Papilledema is a term used to define optic disc edema. However, it is specifically used for non-inflammatory, often bilateral, passive edema of the optic nerve head secondary to raised intracranial tension. The cause for raised intracranial pressure can be space-occupying lesions, meningitis, or idiopathic intracranial hypertension. The disc swelling results due to axoplasmic stasis and intracellular fluid accumulation. Ophthalmoscopically, the disc appears elevated, and hyperemic, with blurred margins. The ophthalmoscopic signs of papilledema include mechanical and vascular signs [Table 1].
|
Mechanical signs |
Vascular signs |
|
a.Elevation of the disc surface b.Blurring of the disc margins c.Filling of the cup d. Edema and opacification of the nerve fiber layer e.Paton’s lines or retinochoroidal folds (in circumpapillary fashion) |
a.Disc hyperemia b. Congested veins c. Splinter hemorrhages in peripapillary area d. Absence of spontaneous venous pulsations e. Macular star formation at later stages |
Table 1: Ophthalmoscopic features of papilledema.
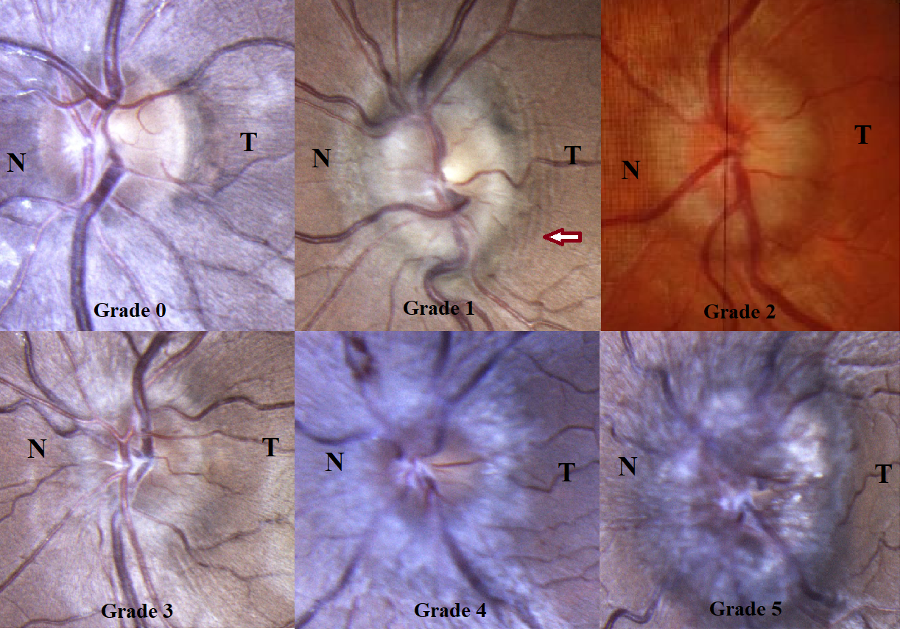
Ophthalmoscopically, Frisen grading is used to grade papilledema [Fig 1] and is shown below in Table 2[1], which was explained by Frisen way back in 1982.
|
Grade 0 |
No papilledema Increased prominence of nerve fiber layer |
|
Grade 1 |
Very early papilledema Nasal obscuration of disc margins, with halo, without elevation of the disc or opacification of the Nerve fiber layer |
|
Grade 2 |
Early papilledema Complete peripaillary halo, elevated disc, obscuration of all borders |
|
Grade 3 |
Moderate papilledema Above + obscuration of one or two segments of blood vessels over the disc |
|
Grade 4 |
Marked papilledema Above + total obscuration of a major blood vessel over the disc |
|
Grade 5 |
Severe papilledema All vessels are obscured by edema Anteriorly elevated, dome-shaped disc Cup is filled and obliterated |
Table 2: Frisen grading of papilledema.[1]
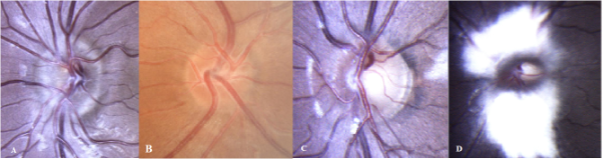
Many congenital disc conditions can mimic papilledema either due to the mechanical elevation of the disc surface or blurred margins and are termed as ‘pseudo-disc edema’. The causes for pseudo-disc edema include the following:
a.Optic disc head drusen (elevation of the disc)- most common cause of pseudo-disc edema
b.Hypermetropic small disc (mimics papilledema as the disc seems hyperemic and has a small or no cup)
c.Myopic Oblique Insertion of the Disc (MOID) or Malinserted disc (nasal margin of the disc is elevated, temporal margin is flat)
d.Myelinated nerve fibers (may simulate blurred margins and nerve fiber layer edema)
This confusion can lead to unnecessary neuroimaging and invasive CSF analysis, causing apprehension in both the patient and the treating physician. Here, we discuss clinical and ocular multimodal imaging pointers that help us differentiate the two to avoid diagnostic dilemmas.
Evaluation begins with a good history taking. In papilledema, patients often present with headaches ranging from moderate to severe and, at times, projectile vomiting. Associated symptoms include episodes of transient loss of vision, which is more on change in posture and may be associated with pulse-synchronous tinnitus. There may be associated diplopia due to lateral rectus palsy which is a false localizing sign.
Stereoscopic examination with a 78D/90D is the best way of assessing the disc and identifying spontaneous venous pulsations at the margin of the cup which are conspicuously absent in papilledema. When absent, they can be induced by gently indenting the globe whilst performing a slit lamp biomicroscopy. However, this is not a fool-proof method as 10-20% of the normal population do not have spontaneous venous pulsation.
There are some morphological presentations of the optic discs that may mimic papilledema and are referred to as pseudo- disc edema. Clinically, Pseudo disc edema is stable and non-progressive, and papilledema is progressive, if not treated. With higher grades, papilledema is more easily recognizable. Differentiating the two may cause difficulties when papilledema is just clinically detectable or is of a smaller grade. Also, around 30% of patients with idiopathic intracranial hypertension have been found to have no headaches, especially in the pediatric age group.[2] Clinically, one can differentiate true disc edema (papilledema) from pseudo-disc edema from the ophthalmoscopic features tabulated below. [Table 3]
|
True disc edema |
Pseudo disc edema |
|
|
Disc color |
Hyperemic |
Normal (Pink-orange) |
|
Peripapillary hemorrhages, hard exudates, cotton wool spots |
Common |
Absent |
|
Nerve fiber layer |
Opacified and edematous May have hemorrhages |
Transparent No hemorrhages |
|
Large vessels |
Dilated and tortuous, but normal in number |
Normal |
|
Small vessels |
Telangiectatic May be obscured in higher grades of edema |
Normal |
|
Spontaneous venous pulsation |
Absent |
Present in 80% of individuals |
|
Optic cup |
Normal initially, filled |
Small or absent |
Under circumstances of a diagnostic dilemma, multimodal imaging can be useful. The most encountered cause of pseudo disc edema is ODD, and thus, it has been extensively discussed in this paper.
Optical Coherence Tomography
OCT is a quick non-invasive go-to investigation in disc edema which can help us in quantitative and qualitative assessment. OCT helps in the following ways.
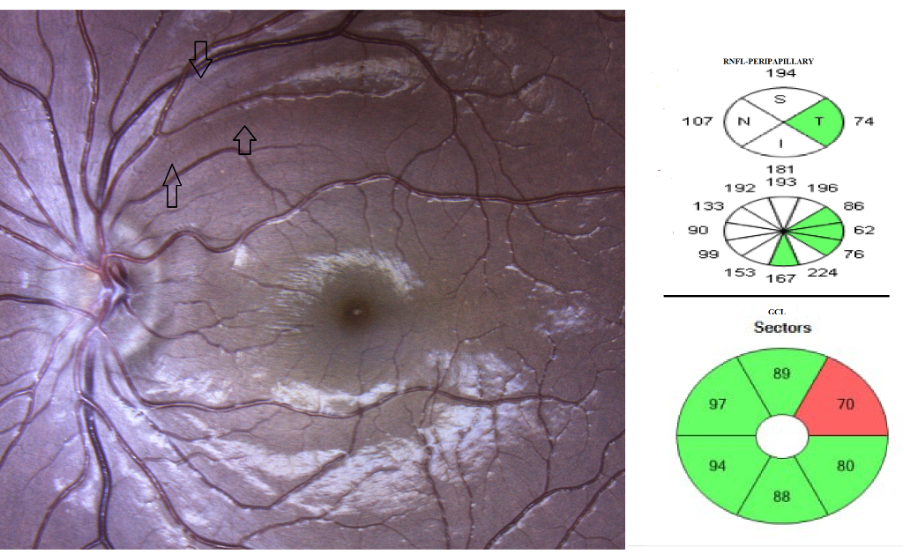
A. Assessing the peripapillary nerve fiber layer thickness (quantitative)
In true disc edema or papilledema, there is a statistically significant increased thickness in the peripapillary retinal nerve fiber layer when compared to pseudo disc edema and normal optic discs.[3,4] However, this is not the only criterion that helps to differentiate, especially when the edema is minimal or in initial stages.
B. Assessing axonal loss during follow-up (quantitative)
This is best done using a ganglion cell layer (GCL) analysis, as it can directly provide the axonal loss. GCL thickness may be normal in early papilledema and is found to decrease in chronicity. A decrease in peripapillary RNFL thickness can be due to decrease in edema or axonal loss or both. On the other hand, GCL analysis reflects the axonal loss and correlates with optic disc pallor. [4,5] As seen in the image below, there can be a GCL thinning in both papilledema and pseudopapilledema and thus cannot be used to differentiate the two.
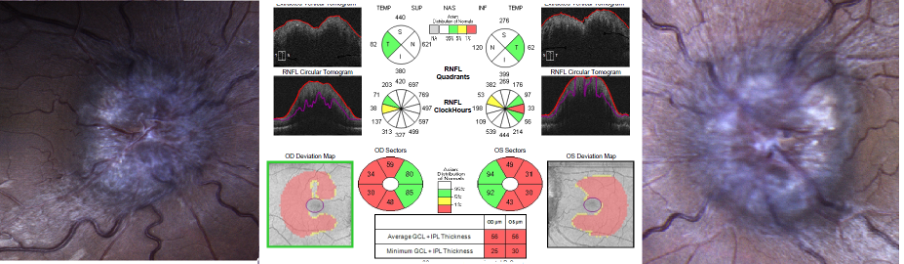
However, the limitations of quantitative OCT include absence of normative data in pediatric age group, unreliable results in myopes, increased RNFL thickness in optic disc drusen, and artifact-induced misinterpretation.[5] More important than a quantitative analysis is a qualitative analysis of the optic nerve head and can be done using a line scan.
C.Qualitative analysis
Transverse OCT scan through the optic nerve head can help us understand the morphology of the disc with respect to the Bruch’s membrane layer. Increase in intracranial pressure will lead to anterior bowing of the Bruch’s membrane layer, which has a V-shaped or flat configuration in normal population. The morphologies described in papilledema are W, S, and dome-shaped.[5] EDI-OCT (enhanced depth imaging OCT) has been found to have the highest sensitivity to detect optic disc drusen. It is seen as a hyporeflective mass with hyper-reflective borders suggestive of a buried disc drusen.
In a myopic oblique insertion of disc (MOID), that is commonly seen in myopes, the disc is inserted in a way that the nasal margin of the disc is elevated and the temporal margin is flat. This may simulate early papilledema. In eyes with high hypermetropia (>5D), the disc is usually smaller, crowded, and has minimal cupping and thus, may simulate papilledema. OCT RNFL parameters are within normal limits and thus helps to differentiate it from papilledema.[7]
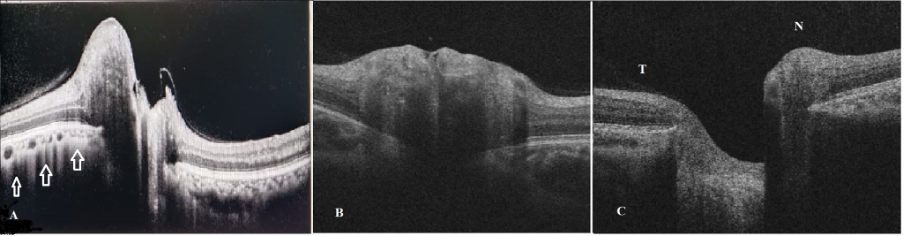
Another important qualitative feature of OCT in identifying papilledema from ODD is the presence of retinal and retino-choroidal folds and creases. They are seen on fundus imaging, and better visualized on enface OCT and include circumpapillary folds, inner retinal folds, outer retinal folds, and choroidal folds. [6] These might be seen in optic disc drusen as well.
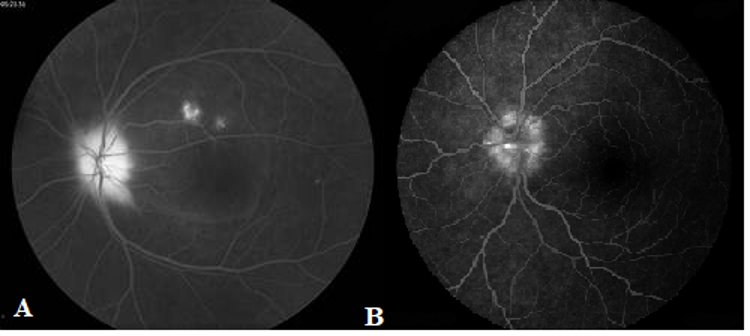
Fundus Fluorescein Angiography
FFA in disc edema involves intravenous injection of fluorescein and understanding the pattern of fluorescence of the disc. In papilledema, there is late leakage of the disc and in eyes with superficial ODD, there is early and late nodular staining of the disc, with no increase in size of the hyperfluorescence. This method has been found to have the highest accuracy in identifying true from pseudo disc edema. [8]
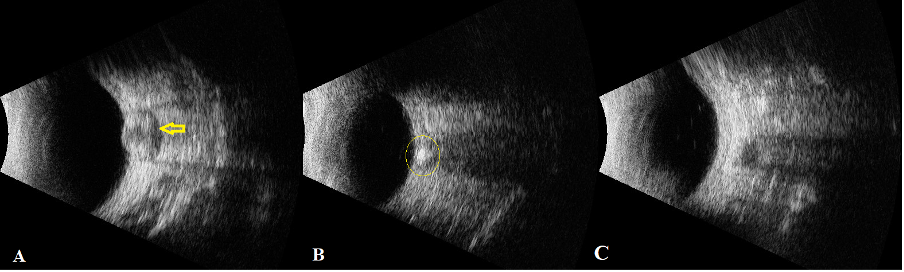
B-scan Ultrasonography
B-scan is performed using a 10MHz probe placed temporally with patient fixing in primary gaze to obtain a transverse section of the optic nerve. The optic nerve is identified as an echolucent tubular structure. It serves the purpose of differentiating papilledema from pseudo disc edema in three ways:
A. Measuring the optic nerve sheath diameter (ONSD)
It is measured at 3mm behind the globe, and any measurement more than 3.3mm can be considered suggestive of papilledema.[9] Yet another study has found a mean of 4.89 (±0.65) mm in cases with papilledema and the diameter correlated positively with the increasing grade of papilledema by Frisen grading.[10]
B. Performing the 30° test
It is performed by measuring the optic nerve sheath diameter in primary position and in 30° abduction. In papilledema, there is a 25% reduction in the ONSD due to the shifting of fluid in the abducted gaze.[11]
C. Identifying the crescent sign
The crescent sign is seen as a hypoechoic shadow within the optic nerve shadow on B-scan and is due to accumulation of fluid in the perineural space, with a sensitivity as good as 92%. [11] However, it may fail in distinguishing true disc edema from optic disc drusen as around only 55% of patients may demonstrate a hyperechoic lesion.[8] When it comes to optic disc drusen (ODD), B-scan reveals a hyperechoic shadow at the optic nerve head with posterior shadowing as shown in Fig 5B.
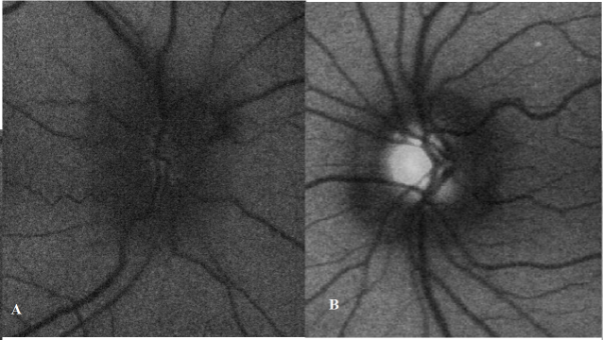
Fundus Autofluorescence
The role of fundus autofluorescence is mainly in diagnosing ODD in a rapid and non-invasive manner. The sensitivity of this test in picking up ODD is around 88% but has the highest specificity.[12] In papilledema, there is hypofluorescence of the disc that extends beyond the margins due to presence of fluid.
Visual field analysis
Visual field analysis forms an important subjective investigation in any case of neuro ophthalmology and can be performed by static or Goldmann perimetry. In papilledema, the usual defects that are increased size of blind spot, peripheral constriction of fields, and defects in the inferonasal field.[13] Around half the number of patients with optic disc drusen develop field defects like enlarged blindspot, nasal step, altitudinal defects, and bundle defects like those seen in glaucoma. [14] These may be progressive in many patients and correlates positively with the size of the drusen. It should be remembered that many patients with papilledema and pseudo disc edema may have normal visual fields. Thus, visual field analysis cannot be used as a differentiating feature between papilledema and optic disc drusen.
To summarize, differentiating papilledema from pseudo disc edema is important in clinical practice and neuroimaging with or without lumbar puncture is the gold standard for the same purpose. However, a good clinical examination aided by one or two imaging modalities explained above, can help arrive at a proper diagnosis.
References
1.Frisen L. Swelling of the optic nerve head: A staging scheme. J Neurol Neurosurg Psychiatry 1982; 45:13-18 2.Lim M, Kurian M, Penn A, Calver D, Lin JP. Visual failure without headache in idiopathic intracranial hypertension. Arch Dis Child. 2005 Feb;90(2):206-10. 3.Fard MA, Sahraiyan A, Jalili J, Hejazi M, Suwan Y, Ritch R, Subramanian PS. Optical Coherence Tomography Angiography in Papilledema Compared With Pseudopapilledema. Invest Ophthalmol Vis Sci. 2019 Jan 2;60(1):168-175. 4.Athappilly G, García-Basterra I, Machado-Miller F, Hedges TR, Mendoza-Santiesteban C, Vuong L. Ganglion Cell Complex Analysis as a Potential Indicator of Early Neuronal Loss in Idiopathic Intracranial Hypertension. Neuroophthalmology. 2018 Jun 19;43(1):10-17. 5.Nogueira PF, Caiado GC, Gracitelli PBC, Martins FM, Duarte Barros FC, De Andrade Matas SL, et al. Association between Optical Coherence Tomography Measurements and Clinical Parameters in Idiopathic Intracranial Hypertension. J of Ophthalmol. 2021, Article ID 1401609, 7 pages, 2021. 6. Sibony PA, Kupersmith MJ, Kardon RH. Optical Coherence Tomography Neuro-Toolbox for the Diagnosis and Management of Papilledema, Optic Disc Edema, and Pseudopapilledema. J Neuroophthalmol. 2021 Mar 1;41(1):77-92. 7.Wenner Y, Brauer V, Kunze K, Besgen V, Kuhli-Hattenbach C, Bertelmann T, Sekundo W. Comparison of Optic Disc Parameters in Hyperopic and Emmetropic Eyes of Healthy Children with HRT and OCT. Klin Monbl Augenheilkd. 2018 Oct;235(10):1129-1137. English. 8. Chang MY, Velez FG, Demer JL et al (2017) Accuracy of diagnostic imaging modalities for classifying pediatric eyes as papilledema versus pseudopapilledema. Ophthalmology 124(12):1839–1848. 9. Carter, S., Pistilli, M., Livingston, K. et al. The role of orbital ultrasonography in distinguishing papilledema from pseudopapilledema. Eye 28, 1425–1430 (2014). 10. Raghunandan N, Joseph M, Nithyanandam S, Karat S. Role of ultrasonographic optic nerve sheath diameter in the diagnosis and follow-up of papilledema and its correlation with Frisén’s severity grading. Indian J Ophthalmol 2019;67:1310-3 11. Bhosale A, Shah VM, Shah PK. Accuracy of crescent sign on ocular ultrasound in diagnosing papilledema. World J Methodol 2017;26:108-11. 12. Chiang J, Wong E, Whatham A, Hennessy M, Kalloniatis M, Zangerl B. The usefulness of multimodal imaging for differentiating pseudopapilledema and true swelling of the optic nerve head: a review and case series. Clin Exp Optom. 2015 Jan;98(1):12-24. 13. Wall M, George D. Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 1991;114:155-80. 14.Lee KM, Woo SJ, Hwang JM. Factors associated with visual field defects of optic disc drusen. PLoS One. 2018 Apr 30;13(4):e0196001.

