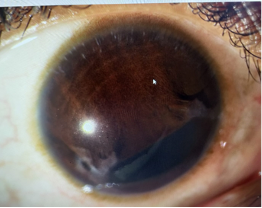
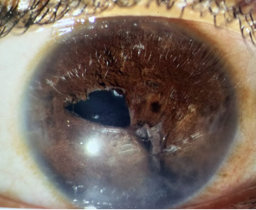
Trauma to the iris can present in various ways depending on its severity and location. Tearat the iris root leads to Iridodialysis, while tears at the pupillary border can damage the sphincter muscle, leading to a partially reactive, atonic or Mydriatic pupil. Tears can be full thickness or partial thickness. Full thickness defect involves the iris stroma and partial thickness involves only the posterior pigment epithelium leading to trans-illumination defects.
Etiology of iris defects:
Iris defects can be a consequence of either:
- Congenital (iris coloboma)
- Acquired
- Iatrogenic (iris lesion removal)
- Traumatic (traumatic mydriasis or injury resulting in pupil irregularity or muscle tear)
- Complicated intraocular surgery (can cause dialysis, atonic dilated pupil or iris tissue loss and injury)
Symptoms:
Patients with photic symptoms due to iris defects complain of:
- Glare,
- Haloes in bright light conditions,
- Diplopia, and
- Trouble reading
Patients with mydriatic pupils report:
- Glare at night and
- Inability to focus at near
Patients should be evaluated for any previous history of:
- Ocular trauma,
- History of uveitis,
- Surgical history,
- History of benign prostate hypertrophy
Indications of iris repair:
Indications for iris surgeries can be divided into thesefive main categories:
1. Functional or optical indications:
Iris defects leading to diplopia should be repaired. Iris defects leading to photic symptoms like glare, haloes around light, near vision problems etc, can be considered for surgical intervention.
2. To provide structural support for lens implantation:
Pupilloplasty and Iridodialysis repair can be performed to provide the necessary support required for iris claw lens implantation as an option if there was no adequate capsular support to implant in-bag or sulcus IOL.
3. To prevent post-operative complications, as in penetrating keratoplasty
In cases of floppy iris that are expected to adhere to the peripheral edge of a corneal graft, pupilloplasty is performed to tighten the iris to prevent it from causing peripheral anterior synechiae (PAS) that would increase the risk of angle closure and graft rejection.
4. To relieve PAS (peripheral anterior synechiae) or appositional angle closure
Pupilllplasty is used to break peripheral anterior synechiae and angle apposition in primary and secondary angle closure glaucoma like post trauma, plateau iris syndrome, Urrets-Zavalia syndrome, secondary to long standing silicone oil in the anterior chamber etc.
5. To provide more cosmetically acceptable pupil
Pupilloplasty is very rarely performed only for cosmesis, but it can be done, especially in large colobomas in a coloured iris where it can provide functional and cosmetic repair.
Contraindications
These are relative contraindications:
-
In a phakic eye with a clear crystalline lens due to the possibility of lens touch and cataract formation.
-
In a case with atrophic iris due to the possibility of increased iris damage.
Surgical Management
Pre-operative Planning:
The repair of iris defects can be challenging, therefore, creating a favourable environment within the anterior chamber will ensure success.
Following are tips that can help facilitate success and avoid complications:
- Repair should be conducted in aphakic or pseudophakic eyes, as the risk of anterior capsular tear and subsequent cataract formation is high in phakic eyes.
- It is recommended to block the eye, either via a peribulbar or retrobulbar block.
- Instillation of miotic agent at the start of the surgery stretches and increases the surface area.
- Centripetal mechanical pulling of the iris helps to loosen and stretch the tissue in preparation for suturing.
- Ensure there is ample viscoelastic in anterior chamber to protect the corneal endothelium, as well as in the ciliary sulcus to slightly tent up the iris for an easier pass of the suture. Using an anterior chamber maintainer or pars plana infusion in vitrectomized eyes is beneficial.
- Docking the needle into a 25-gauge cannula as the needle enters and exits the anterior chamber can help to prevent an inadvertent pass through the Descemet’s membrane.
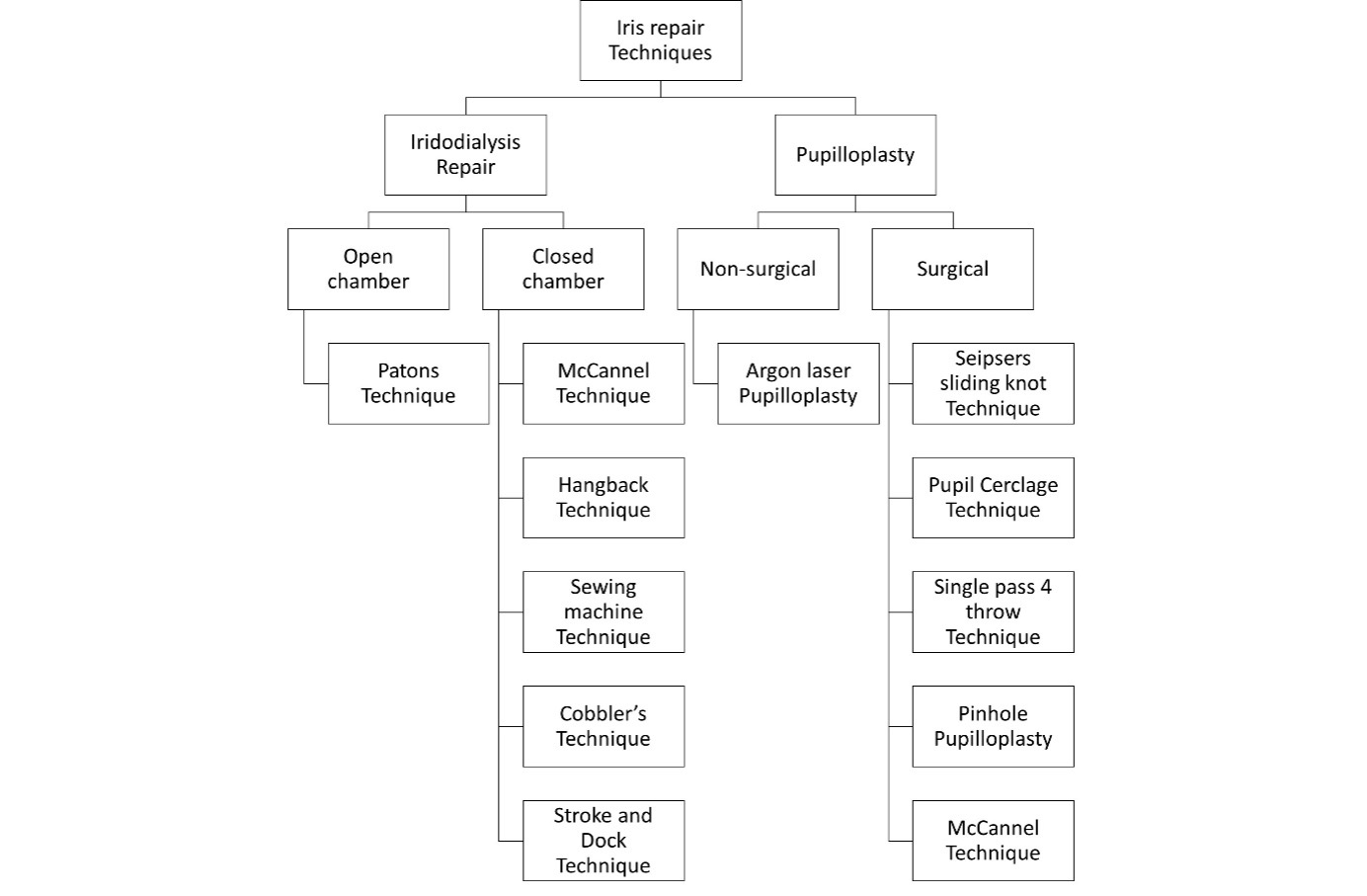
Types of Iris Repair Surgeries
-
- Iris root surgeries/ Iridodialysis repair
- Pupilloplasty
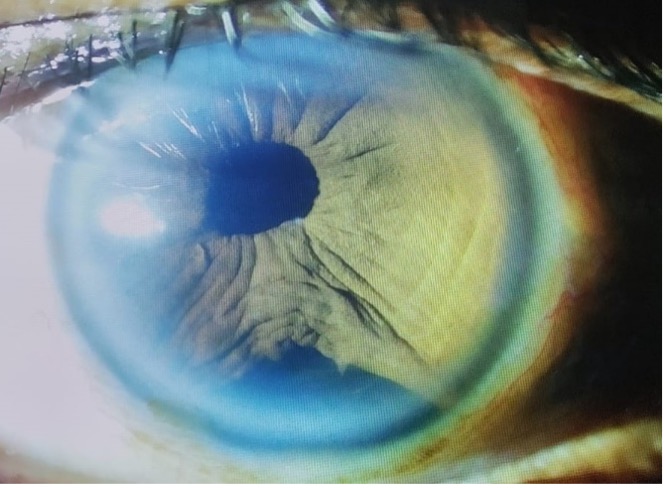
A. Iridodialysis
Iridodialysis, also known as coredialysis is tearing away of iris from its attachment to ciliary body. It occurs when, secondary to blunt trauma, there is sudden acceleration or deceleration in the eye, leading to a hydraulic shock wave. This shock wave traveling in the closed sphere transfers force to the contrecoup region to detach the iris at its insertion to the ciliary body i.e the iris root.
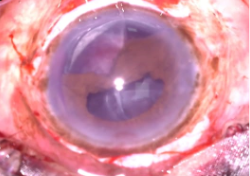
Techniques of Iridodialysis Repair:
Open chamber technique
Paton’s technique of ID repair: Paton in 1973, first described this technique. It is obsolete now and only its historic value remains.
Closed chamber techniques of ID repair:
- McCannel technique
- Hangback technique
- Sewing machine technique
- Cobbler technique
- Stroke and dock technique
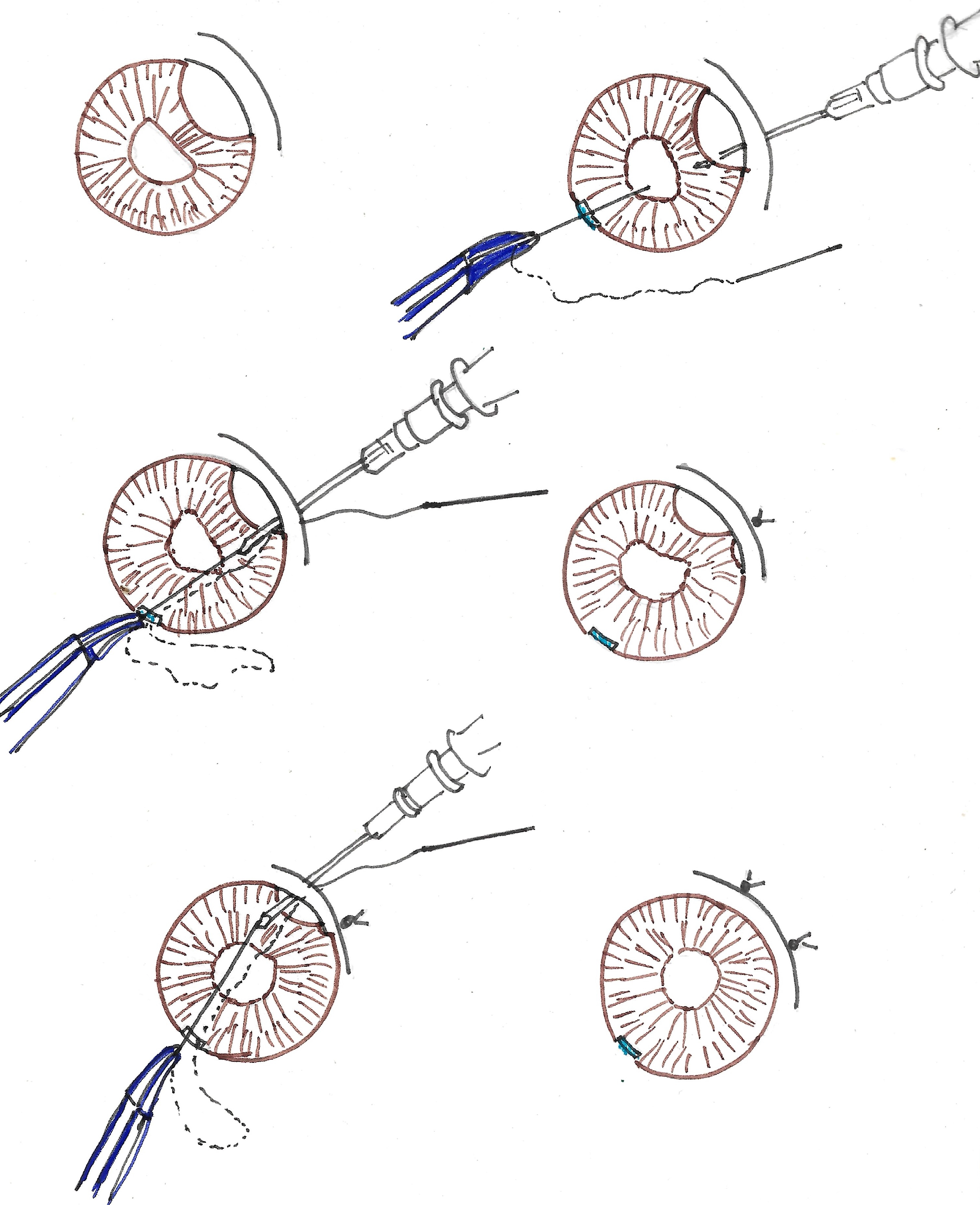
McCannel technique of ID repair:
The double-armed McCannell suture method begins with one needle entering the anterior chamber through the limbus inferiorly. It then pierces the iris base and leaves the chamber angle and sclera. A second needle is utilized in a similar fashion, entering from the same incision, but rather piercing the iris adjacent to the previous iris base site. The suture is then tied over the sclera and buried
Hangback technique of ID repair:
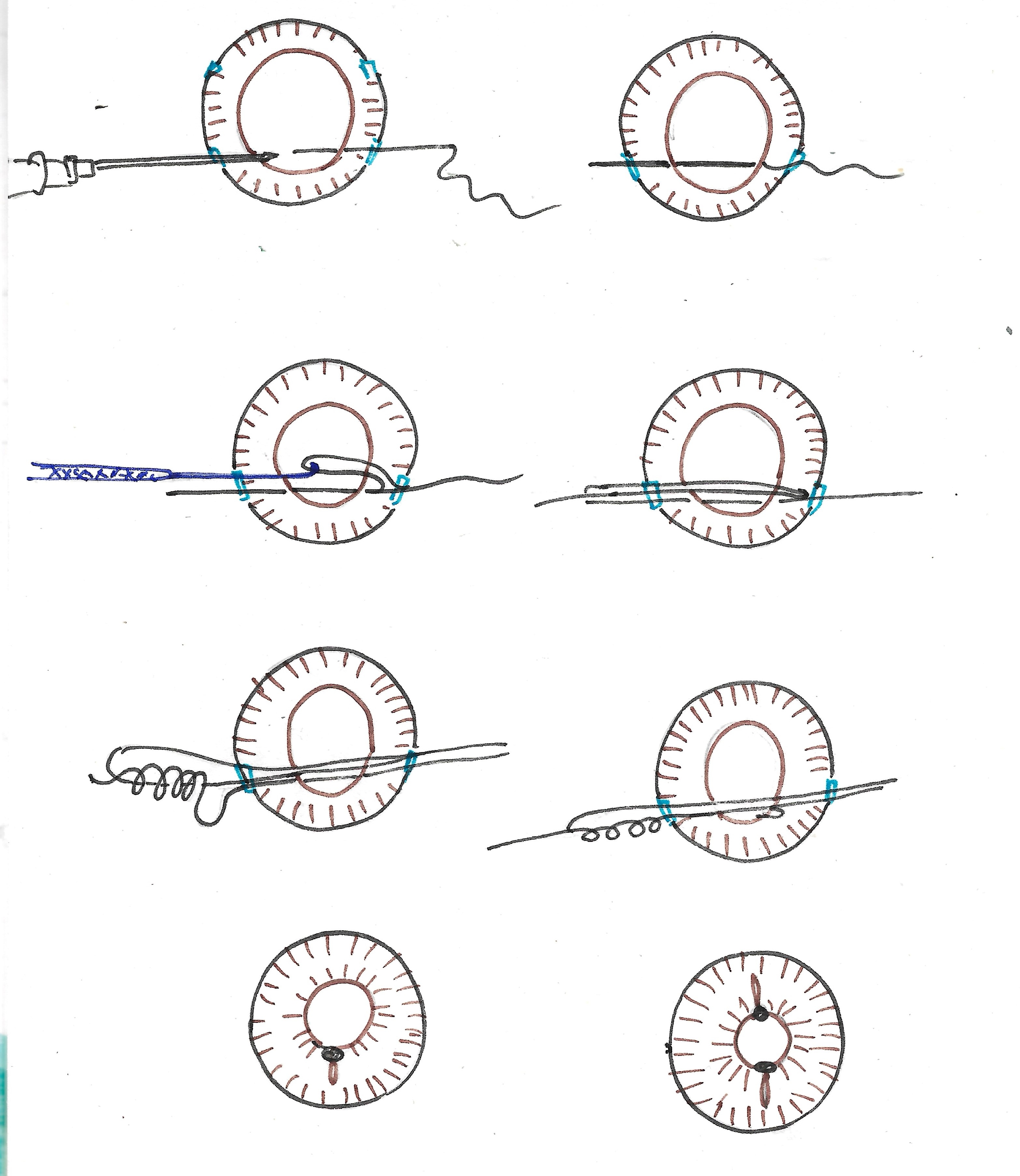
Works best for the repair of ID of 3 o’clock hours or less. A partial thickness scleral tunnel is made parallel to iridodialysis. The side port is created about 3-4 clock hours away from the dialysis. The detached peripheral iris is suspended by 10-0 polypropylene suture inside normal iris insertion. The knot lies in anterior chamber.
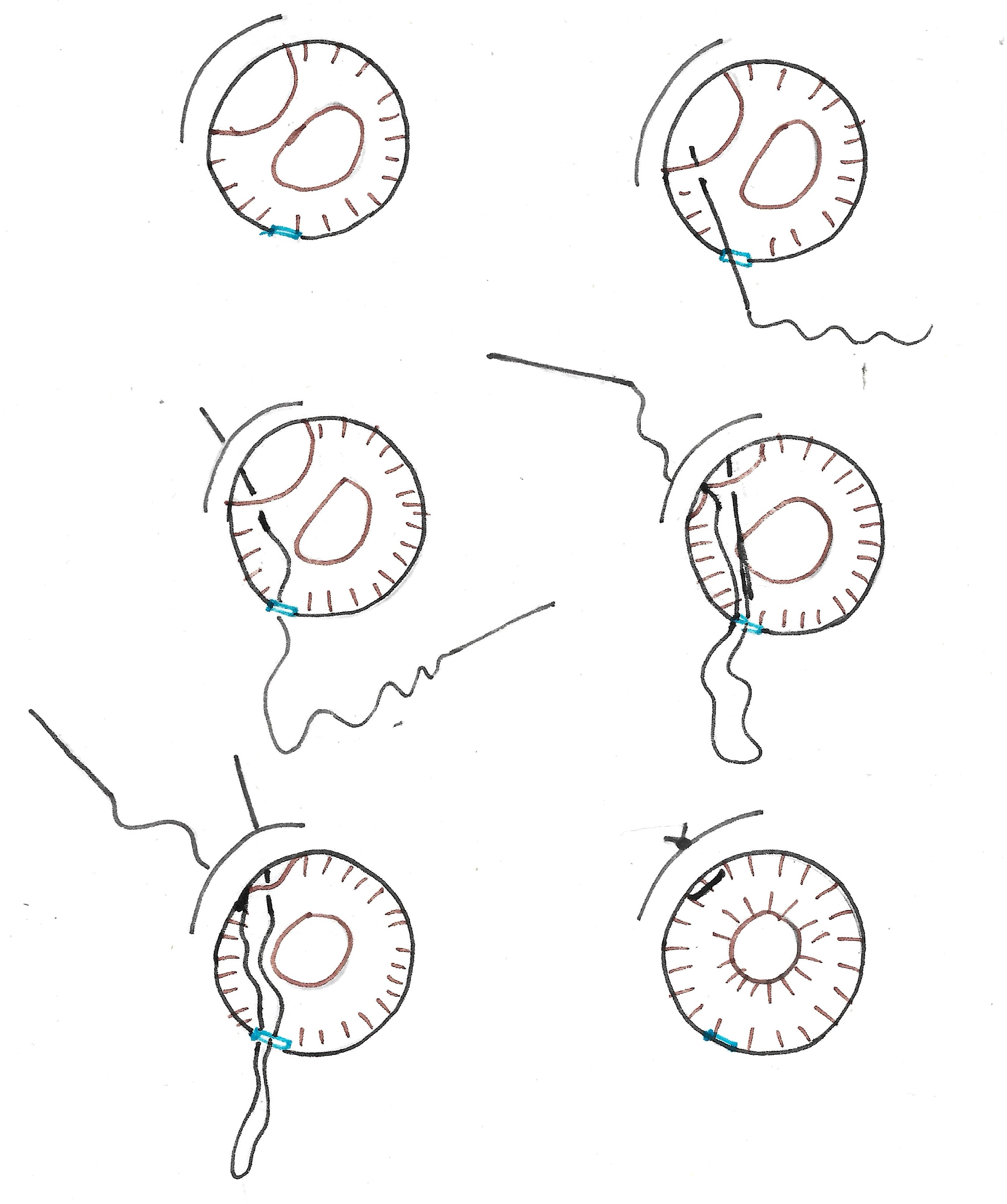
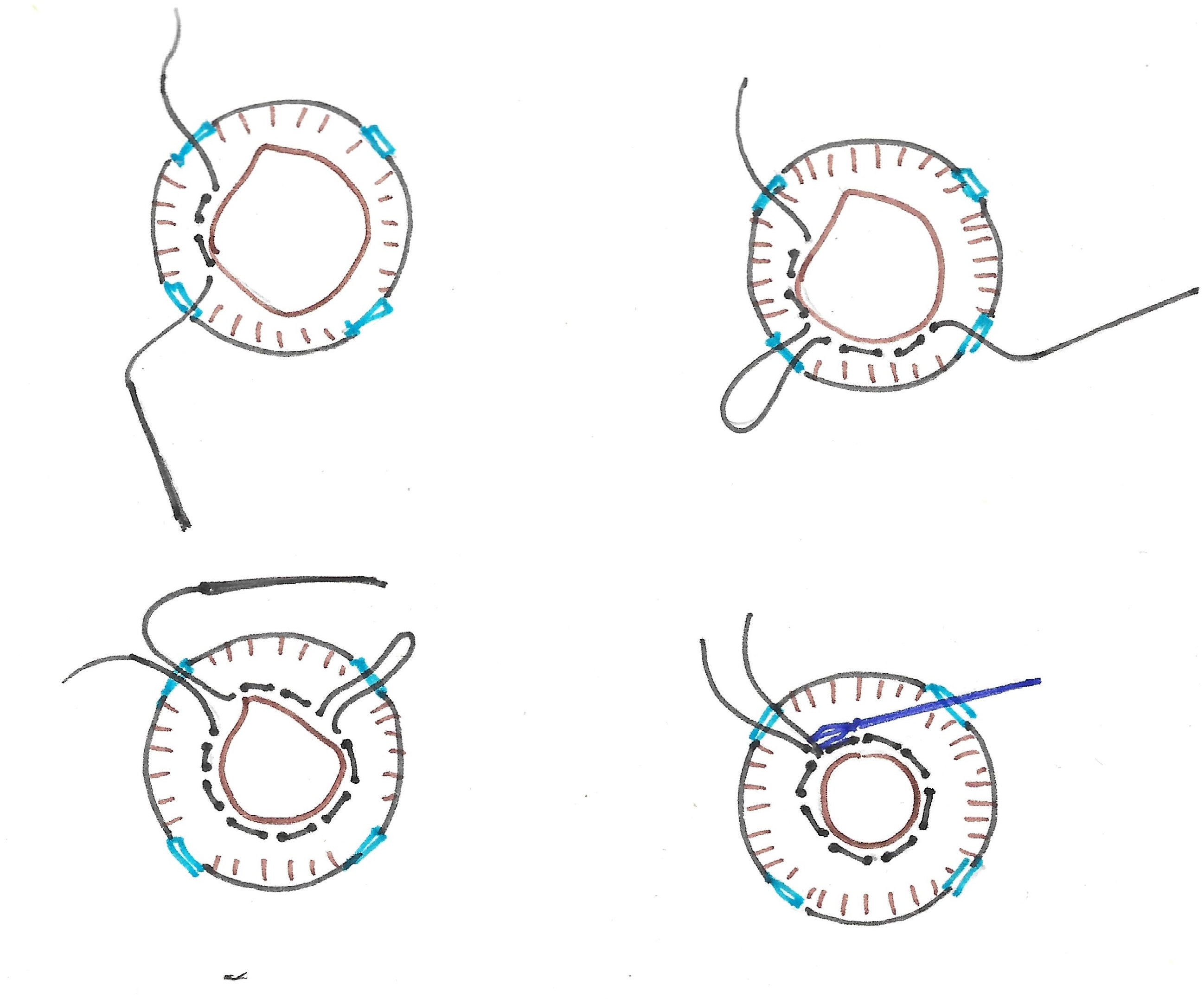
Sewing machine technique of Iridodialysis repair (SMT):
10-0 suture is threaded into 26G inch long hypodermic needle. The scleral tunnel is made parallel to the iridodialysis. Side port is created opposite to the dialysis. The 26-gauge needle with suture is passed through the paracentesis and the scleral groove engaging the root of the iris. The free end of the polypropylene suture is pulled out through the scleral tunnel. Suture loop is created by withdrawing the needle in the AC with assistant holding on to the exteriorised suture. The same process is repeated to create multiple loops. Suture loops are then cut and adjacent ends are then tied. The knots are buried into the scleral tunnel and conjunctiva is closed.
Cobbler technique of Iridodialysis repair:
A partial-thickness scleral tunnel is created parallel to the limbus along the extent of the iridodialysis. A limbal paracentesis is created at the 2 O’clock position. The 26-gauge needle with suture is passed through the paracentesis and the scleral groove engaging the root of the iris. The free end of the suture is pulled out. The needle is withdrawn into the AC and taken out engaging the root of the iris again. The suture is pulled out forming a loop through which the free end of the suture is passed to lock the loop. This step is repeated multiple times until multiple loops are laid over the scleral bed.
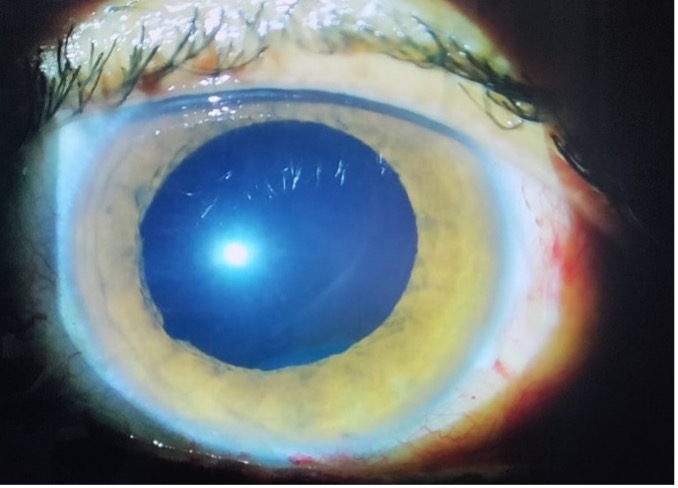
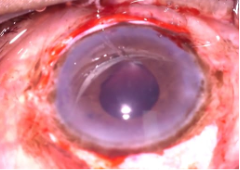
B. Pupilloplasty
Iris sphincter tears may occur after blunt ocular trauma and can result in persistent mydriasis. Iris sphincter tear occurs secondary to anteroposterior compression of the globe following blunt trauma. This compression leads to equatorial expansion and sudden displacement of aqueous within the anterior chamber. The aqueous forcefully rushes through the path of least resistance i.e., the pupillary orifice, to dissipate the tension created in the anterior chamber, causing forced pupillary dilatation. At the same time, there is reflex constriction of pupillary sphincter inducing shearing forces in the sphincter pupillae. When the sphincter elasticity reaches its limit, the weakest areas rupture causing mydriasis.
Techniques
These can be divided into non-surgical and surgical methods:
Non-surgical methods:
Argon laser pupilloplasty:
It is done to adjust the position of an eccentric pupil, or to change the size of miotic pupil.
In cases of eccentric pupil, the procedure is performed by applying laser spots to the mid-peripheral iris in sectoral fashion to pull the pupil in a particular direction aiming for re-centration, used specially in cases of multifocal IOLs.
In case of a miosed pupil, laser spots are applied circumferentially in multiple rows that causes contraction of the iris tissue pulling the pupilllary margin toward the periphery, thus dilating the pupil. Mainly performed in cases of miosed pupil with implanted multifocal IOL, as miosis obstructs light from reaching the rings of multifocal IOL resulting in functional disruption of multifocality and deteriorating the visual quality
Parameters - Initial placement of 3600 contiguous, concentric, small concentration argon laser burns (200 micrometres, 0.2 seconds exposure and 200-400mV power) just adjacent to the pupillary margin.
Argon laser pupilloplasty can be used in combination with procedures such as Argon Laser peripheral iridoplasty to relieve the pupillary block when the pupillary sphincter cramps. Linear cuts are made across the iris fibres. Argon laser burns are delivered through an Abraham iridectomy lens. Intrinsic iris tension then causes the linear cuts to spread apart. This allows enlargement, or repositioning of the pupil with minimal burn energies and a high percentage of success.
Surgical methods:
- Siepser sliding knot technique
- Pupil cerclage technique
- Single-pass four-throw technique (SFT)
- Pinhole pupilloplasty
- McCannel technique
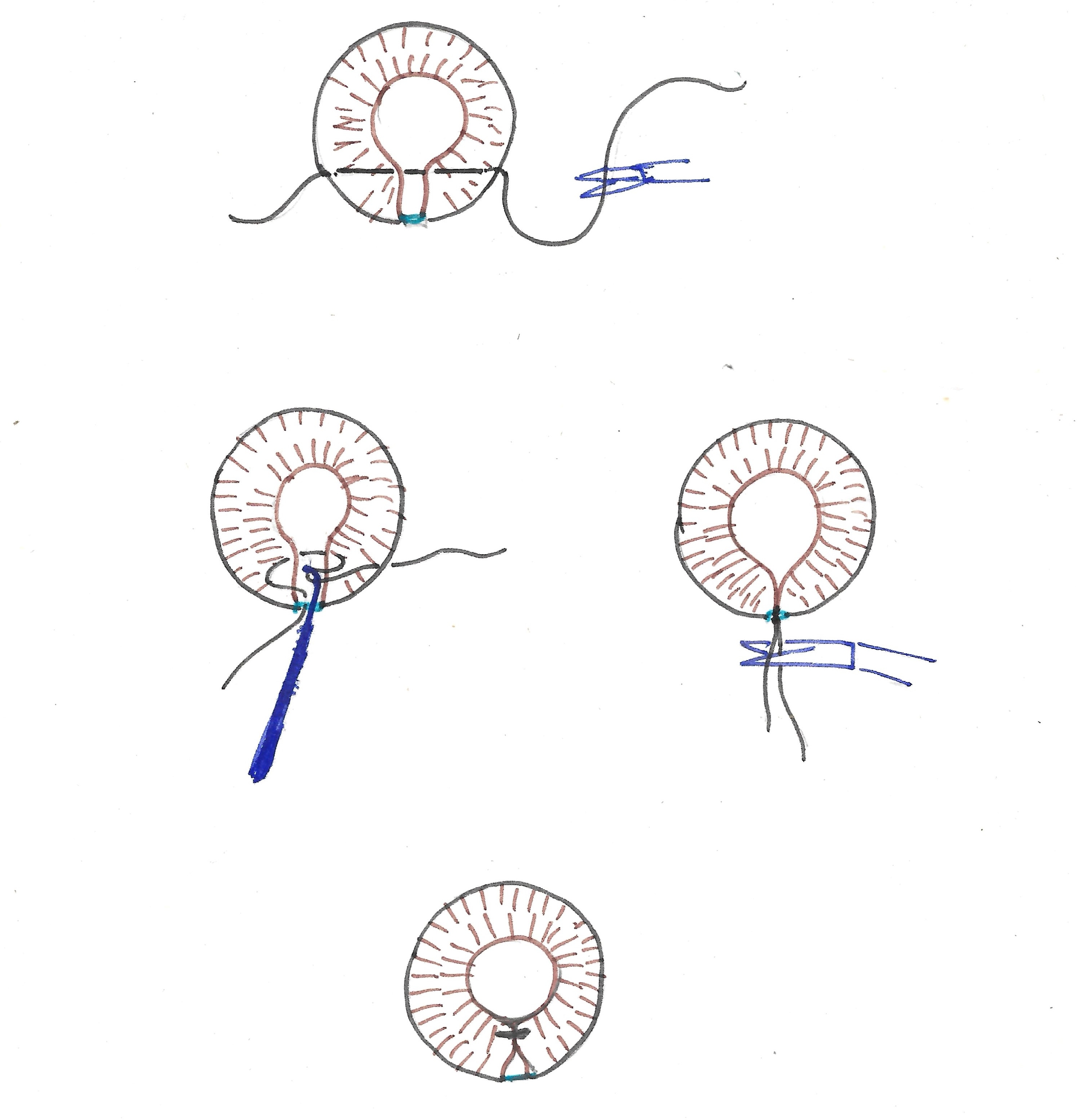
Siepser sliding knot technique:
This sliding knot technique allows sutures to be tied within the eye without impairing uveal tissue thus keeping a well-maintained anterior chamber during the process. The aim is to minimise corneal damage by decreasing the number of incisions and reducing the manipulation exerted on the delicate iris tissue.
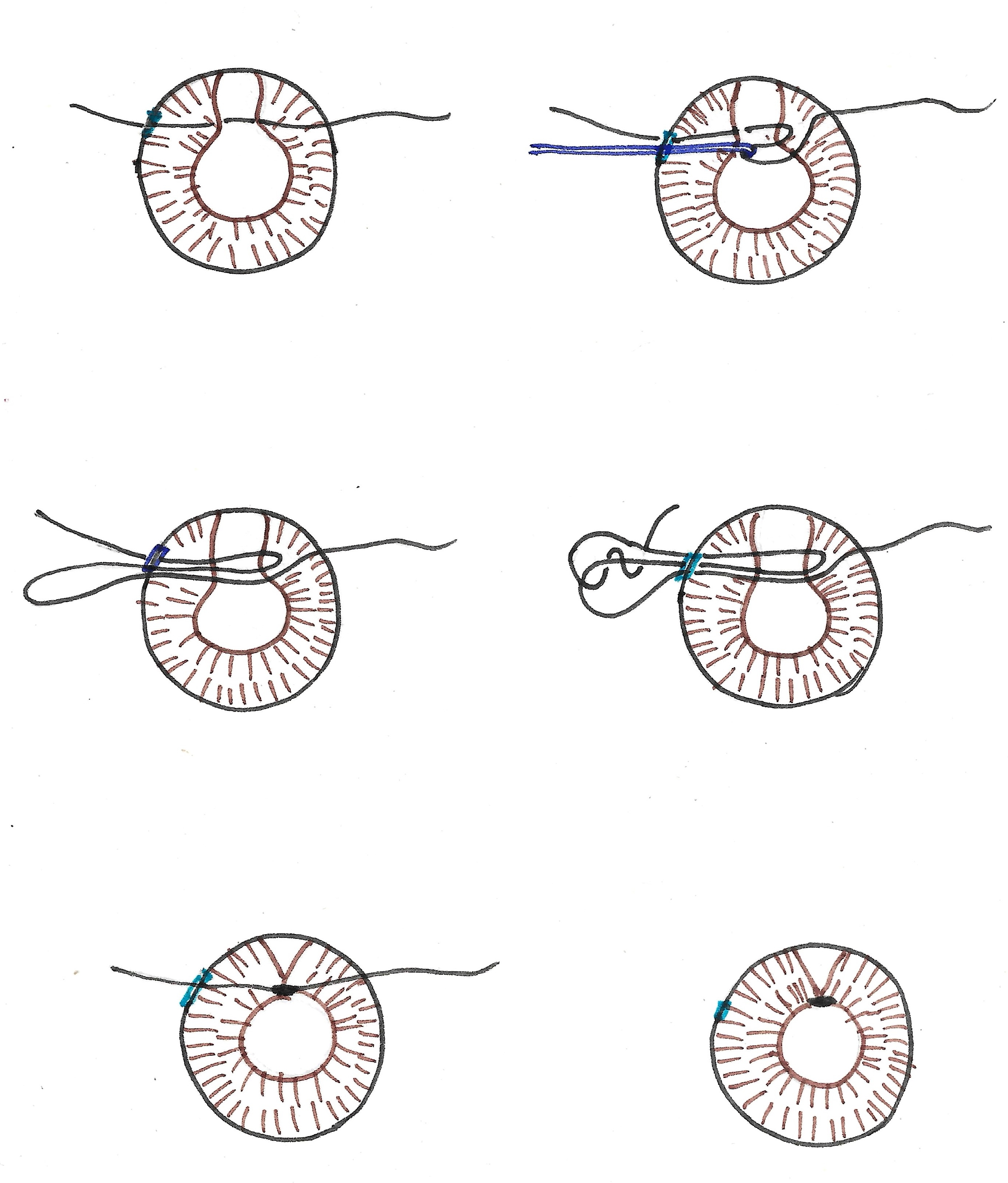
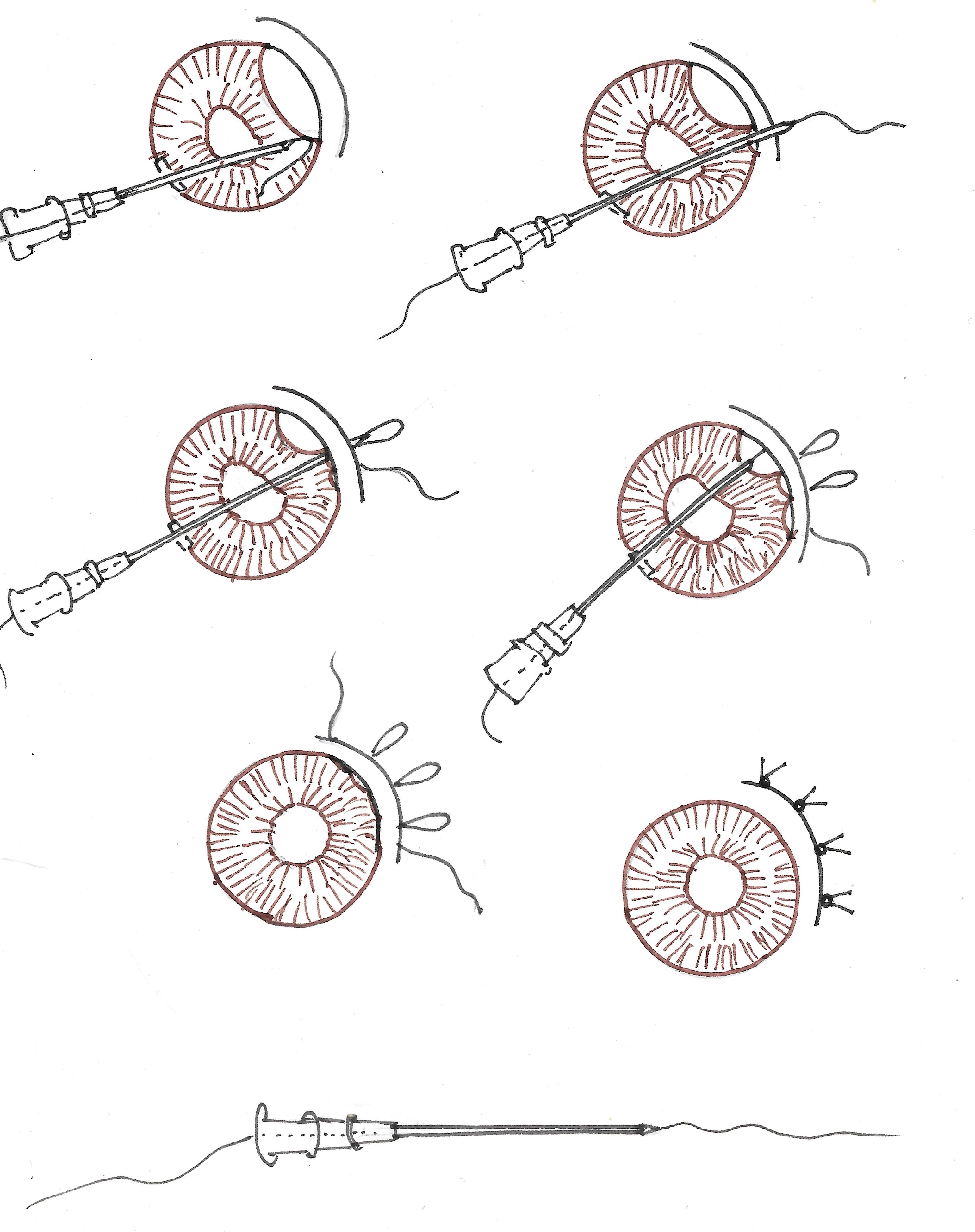
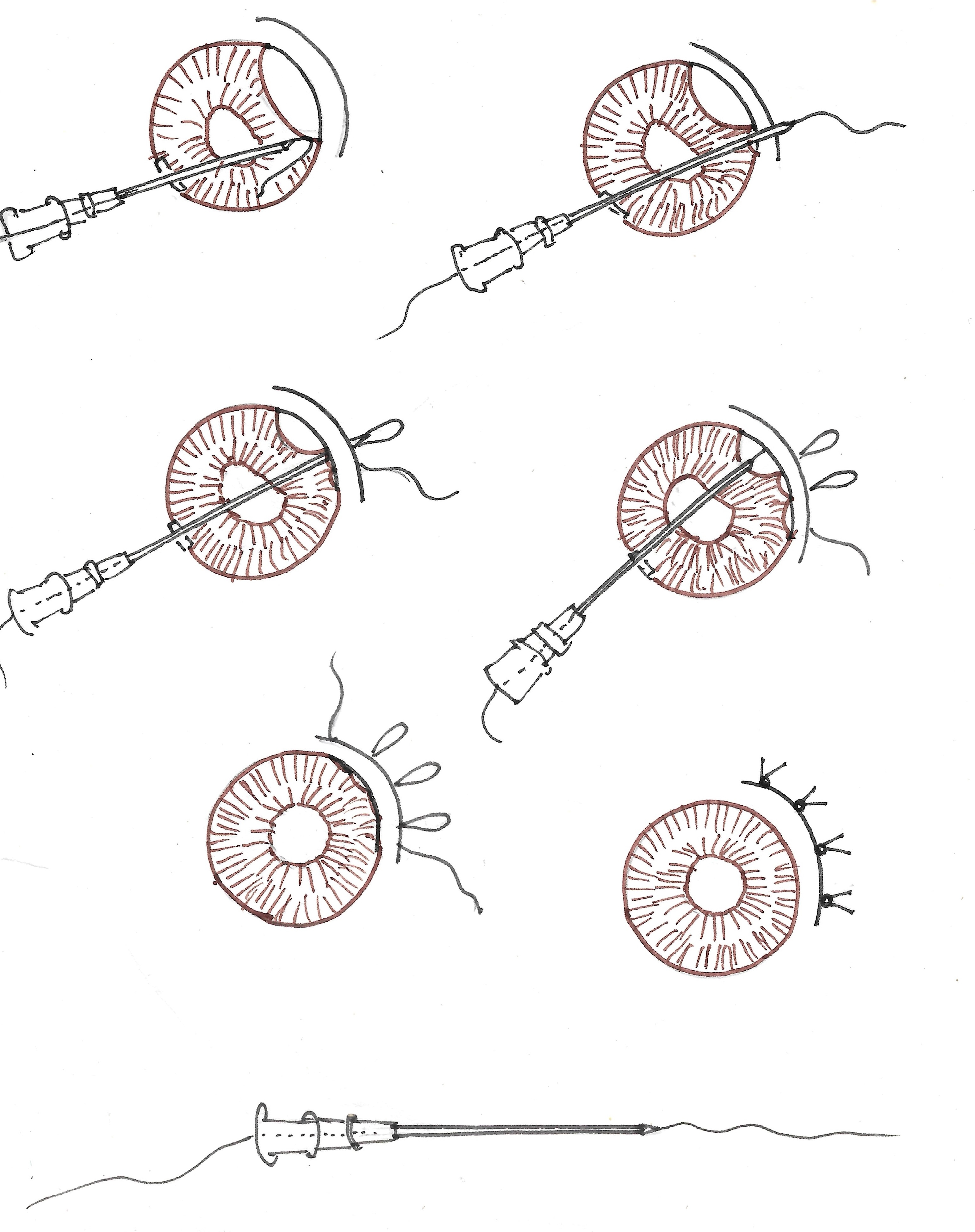
2. Pupil cerclage technique
Paracentesis is created at 2, 5, 7 and 10 o clock position. The pupil cerclage technique re-establishes the pupil with a precise regulation of the pupil size without distortion of its natural round shape. The sliding knot allows surgeon to lessen the risk of iatrogenic iris damage and to make a secure permanent knot.
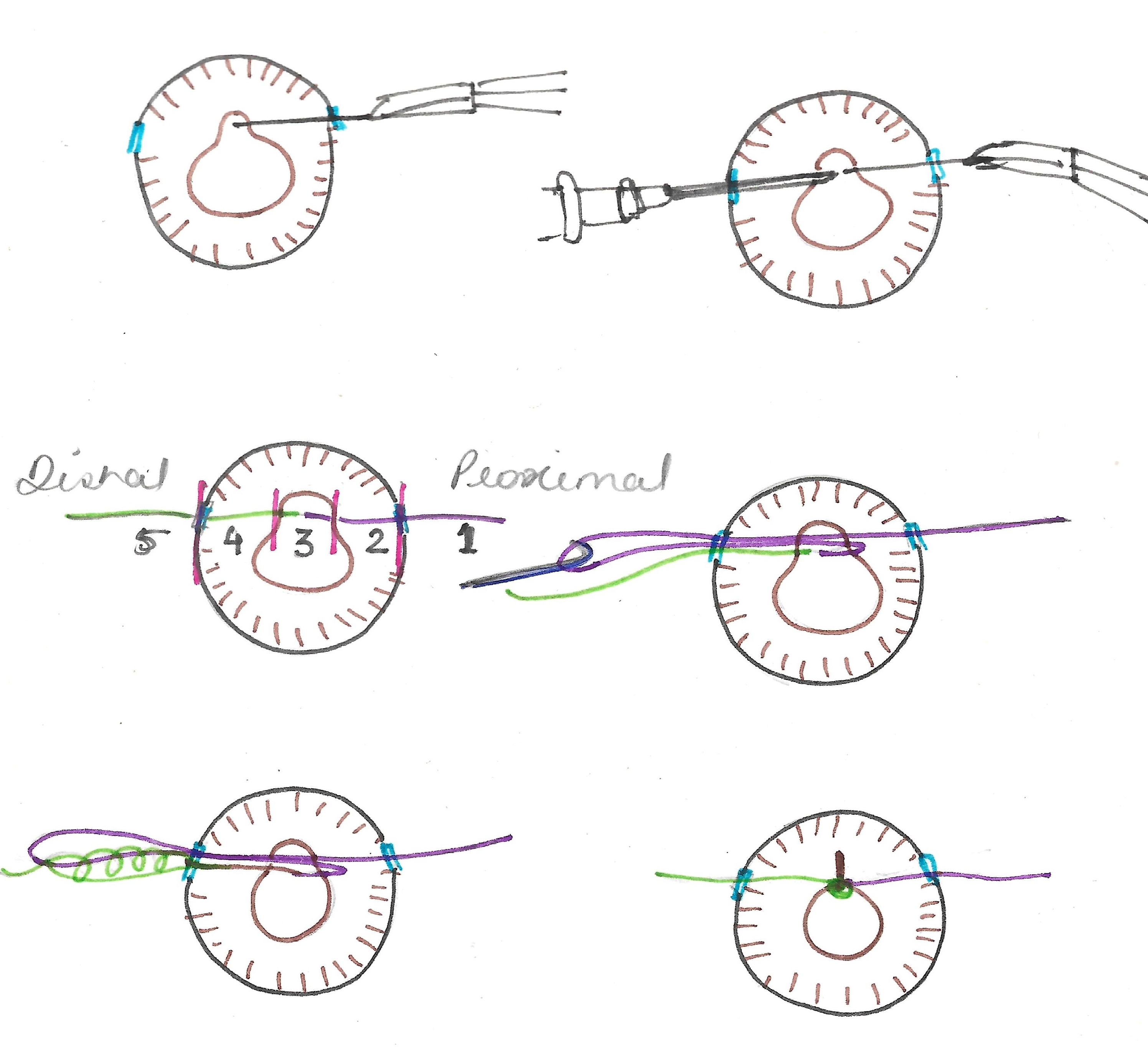
3. Single-pass four-throw technique (SFT)
This method is regarded as the simplest form of surgical pupilloplasty, with a short learning curve. The suture end is passed through the loop with 4 throws, creating a helical configuration, making the knot strong and durable.
4. Pinhole pupilloplasty
The aim is to achieve a smaller (pinhole) pupillary aperture (of approximately 1.3 mm in diameter), based on the fact, that obtaining a pinhole-sized pupil will filter the stray light from the periphery of the cornea in cases with high-order corneal aberrations. The pinhole effect blocks distorted and unfocused light rays and isolates more focused central and paracentral rays through the central aperture, in a way reducing aberrations of the optical system as a whole. It also increases the depth of focus enhancing visual acuity and its image quality both for near and far.
5.McCannel technique
In this technique, 10-0 polypropylene suture is passed through two paracenteses, which has been created perpendicular to the edge of an iris defect. A full thickness stab incision is created between the paracenteses through the peripheral cornea. A hook is introduced through the stab incision and is used to bring both ends of the suture out of the eye where it is then tied pulling the pupillary edges together to close the defect.
5. Stroke and Dock Technique
A partial thickness scleral flap is made parallel to the Iridodialysis. The 9-0 polypropylene needle is used for stroking and entering the peripheral iris, and the 26-gauge needle is used for docking the suture needle, thus the name of this technique. For large Iridodialysis, multiple sutures are required, and multiple entries are made through the anterior chamber, potentially increasing the chances of injury to endothelium and lens.
To summarise, there are many techniques of iris repair described in literature, with new modifications happening every day. Choice of surgery depends on the site of injury, the amount of damage and of course the skills of the surgeon.
References:
- Pandya M, Shah A. Iridodialysis repair using double-armed McCannell suture. J Case Rep Images Opthalmol2019;2:100013Z17MP2019
- Ravi Kumar KV. Modified sewing machine technique for Iridodialysis repair, intraocular lens relocation, iris coloboma repair, Cionni ring fixation, and scleral-fixated intraocular lens. Indian J Ophthalmol. 2018 Aug;66(8):1169-1176. doi: 10.4103/ijo.IJO_1320_17. PMID: 30038167; PMCID: PMC6080449.
- Pandav SS, Gupta PC, Singh RR, Das K, Kaushik S, Raj S, Ram J. Cobbler's Technique for Iridodialysis Repair. Middle East Afr J Ophthalmol. 2016 Jan-Mar;23(1):142-4. doi: 10.4103/0974-9233.171770. PMID: 26957855; PMCID: PMC4759894.
- Dağlioğlu MC, Coşkun M, Ilhan N, Ayintap E, Tuzcu EA, Ilhan O, Oksüz H. Repair of Iridodialysis using 8-0 polypropylene. Semin Ophthalmol. 2014 May;29(3):159-62. doi: 10.3109/08820538.2013.796395. Epub 2013 Jul 23. PMID: 23879224.
- Snyder ME, Lindsell LB. Nonappositional repair of Iridodialysis. J Cataract Refract Surg. 2011 Apr;37(4):625-8. doi: 10.1016/j.jcrs.2011.02.001. PMID: 21420584.
- Kusaka M, Miyamoto N, Akimoto M. Repairing Iridodialysis by riveting with a double-flanged polypropylene suture. J Cataract Refract Surg. 2019 Nov;45(11):1531-1534. doi: 10.1016/j.jcrs.2019.08.001. Epub 2019 Oct 1. PMID: 31585854.
- Kaufman SC, Insler MS. Surgical repair of a traumatic Iridodialysis. Ophthalmic Surg Lasers. 1996 Nov;27(11):963-6. PMID: 8938808.
- Lian RR, Siepser SB, Afshari NA. Iris reconstruction suturing techniques. Curr Opin Ophthalmol. 2020 Jan;31(1):43-49. doi: 10.1097/ICU.0000000000000628. PMID: 31770162
- Alpar JJ. The use of Healon in McCannel suturing procedures. Trans Ophthalmol Soc U K (1962). 1985;104 ( Pt 5):558-62. PMID: 3901433
- Osher RH, Snyder ME, Cionni RJ. Modification of the Siepser slip-knot technique. J Cataract Refract Surg. 2005 Jun;31(6):1098-100. doi: 10.1016/j.jcrs.2004.11.038. PMID: 16039481.
- ÖZDEK Ş, ÖZMEN MC. A simple surgical technique for repair of Iridodialysis. Turkish Journal of Medical Sciences. 2009;39(2):317-9.
- Khokhar S, Gupta S, Kumar G. Iridodialysis repair: stroke and dock technique. International ophthalmology. 2014 Apr;34:331-5.
- Safran SG. Sewing machine style technique for Iridodialysis Repair. Ocular Surgery News. 1995 May 1;49.
- Wachler BB, Krueger RR. Double-armed McCannell suture for repair of traumatic Iridodialysis. American journal of ophthalmology. 1996;1(122):109-10.
- Erakgun T, Kaskaloglu M, Kayikcioglu O. A simple closed chamber technique for repair of traumatic Iridodialysis in phakic eyes. Ophthalmic Surgery, Lasers and Imaging Retina. 2001 Jan 1;32(1):83-5.
- Key BW. Concerning Iridodialysis as a clinical entity, its surgical treatment: Report of cases. Transactions of the American Ophthalmological Society. 1933;31:93.

