Chief Complaint:
A female patient of 58 years old who came for a routine eye examination.
History of Present Illness:
No specific complaints.
Past Ocular History:
No H/O any previous injury.
Past Medical History/ History of Medication:
Known diabetic for the past 10 years and on control with oral hypoglycemic agents.
Family History:
No significant family history.
Review of Systems/Systemic Examination
Pulse rate - 88/min, respiratory rate - 16/minute. BP- 120/80 mm Hg. Examination of other systems were normal.
Ocular Examination
Best Corrected Visual Acuity (Snellen)
- Right eye (OD): 6/6 p N6
- Left eye (OS): 6/6 N6
Ocular Motility/Alignment
Extraocular motility was full and free in all gazes in both eyes.
Intraocular Pressure (IOP)- By Applanation tonometry
- Right eye (OD): 14mm
- Left eye (OS): 16mm
Pupils:
Both eyes (OU) - round and briskly reacting to light.
Slit-lamp examination:
- Lids/lashes:
Both eyes (OU)- normal.
- Conjunctiva/sclera:
Both eyes (OU) - normal.
- Cornea:
Both eyes (OU) – clear.
- Anterior chamber:
Both eyes (OU) – normal in-depth and quiet.
- Iris:
Both eyes (OU)- normal in color and pattern.
- Lens:
Both eyes (OU) - Nuclear sclerosis grade 1.
Dilated Fundus examination
- Vitreous:
Right eye (OD) – Asteroid hyalosis.
Left eye (OD) – Clear.
- Disc:
Size, shape, color and margins are normal in both eyes.
- Macula:
Right Eye (OD) – shows hard exudates in the supero-temporal region of the macula and few microaneurysms.
Left eye (OS) - showed few microaneurysms.
- Vessels:
Both eyes (OU) – normal.
- Retinal examination and Periphery:
Right eye (OD) – Normal.
Left eye (OS) – Normal.
Ancillary Investigations:
Fundus photo:
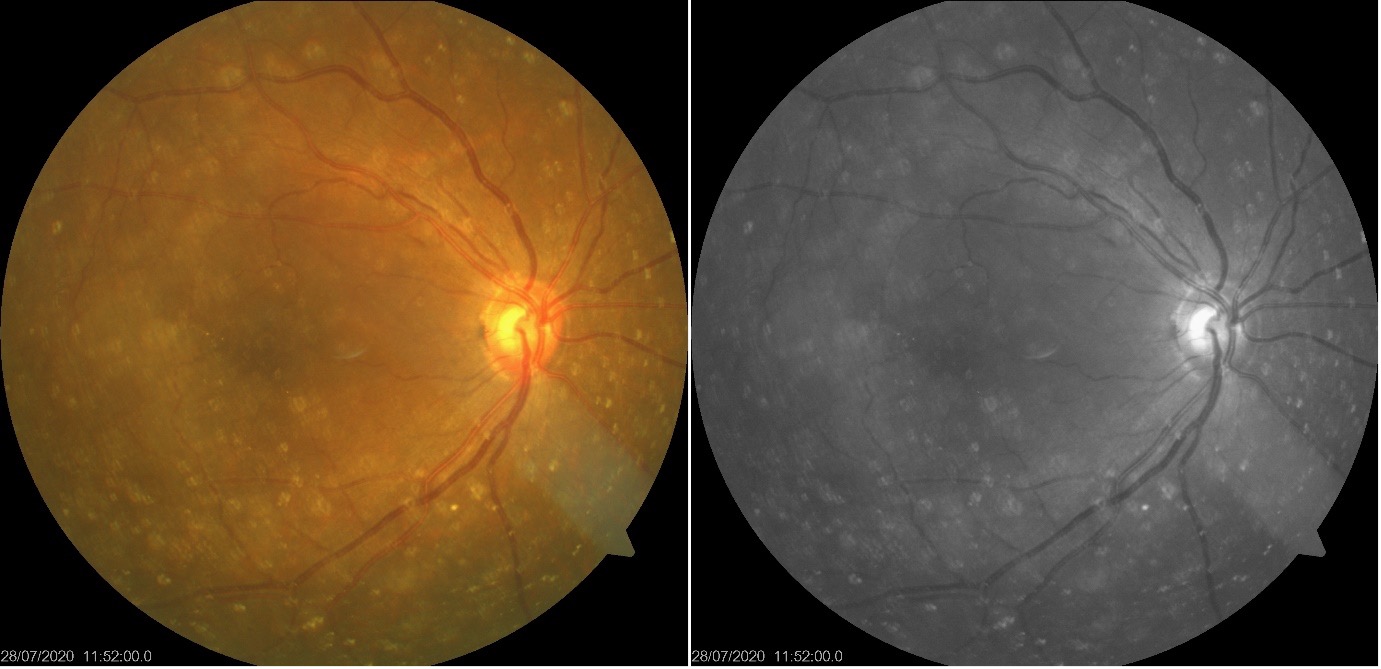
This is the fundus photo and red-free photo of the right eye showing yellow-white opacities in the vitreous suggestive of asteroid hyalosis and few hard exudates temporal to the fovea.
B Scan ultrasonography of the right eye:
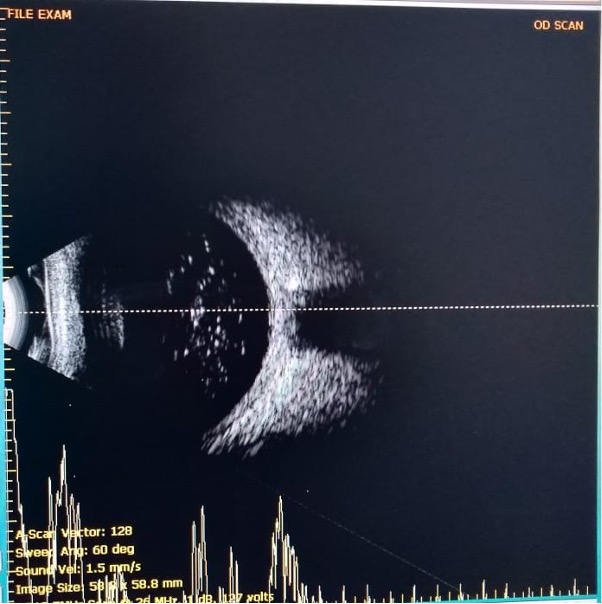
This is the B scan of the same patient showing bright high spiked echoes in the vitreous and a lucid zone between the vitreous echoes and retina.
Clinical Course of the condition:
The patient came for a routine eye checkup, particularly for glasses. She was advised optical coherence tomography of the macula and fundus fluorescein angiography to look for the extent of diabetic macular edema in the midst of asteroid hyalosis but got lost to follow up.
Differential diagnosis:
-
- Synchisis scintillans
- Amyloidosis
- Severe vitritis
- Malignancy like lymphoma and metastatic carcinoma
- Old vitreous hemorrhage
Difference between asteroid hyalosis and Synchisis scintillans
|
Asteroid hyalosis |
Synchisis scintillans |
|
|
Age |
elderly |
Usually young |
|
Laterality |
Unilateral |
Bilateral |
|
Appearance |
yellow-white spherical bodies |
Multicoloured discoid crystals |
|
Mobility |
Moves with movement of vitreous and returns back to the original position |
Freely floating but settle down inferiorly in vitreous due to gravity |
|
Composition |
Calcium |
Cholesterol |
|
Associated ocular pathology |
Diabetes in certain cases |
Secondary to other ocular diseases and trauma |
|
Vitreous condition |
Normal |
Liquified |
|
Visual impairment |
none |
Depending on the underlying pathology |
Diagnosis:
Asteroid hyalosis.
Discussion
Description
Asteroid hyalosis (AH) is the degeneration of the vitreous wherein yellow-white calcium-lipid bodies are suspended in the vitreous. This entity was first described by Benson as “asteroid hyalitis” because of its resemblance to “stars on a clear night” appearance. He also differentiated this from synchisis scintillans. Luxenberg and Sime later coined the term “asteroid hyalosis” as there were no signs of inflammation [1].
Epidemiology and risk factors
The Gutenberg health study conducted in Germany estimated the prevalence of AH to be 0.5% and this was associated with male gender, diabetes, and advanced age in Europe. The five-year cumulative incidence was estimated to be 0.2%. It showed increased unilaterality of the condition [2].
The retrospective autopsy-based study conducted at the University of California at Los Angeles (UCLA) showed a higher prevalence of AH than the earlier studies. This study also showed that there was no statistically significant correlation between diabetes and AH and strongly correlated with age and inversely correlated with posterior vitreous detachment [3].
The Blue Mountains Study showed that the prevalence of AH was 2.1% in people aged 75 years or more and significantly higher in males (1.4%) than in females. It also showed increased unilaterality of the condition. There was no association with diabetes, smoking, gout, history of heart disease, or increase in alcohol consumption [4].
The Beaver Dam Study showed the prevalence of AH to be 1.25 in the middle-aged to the older population. It also showed increased prevalence in men and increasing age and no association with diabetes [5].
Pathophysiology
Asteroid bodies are rounded structures measuring about 10-100 nm and stain positively with alcian blue. They also stain positively for neutral fats, phospholipids, and calcium. They stain metachromatically and exhibit birefringence. Occasionally, they will be surrounded by foreign body giant cells but without any evidence of inflammation. Element mapping by electron spectroscopy has revealed a homogenous distribution of calcium, phosphorus, and oxygen. They exhibit structural and elemental similarity to hydroxyapatite. Immunofluorescence microscopy reveals the presence of chondroitin sulfate at the periphery of asteroid bodies [6,7,8}
Investigation
Fundus examination may be difficult in severe cases. Fluorescein angiography and ultrasonography may be used in such cases. Among optical coherence tomography (OCT), swept-source OCT has been shown to be superior to spectral-domain OCT. Multicolour imaging seemed to give a better image of the retina where color fundus photography could not. Optos ultrawide field imaging has been shown to be better in cases of severe AH interfering with fundus examination [9].
Complications
AH can abnormally cause the eye to be hyperopic during biometry because of the reflection from the bodies making the intraocular lens (IOL) power calculation difficult. Deposits have been shown on patients with silicone IOLs. AH can be an obstacle to laser photocoagulation delivery in patients with diabetic retinopathy or vein occlusions. Unusual bilateral presentation and progression of AH have been seen in patients with retinitis pigmentosa for which the mechanism has not been clearly understood. In some patients, a vitrectomy had to be performed to remove the vitreous bodies [9,10].
Asteroid hyalosis |
|
|
Epidemiology
|
Signs
|
|
Symptoms
|
Differential diagnosis
|
|
Investigations
|
Treatment
|
References
- Robert L. Bergren, Gary C. Brown and Jay S. Duker, Prevalence and Association of Asteroid Hyalosis With Systemic Diseases, American Journal of Ophthalmology, 111: 289-293, March 1991.
- Hisham Elbaz, Alexander K. Schuster, Stefan Nickels, Markus Nagler, Katharina I. Ponto, Thomas Munzel, Philipp S. Wild, Manfred E. Beutel, Irene Schmidtmann, Karl J. Lackner, Norbert Pfeiffer, Tunde Peto, Epidemiologic Analysis of Asteroid Hyalosis and Associations: The Gutenberg Health Study, Ophthalmology, 2021 Feb;128(2):328-330. doi: 10.1016/j.ophtha.2020.07.008.
- Amani A. Fawzi, Baotran Vo; Ryan Kriwanek, Hema L. Ramkumar, Chris Cha, Amy Carts; John R. Heckenlively, Robert Y. Foos, Ben J. Glasgow, Asteroid Hyalosis in an Autopsy Population.
- The University of California at Los Angeles (UCLA) Experience, Arch Ophthalmol. 2005; 123:486-490.
- Paul Mitchell, Maria Y. Wang, Jie Jin Wang, Asteroid hyalosis in an older population: The Blue Mountains Eye Study, Ophthalmic Epidemiology – 2003, Vol. 10, No. 5, pp. 331–335.
- Scot E. Moss, Ronald Klein and Barbara E. K. Klein, Asteroid Hyalosis in a Population: The Beaver Dam Eye Study, Am J Ophthalmol 2001;132:70–75.
- Ophthalmic pathology and intraocular tumours – AAO – Basic science and clinical science course section 4, 2015-2016, chapter 10, Vitreous Degenerations, Asteroid hyalosis.
- Winkler J, Lünsdorf H. Ultrastructure and composition of asteroid bodies. Invest Ophthalmol Vis Sci. 2001;42(5):902–907.
- Harvey W. Topilow, Kenneth R. Kenyon, Masataka Takahashi, H. MacKenzie Freeman, Felipe Tolentino, Laila A. Hanninen, Asteroid Hyalosis Biomicroscopy, Ultrastructure, and Composition, Arch Ophthalmol 1982;100:964-968.
- Matin Khoshnevis, Sasha Rosen, J. Sebag, MD, Asteroid Hyalosis - A comprehensive review, Survey of Ophthalmology, Volume 64, Issue 4, 452-462, July 01 2019.
- YasuhiroIkeda,ToshioHisatomi,YusukeMurakami,MasanoriMiyazaki,Ri-ichiro Kohno,Hiroshi Takahashi,Yasuaki Hata,Tatsuro Ishibashi Retinitis pigmentosa associated with asteroid hyalosis. Retina, 2010 Sep;30(8):1278-81. doi: 10.1097/IAE.0b013e3181dcfc0a.
