fitting process is skill intensive and time-consuming.
SURGICAL MODALITIES:
About 10 to 25% of keratoconus progresses to a condition where extreme thinning or scarring warrants a keratoplasty. The various options available are epikeratoplasty, deep anterior lamellar keratoplasty, and penetrating keratoplasty
EPIKERATOPLASTY:
In epikeratoplasty, the corneal epithelium is removed, followed by a annular keratectomy 0.3 mm deep encompassing the cone and a lenticule of donor tissue is grafted on top of it. Alternatively an annular lamellar dissection is carried out and the lenticule is tucked into the host and sutured tightly. This compresses the cone and reduces the irregular astigmatism. However the problems associated with donor –recipient mismatch can result in poor epithelialisation of the graft- host junction. This procedure requires good surgical skills and is rarely done now.
DEEP ANTERIOR LAMELLAR KERATOPLASTY (DALK):
DALK can be defined as a procedure in which the anterior layers of the cornea are removed up to the pre-descemets level & replaced with donor cornea in order to achieve the best possible visual rehabilitation
.
The advantages of DALK are that it is an extra-ocular procedure, with fewer chances of intraocular complications. The incidence of rejection is reduced considerably since the endothelium of the host is preserved . Suture removal can be done early with early visual rehabilitation. Since endothelium of the donor is not used, donor tissue criteria is less stringent.
The major disadvantages of this procedure are that it is technically more challenging and requires excellent surgical skills. Other problems associated with this procedure are the development of interface haze, persistent epithelial defect again due to poor donor-recipient mismatch. Some patients in spite of best possible results still complain of poor visual quality particularly if the other eye had undergone a penetrating keratoplasty.
Techniques of DALK:
One of the most important criteria for good visual results after DALK is to do a lamellar dissection up to the level of the descemets membrane. Though several methods have been described, the most popular one is the Big Bubble technique of Anwar. Here injection of air bubble into the deep stroma creates a space between the posterior stroma and descemets, which helps the surgeon to achieve the dissection with relative ease. However in patients with history of previous hydrops with descemets rupture, a full thickness penetrating keratoplasty is mandatory.

Fig: Big Bubble technique
Various other surgical modalities of achieving the lamellar dissection that has been described are direct open dissection, Malbran's peeling technique, visco dissection of Melles and saline hydrodelamination of sugitos. One of the newer and most exciting developments in lamellar corneal surgery are the Microkeratome and Femtosecond assisted Lamellar Keratoplasty.

Fig: Corneal button sutured

Fig: Descemets exposed
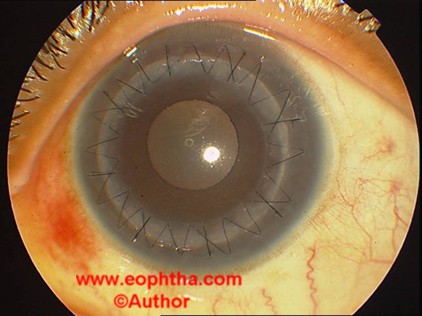
Fig: DALK(deep anterior lamellar keratoplasty)
Intraoperative complications:
Inadvertent perforation into the anterior chamber can happen particularly in extremely thin corneas with advanced cones. In cases with small or medium perforations the procedure can be completed without any compromise on the ultimate result. However in patients with large perforations it is mandatory to convert to penetrating keratoplasty
Post-operative complications:
Double anterior chamber can occur in patients with inadvertent small perforation due to influx of aqueous into the potential space between the donor and the recipient. Injection of air into the anterior chamber to push the descemets and endothelium towards the posterior stroma of the donor lenticule is the recommended modality of treating this unique problem. Other problems associated with DALK are descemet's folds and delayed epithelialisation due to graft-host mismatch. The persistent epithelial defect (PED) can lead to a stromal melt. Interface haze, epithelial ingrowth and infections in the graft can also occur.
Late post-operative complications:
Interface haze and high astigmatism with sub optimal visual acuity can occur in patients as late complications of DALK.
INTACS:
Intacs are now a well-established procedure in the treatment of early to moderate cones.
Intrastromal corneal ring segments (Intacs Addition Technology Inc) have crescent shaped two 150-degree PMMA segments that are surgically placed in the peripheral cornea at two-thirds corneal depth. Intacs comes in thickness ranging from .25 to .45 mm in .05 mm increments. Intacs correct the myopia and irregular astigmatism by producing a mechanical flattening of the central cone. Intacs segments act as passive spacing elements, shortening the arc length of the anterior corneal surface, flattening the central cornea and provide biomechanical support to the thin ectatic cornea. The thickness of the inserts determines the amount of correction achieved.
The advantages of Intacs are they are reversible. In case of sagging peripherally placed cones even a single segment can be used to provide preferential flattening of the cone and steepening of the flat area above the cone. It can also be combined with corneal collagen cross-linking.
The creation of the intrastromal corneal tunnels can be done mechanically or by using femtosecond laser. The laser delivers the energy to create a tunnel and entry incisions at the appropriate depth with little risk of corneal perforation.
The various complications associated with the creation of the tunnel mechanically are epithelial defects at the incision site, anterior & posterior perforations during channel creation, extension into the visual axis or limbus, shallow or uneven placement, and infectious keratitis.The femtosecond laser reduces these complications because of the more precise localization of the channel with appropriate depth, dimension and width.

Fig: INTACS
CORNEAL COLLAGEN CROSS-LINKING (C3R/CXL):
This therapeutic option is based on the fact that, the biomechanical strength and resistance of the cornea is largely dependent on the 3-dimensional configuration of the collagen lamellae. The basic problem in keratoconus is the weakness of the cross links which act as anchors between the collagen fibrils UV-A irradiance of the cornea after sensitization with riboflavin, augments these cross-links, and hence recovers some of the corneal mechanical strength in keratoconus. This treatment modality stabilizes the collagen scaffold and increases the stiffness of the cornea against the action of proteolytic enzymes. Riboflavin/UVA light causes There is increase in the corneal stiffness of the anterior 200-250 μm Deeper structures like the lens and endothelium do not get damaged.The progression of keratoconus or keratectasia can be stopped. This is an easy and simple treatment with low costs. If there is progression, an early cross-linking treatment is recommended.

Fig: Application of riboflavin drops for 20 minutes for every 2 minutes
Procedure:The procedure consists of
- Removal of 8-9mm of epithelium under topical anaesthesia.
- Application of 0.1% riboflavin drops for 20 minutes for every 2 minutes
- Exposure to UV-A light with a wave length of 370 nm and irradiance of 3mw/cm2 for 30 minutes.

Fig: Exposure to UV A rays
During this period riboflavin is applied every 4-5 minutes to sustain the concentration of riboflavin in the corneal stroma. The eye is patched with antibiotic eye ointment till the epithelium heals. During the post-operative period flurometholone and artificial tears are applied for a period of one month. In the pilot study done on 23 eyes and followed up to 4 years Wollensaket alfound a mean reduction in steepening of 2.01 D. Other investigators such as caporossiet aland Krumeichet alreported a similar result.
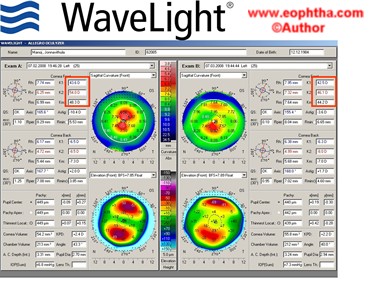
Fig:Pre and Post Topography of Collagen cross linking
The improvement in vision after cross-linking is caused by a decrease in astigmatism and corneal curvature as well as topographical homogenization of the cornea as a result of the increased rigidity in the cross- linked cornea. In addition tolerance to contact lenses improved. Cross-linking is a practical out patient treatment, which is minimally invasive and cost-effective.
Though various modalities of treatment are available for management of Keratoconus, collagen cross-linking is the only modality proven to stop the progression of keratoconus. Most of these patients present in their teens and early treatment can reduce the morbidity and the number of keratoplasties.
At present Keratoconus is not curable but early cross-linking can stop its progrssion. Further improvement in vision can be achieved by combining cross-linking with Intacs, topography-guided photorefractive keratectomy and thermal keratoplasty an area under clinical research.
CONCLUSION:
Management of Keratoconus is often complex and differs at different stages of the disease. Special attention should be given to optimize visual outcome depending on the need of the patient. Corneal collagen cross- linking should be considered as a treatment modality in patients with progressive disease. Since most of the patients present at a very young age it is important to reduce the morbidity associated with this disease & give a better quality of life to the patient. This review is by no means complete and extensive but is aimed at providing an overview of keratoconus management for the practicing ophthalmologist
References:
1. Keratoconus and non-inflammatory thinning disorders. Howard. M. Leibowitz, Sergio Morello Jr. CORNEAL DISORDERS. CLINICAL DIAGNOSIS AND MANAGEMENT
2. Edward S. Bennet, O.D.MS.Ed Barry A.weissman od Ph.D . CLINICAL CONTACT LENS PRACTICE
3. Intacs insertion with femtosecond laser in the management of keratoconus-Aylin ertan JCRS 2006 32; 2039-2042
4. Effect of inferior segment Intacs with and without C3-R on Keratoconus-colin c.k. chan,Brian Boxer Wachler JCRS 2007 33;75-80.
5. Corneal Transplantation –Rasik Vajpayee, Section 4 Lamellar Keratoplasty
6. Collagen cross linking with riboflavin and ultra-violet –A light in Keratoconus; long term results Frederik Raiskup-Wolf, Anne Hoyer Eberhard Spoerl JCRS 2008 34;796-801
