Sideport might appear as a small and trivial step in SICS but it has great significance. Improperly constructed side port will give rise to a cascade of events which will complicate the further steps. You can make an ideal side port by employing the following tips.
1. Size
Width:
A very small side port will pose a lot of problems while instrumentation. It will force multiple attempts to enlarge the side port throughout surgery, which itself poses the risk of injury to intraocular structures.
Conversely, a very big side port will lead to wound leak and instable AC intra-operatively. It may end up in needing a suture at the end.
So assessment of apt width is imperative. The size of side port is largely dependent on the gauze of simcoe cannula being used. It needs a bit of experience to adequately size the side port and after doing a few cases one will be able to judge how much the blade needs to be inserted and how much extension is required.
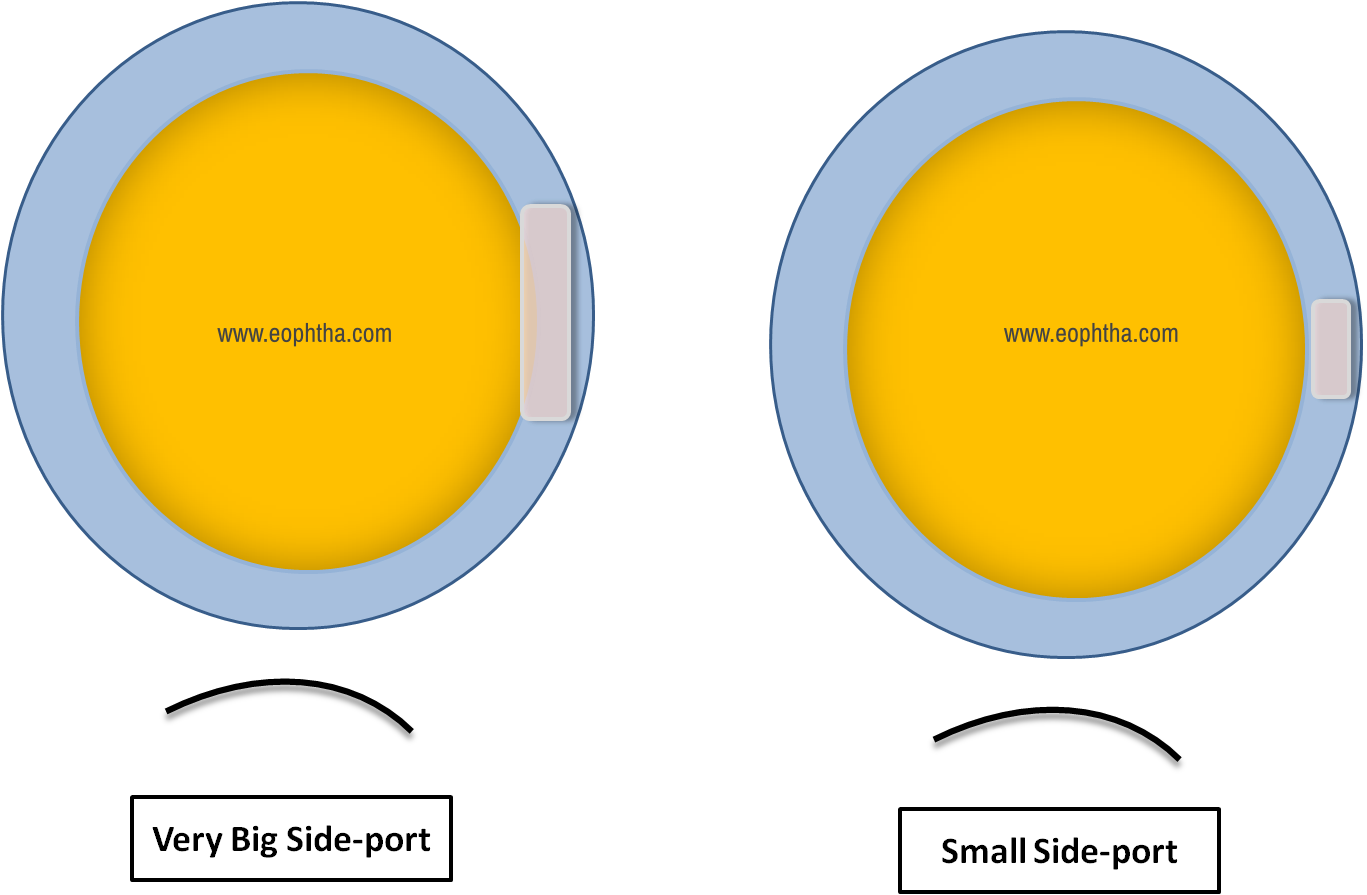
Fig 1 a. Very Big Sideport and b. Small Sideport
Thickness:
- Very thick side port poses difficulty in instrumentation and the risk of Descemet's membrane detachment increases multiple folds.
- A very thin side port is very leaky with a risk of iris prolapse, unstable AC during surgery and may pose challenges in AC formation at the end.
- Accordingly, like the role of width, thickness also plays a vital role. The thickness of the side port can be controlled by the amount of stroma pierced before entering the AC.
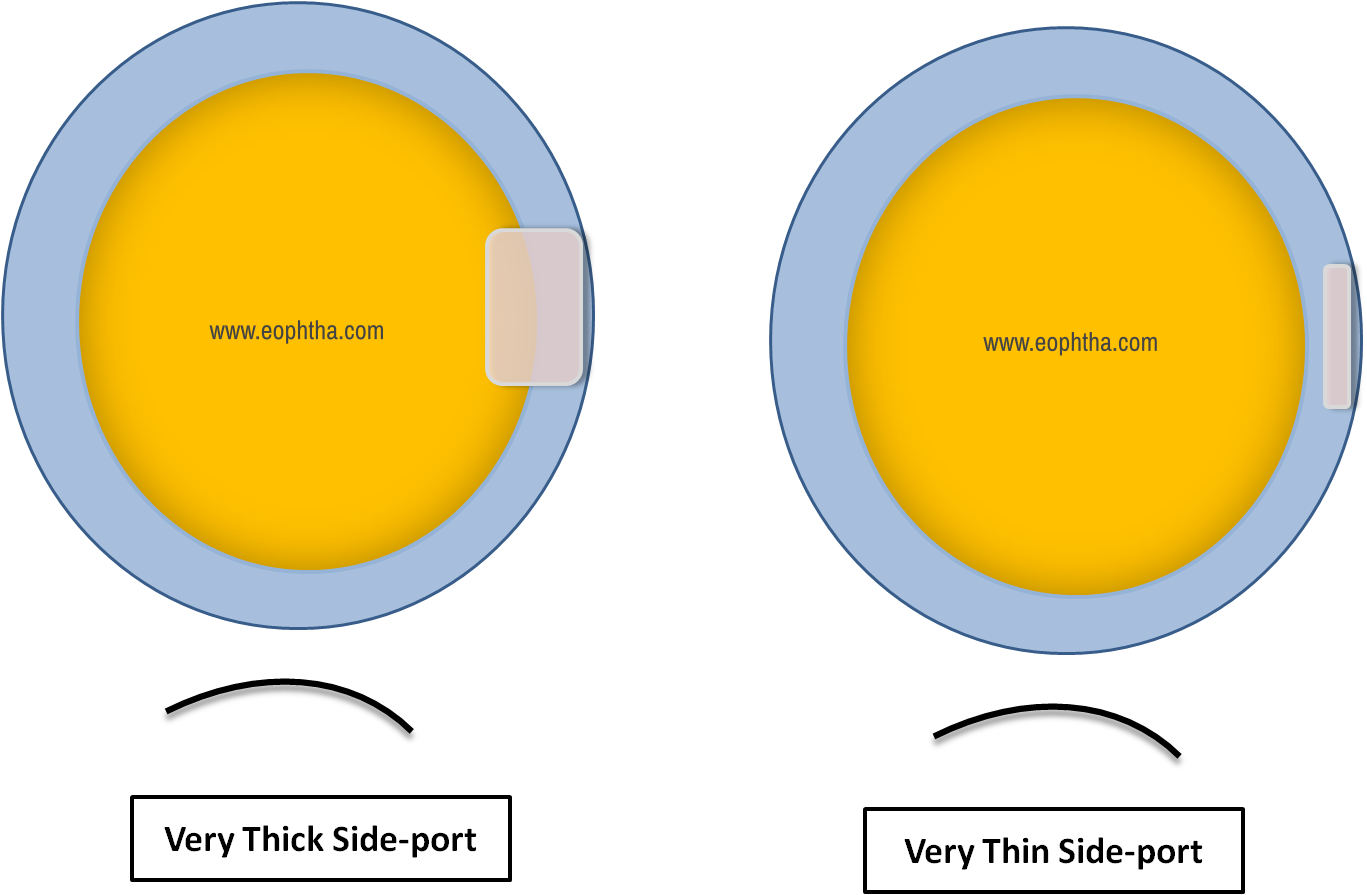
Fig 2 a. Very thick side port and b. Very thin side port
2. Site
According to clock hour:
The ideal position depends on the surgeon’s preference. I would suggest making it anywhere between 8 O’clock to 10 O'clock. The site plays a very important role as it can pose difficulty to aspirate the sub-incisional cataract. A very inferiorly placed side port will pose difficulty in rhexis construction and slightly easier cortex wash, similarly, with superiorly placed sideport it may be easier for rhexis construction but cortex wash becomes difficult.
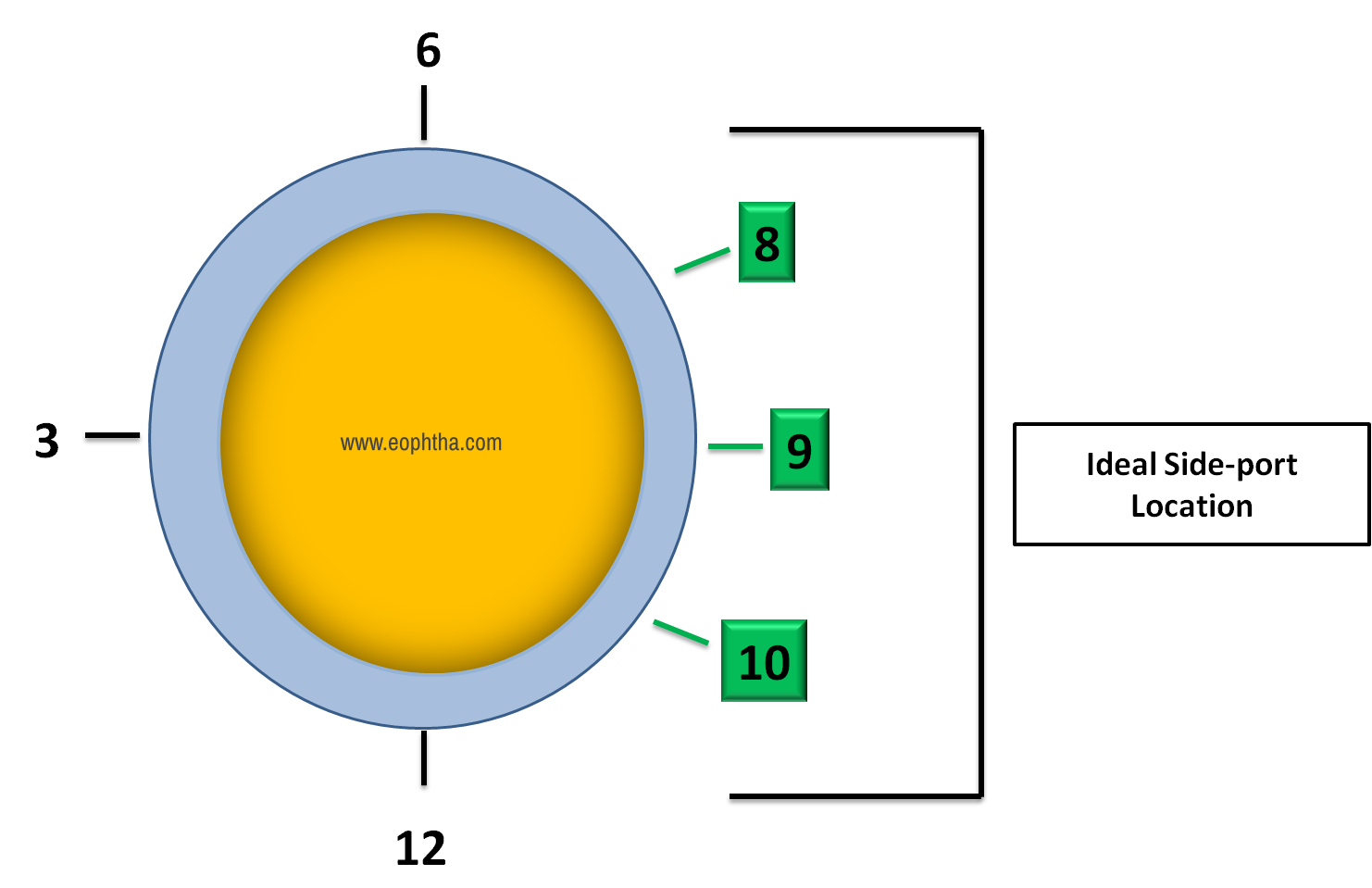
Fig 3 Ideal side port location according to clock hour
With respect to limbus:
The position of the side port in relation to the limbus also has to be taken into consideration.
It can be limbal or scleral; it would very difficult to maneuver the instrument, iris will keep prolapsing throughout the surgery, it is very difficult to form the anterior chamber with hydration at the end along with the huge risk of Descemet's detachment
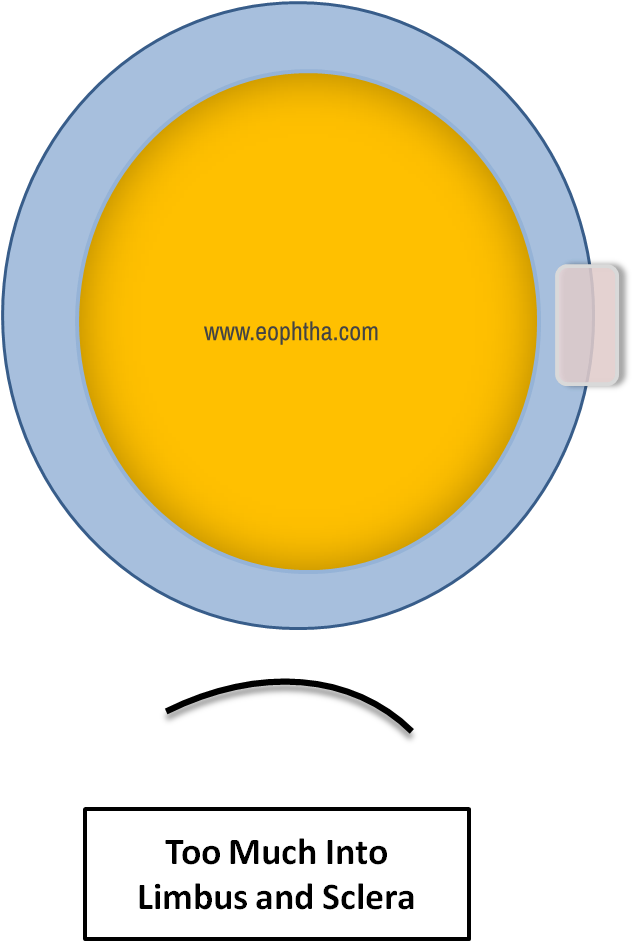
Fig 4 Sideport made too much into the Limbus or too scleral
If it is too much into the cornea; it would very difficult to maneuver the instrument and risk of Descemet's detachment
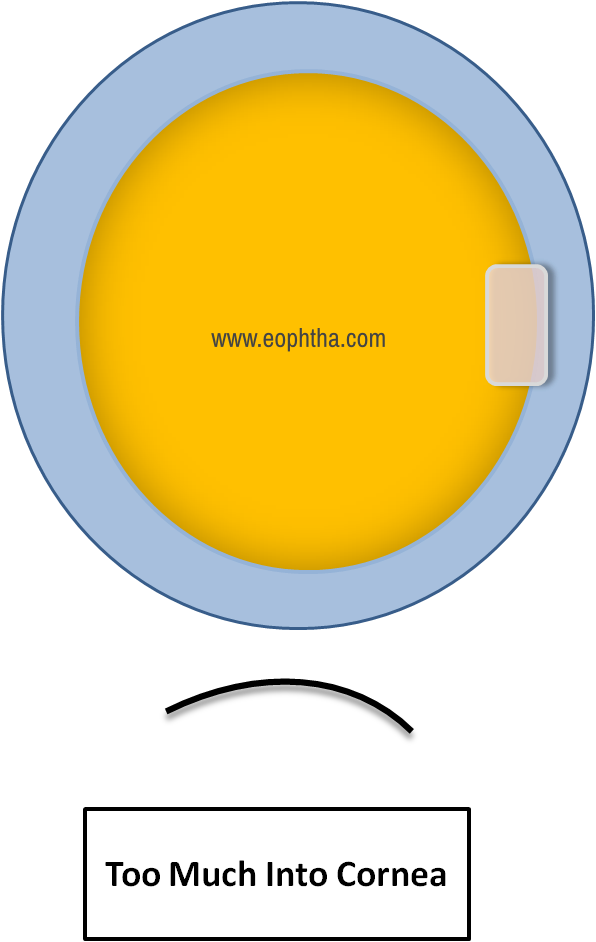
Fig 5 Sideport made too much into the cornea
So, Ideally, it should be just slightly in the cornea, to avoid iris prolapse and Descemet's membrane detachment
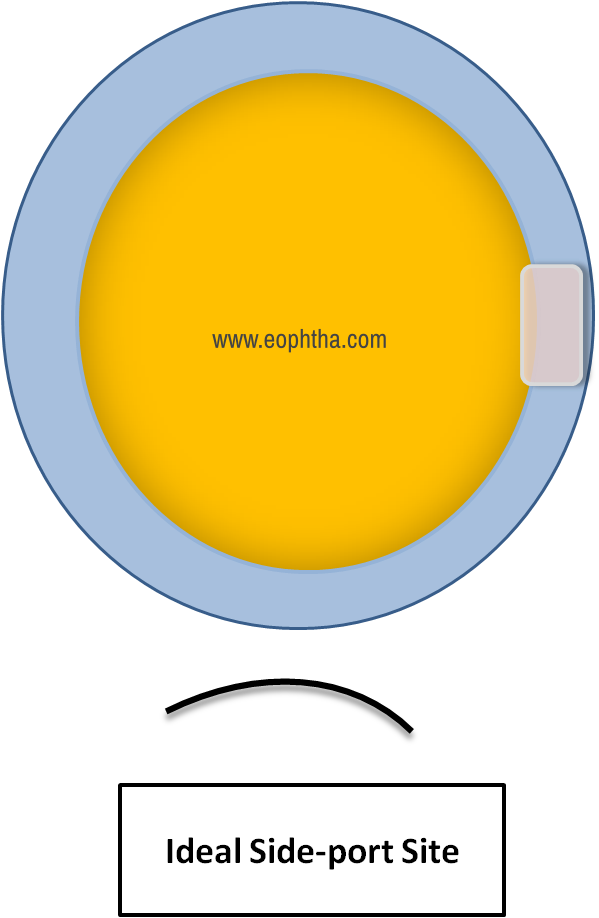
Fig 6 Ideally Placed Sideport, Slightly Corneal
3. Pterygium
Pterygium poses a lot of difficulty for side port construction and later conjunctival ballooning.
Following are a few different strategies to tackle this problem
Try to make it at a different clock hour, either superior or inferior to pterygium according to the preference.
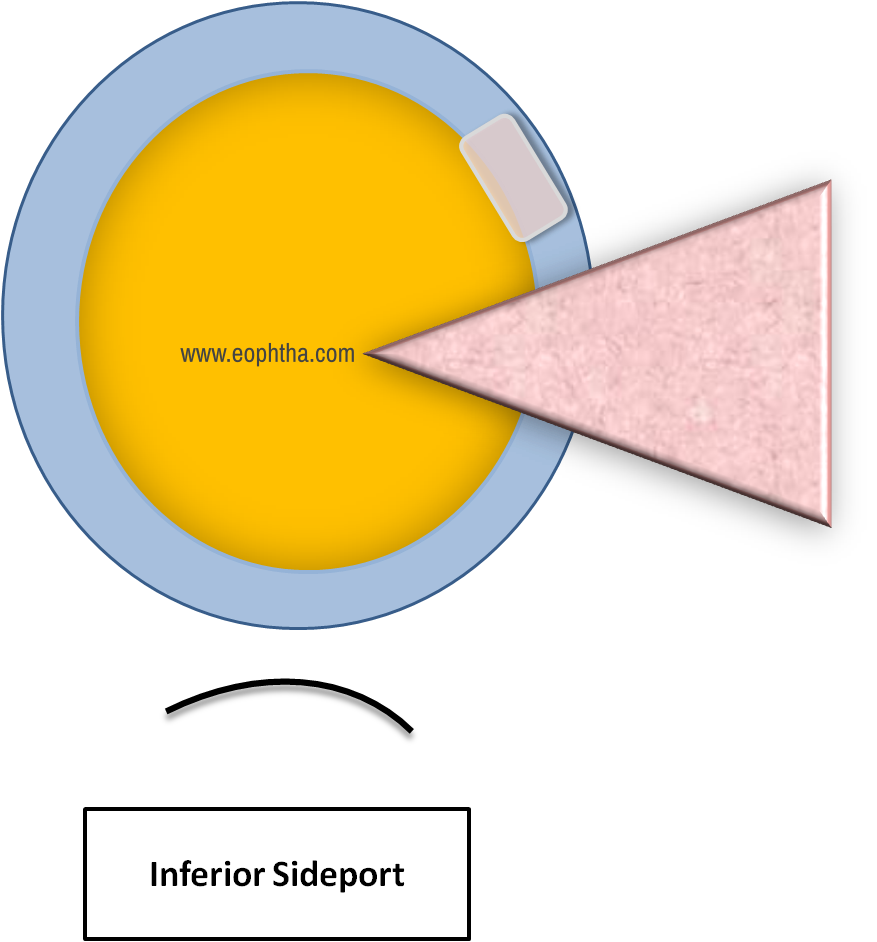
Fig 7 In Case of Pterygium, one can make a inferiorly placed sideport
One can shift the entire Tunnel and side port complex slightly Superior – Temporal to avoid the pterygium altogether
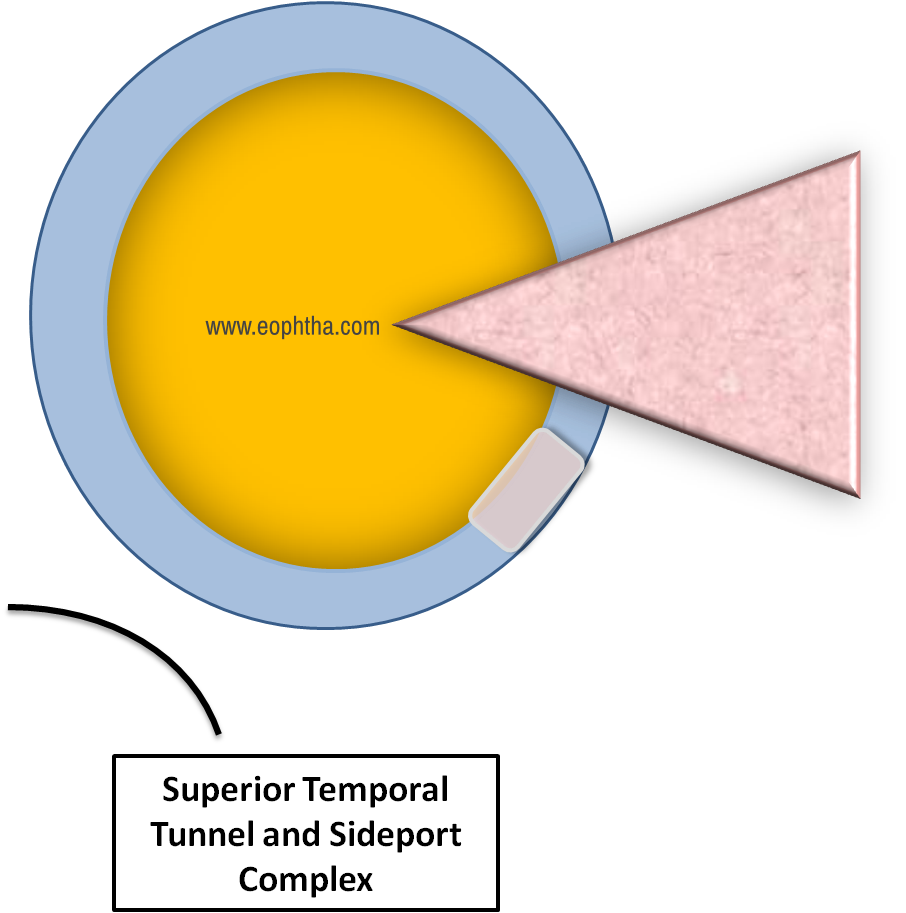
Fig 8 In the case of pterygium, one can shift side port and tunnel complex superior temporally
If you are ambidextrous then you can shift the side port to the other side.
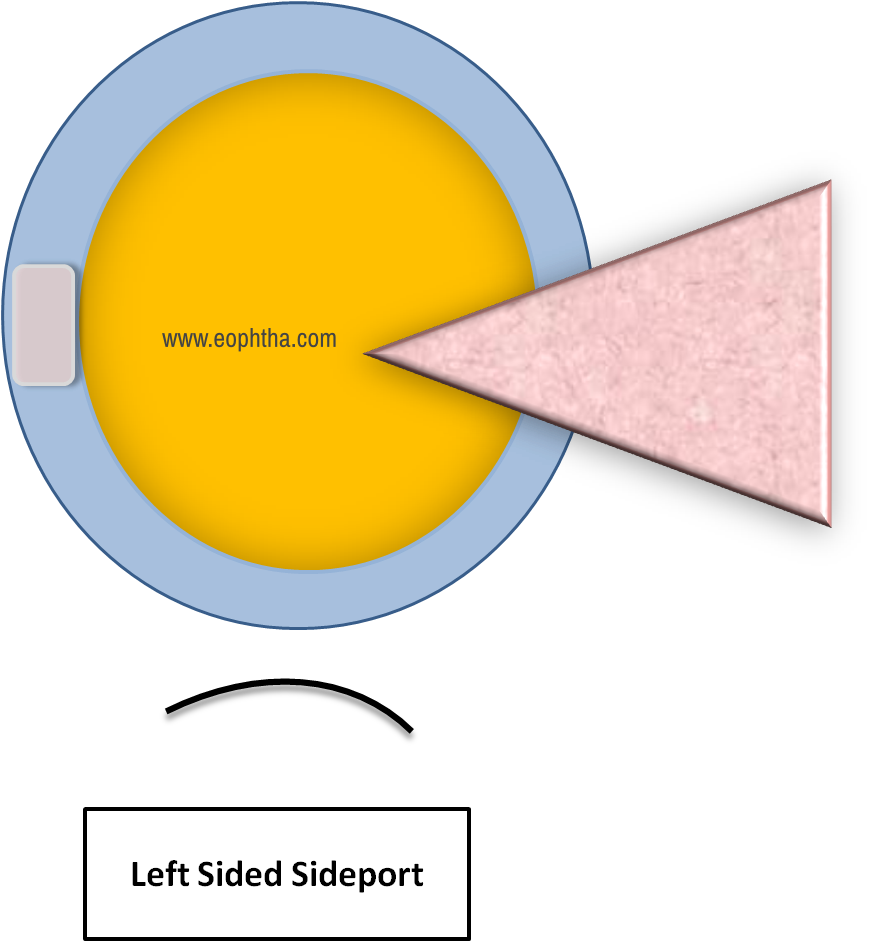
Fig 9 In case of pterygium, one can shift side port to the left side
The last option would be just to remove the pterygium if it is small and then continue as routine surgery.
4. Counter traction
While in side port construction one needs to push and move the blade on the cornea near the limbus and it needs counter traction exactly opposite to the entry point otherwise it will stop the eyeball from moving.
With improper counter, traction eyeball can rotate or twist causing changes in side port shape.
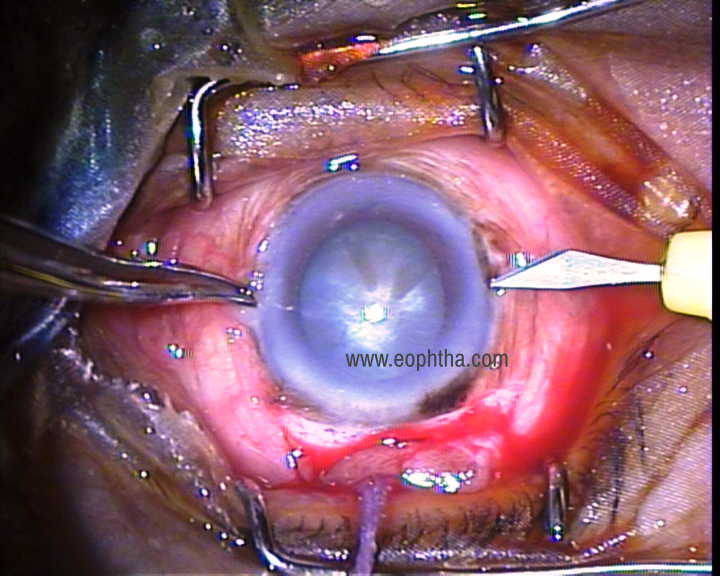
Fig 10 Correct counter traction has to be given by stabilizing the globe with forceps exactly opposite to side port
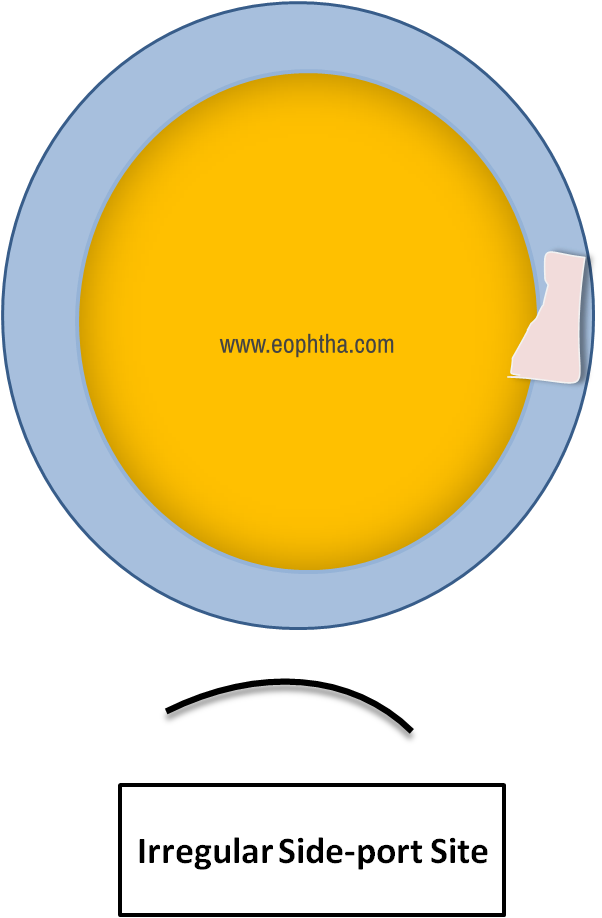
Fig 11 Improper counter traction can give rise to an irregular side port
5. Angulations
Horizontally:
As discussed earlier side port needs to be in a rectangular shape. So, while making the side port if the blade is not exactly perpendicular to the limbus, it can alter the shape of the side port and consequentially lead to difficulty in hydration at the end and increases the risk of Descemet's detachment
Vertically:
- While entering the cornea the blade should be parallel to the iris otherwise too much tilting down can injure the iris or anterior capsule
- If it is directed too much in an upward direction it can injure the cornea
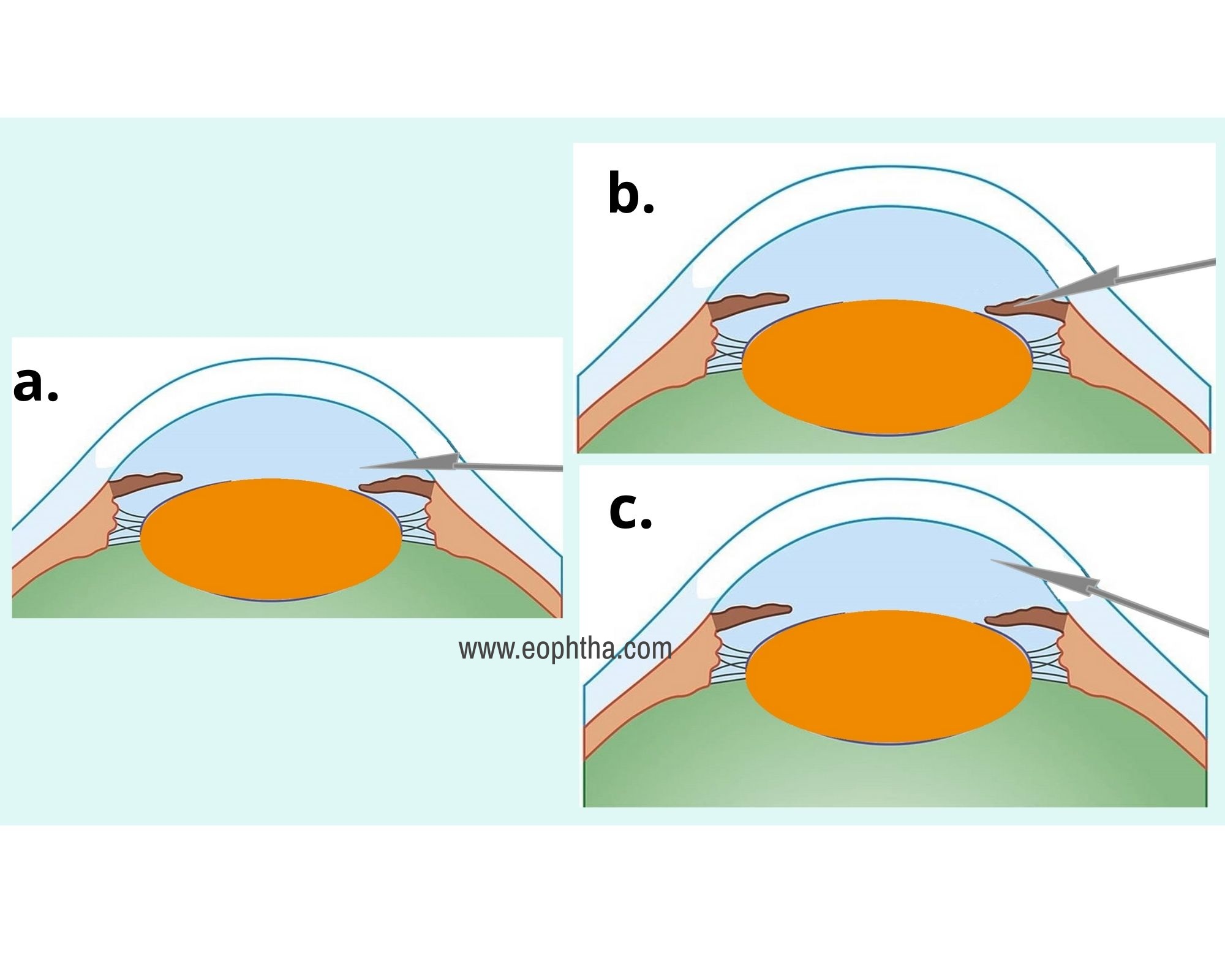
Fig 12a. Ideally, keep the blade parallel to the iris Fig 12b. Dipping the blade too much can injure the iris Fig 12c. Tilting the blade upwards can injure the cornea
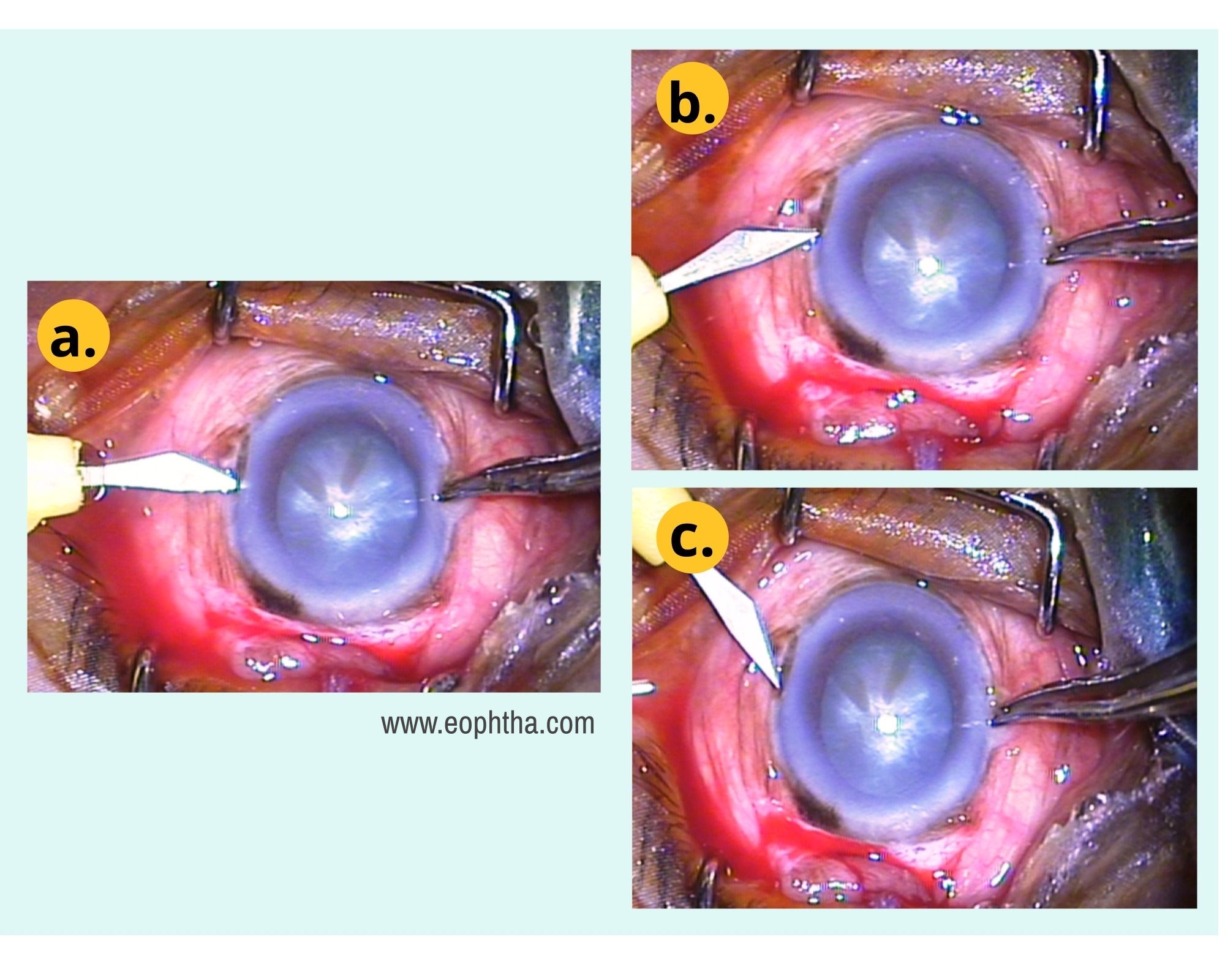
Fig 13a. Correct orientation to the globe Fig 13b.& Fig 13c.Improper orientation of the blade
6. Don’t press the globe
Any kind of excessive pressure on the globe can cause an aqueous leak and make the eyeball soft. All this changes the dynamics of the eyeball and side port constructions will go haywire. So, while doing side post construction only the forward motion of the blade without downward pressure is mandatory.
7. Quality of blade
It’s very common to have the tip of the blade bending; using this kind of blade can lead to Descemet's membrane detachment. So, always inspect the blade before using it. This tip holds good for any instrument.
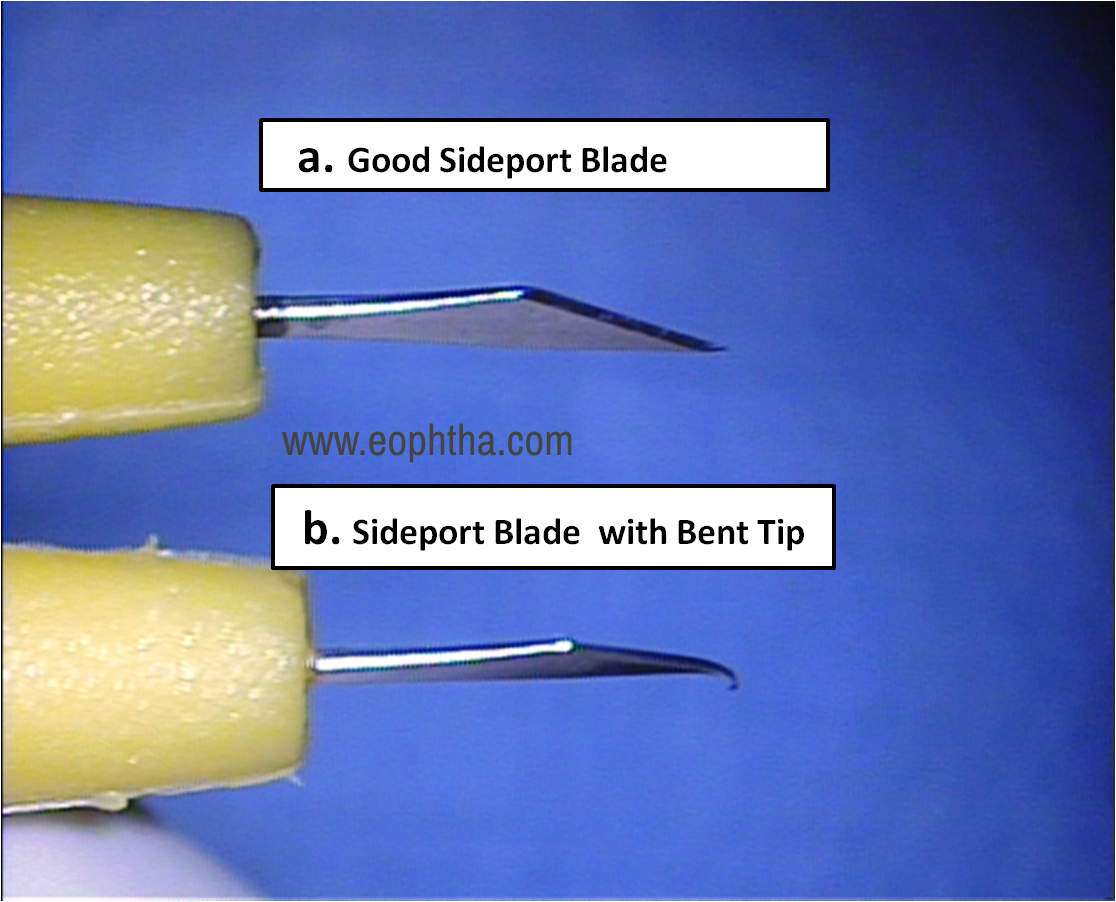
Fig 14a. Good side port blade and Fig14 b. Sideport blade with a bent tip
These tips are advisory in nature and may be taken as guiding principles. It is said practice makes man perfect but practice cannot be made in a vacuum. So consciously remember these small tips while performing a procedure and it will not be too far when you don’t need any effort for side port making becomes a seamless move. Smaller deviations depending upon one's habit of holding the blade, table position, patient position, etc. are permissible but the object must be hassle-free successful completion of the procedure.

