A 23 years old female presented to the ophthalmology clinic with complaints of blurring of vision in the left eye since the past 4-5 days with associated mild pain around the left eye, mainly on ocular movements
History of Present Illness:
Patient did not give any history of associated nausea, vomiting, headache, tingling numbness or limb weakness. There was no history of any preceding febrile illness nor any history of vaccination in the recent past.
Past Ocular History:
There was no history of any similar episode, any ocular trauma or surgery in the past.
Past Medical History:
No history of any significant systemic illness or any medications.
Family History:
No significant history.
Systemic Examination:
Within normal limits.
Pulse rate: 82/min, BP: 124/76 mmHg, Respiratory rate:12/min
OCULAR EXAMINATION:
Best Corrected Visual Acuity (BCVA)
- Right eye (OD): 6/6,N6
- Left eye (OS): 6/24,N8
Colour Vision (CV) using Ishihara pseudoisochromatic plates:
- OD: Normal 21/21
- OS: Impaired 1/21(identified only test plate)
Ocular Motility:
- Full, free but associated with mild pain in the left eye
- Orthophoria in all gazes
Intraocular Pressure:
- OU: 12mm Hg with GAT
Pupils:
- OU pupils were round, regular and equal in size, with the presence of grade 2 relative afferent pupillary defect (RAPD) in the left eye on swinging flashlight test
Confrontation visual fields:
Finger confrontation: OU-Full
Red target testing: OD -normal, OS-red desaturation centrally
Slit-lamp examination:
|
OD |
OS |
|
|
Lids/lashes |
Normal |
Normal |
|
Conjunctiva/sclera |
Normal |
Normal |
|
Cornea |
Clear |
Clear |
|
Anterior chamber |
VH 4, Quiet |
VH 4, Quiet |
|
Iris |
Normal |
Normal |
|
Lens |
Clear |
Clear |
Dilated Fundus examination:
|
OD |
OS |
|
|
Vitreous |
Clear |
Clear |
|
Disc |
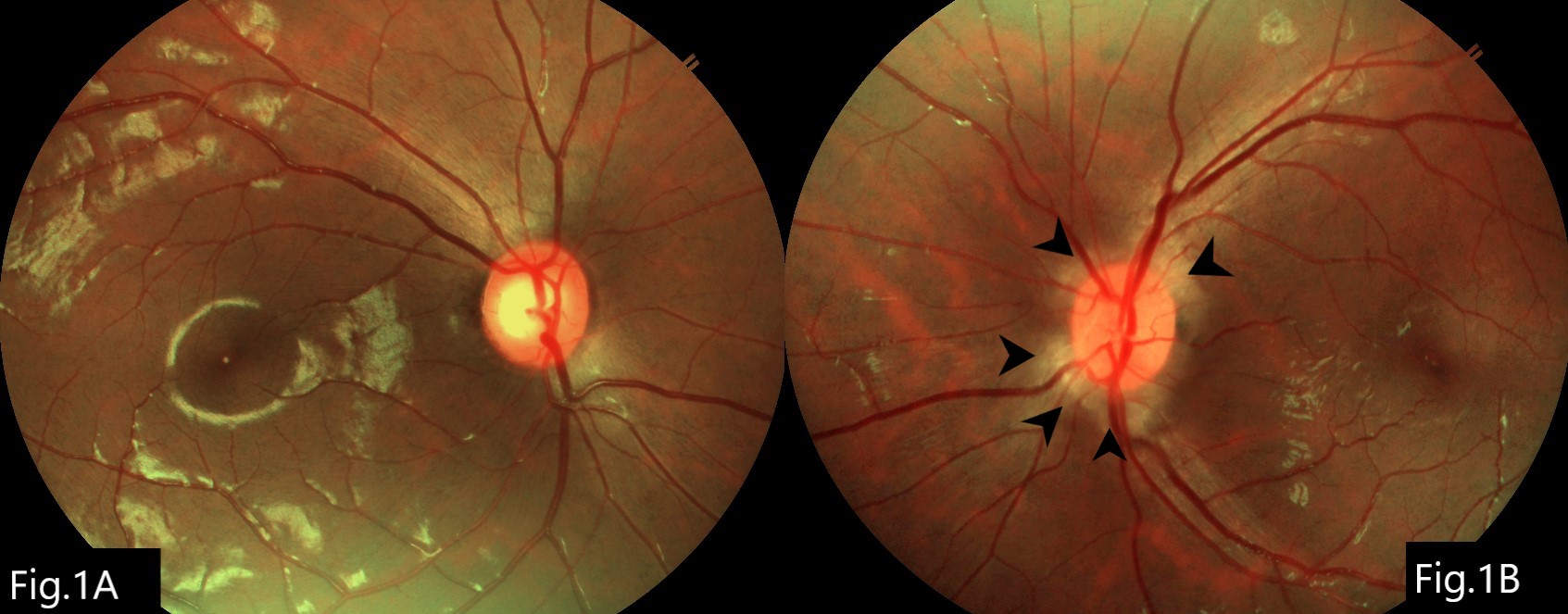
Medium sized, healthy NRR, CDR-0.4 (Fig.1A) |
Medium sized, mild oedematous, obliterated cup, elevated with peripapillary RNFL oedema (Fig.1B) |
|
Macula |
Normal |
Normal |
|
Vessels |
Normal in calibre |
Normal in calibre |
|
Periphery |
Normal |
Normal |
ANCILLARY INVESTIGATIONS:
1) Magnetic Resonance Imaging (MRI):
With the provisional diagnosis of optic neuritis, the patient was advised to get MRI of brain & orbit with gadolinium contrast. MRI orbit revealed mild thickening with post-contrast enhancement of intraconal segment of the left optic nerve on T1(Fig.2A & B), suggestive of optic neuritis(ON). Multiple areas of T2 and FLAIR hyperintensity without diffusion restriction or postcontrast enhancement were noted in bilateral periventricular white matter (Fig.2C & D) and were oriented perpendicularly (suggestive of Dawson’s fingers). Similar hyperintensities were also noted at the callososeptal interface, the juxtacortical white matter in the right frontal, and bilateral parietal lobes. Screening MRI of the whole spine showed multiple small peripheral patchy areas of T2 hyperintensities at C2 and C3 levels. These CNS lesions were suggestive of demyelinating plaques of previous attacks of Multiple Sclerosis (MS).

2) Perimetry (Humphrey’s Visual Fields) 30-2:
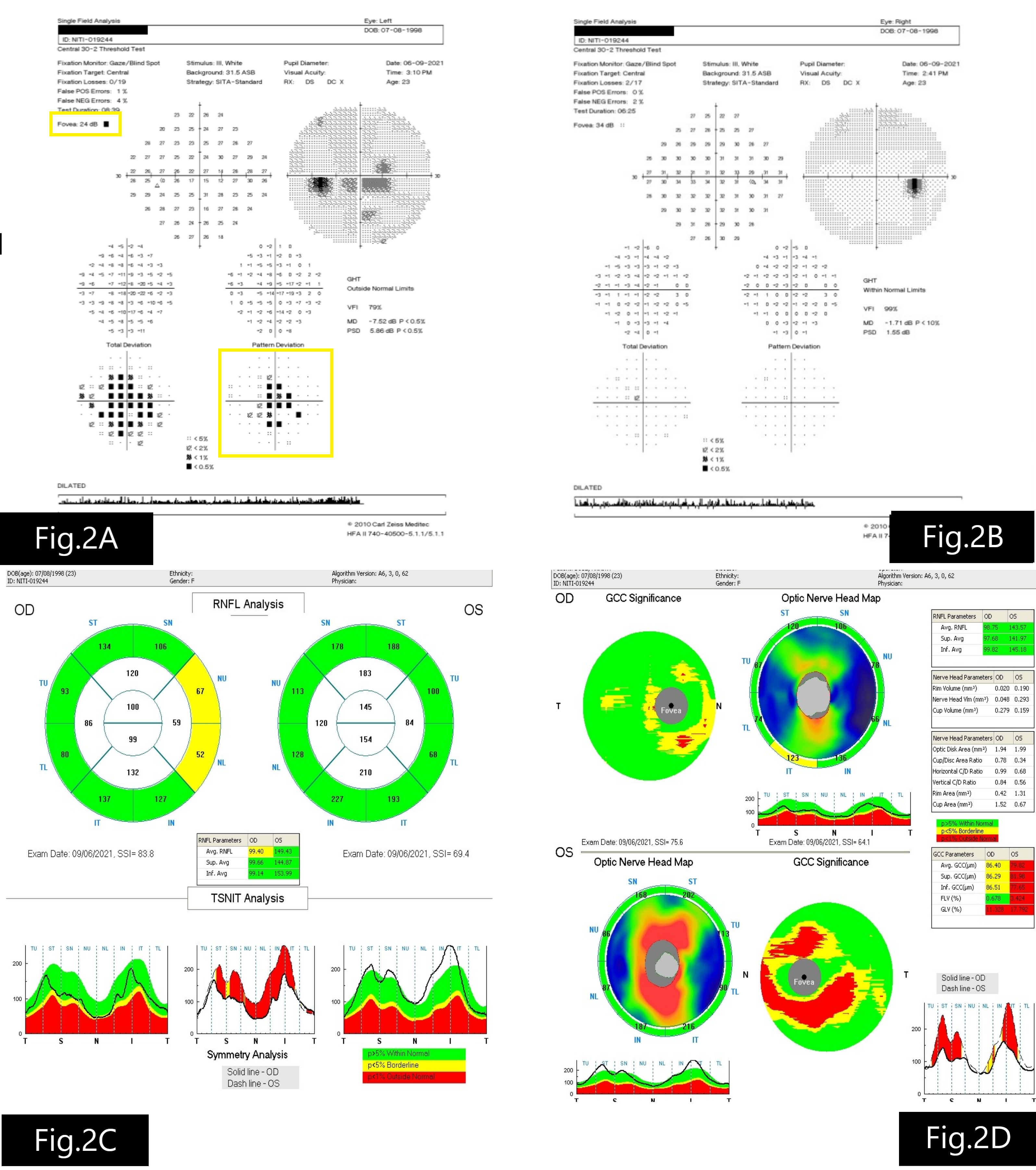
HVF 30-2 was normal in RE (Fig.3B) and LE showed decreased foveal threshold and cecocentral field defect (Fig.3A)
3) Optical Coherence Tomography (OCT):
OCT disc showed increased peripapillary retinal nerve fiber layer (pRNFL) thickness in the left eye (Fig.3C) and thinning of macular ganglion cell layer and inner plexiform layer i.e., ganglion cell complex (GCC) in the LE(Fig.3D).
Clinical Course of the condition:
Based on the clinical picture and MRI findings, the patient was diagnosed with left eye acute optic neuritis associated with MS.
She was treated with intravenous methylprednisolone (IVMP) 1 gram/day for 3 days followed by oral steroid (Prednisolone 1mg/kg/day) taper for 11 days.
After consultation with the neurologist, the patient underwent a battery of laboratory investigations including CBC, ESR, CRP, ANA, RA factor, Chest X-ray, CSF analysis-all were within normal limits. Aquaporin 4 antibody (AQP4-ab) and myelin oligodendrocyte glycoprotein (MOG) antibody were negative.
After the 3 doses of IVMP, VA improved in LE to 6/9 and CV was still defective in LE. After the course of oral steroids, vision in LE was stable, disc edema resolved and perimetry showed improvement with few central depressed points persisting.
Differential Diagnosis:
Differential Diagnosisfor disc edema associated with diminution of vision
- Typical ON
- Atypical ON (Neuromyelitis optica spectrum disorder-NMOSD,MOG,infective, autoimmune)
- Ischemic optic neuropathy
- Hereditary optic neuropathy
- Compressive optic neuropathy
- Papillitis secondary to uveitis
- Infiltrative/Neoplastic optic neuropathy
- Diabetic papillopathy
Diagnosis:
LE-Acute typical demyelinating ON associated with MS
DISCUSSION: TYPICAL OPTIC NEURITIS
Optic neuritis (ON) describes a diverse group of inflammatory and infectious optic neuropathies. Typical ON is a unilateral, acute, demyelinating, inflammatory optic neuropathy with characteristic features.
Atypical presenting features, radiographic findings, or clinical course should raise suspicion for atypical ON (Table 1). Atypical ON can result from inflammatory, infectious, autoimmune or CNS demyelinating disorder. Differentiating typical from atypical ON may be challenging early on in the clinical course, but a systematic evaluation and stepwise approach in investigations helps in arriving at the correct diagnosis.
Etiology:
Typical ON may be an isolated, idiopathic syndrome or associated with MS.Para-infectious or post-vaccination incidences have also been described in literature.
Epidemiology:
Several studies have examined the incidence of optic neuritis, and in general the range is between 1 and 6.4 new cases per year per 1 lakh population. Females are more commonly affected than males(3:2).Typical ON is seen in the age group of 20-45 years. The prevalence of ON varies to some extent based on geography and race. Whites of northern European ancestry being most susceptible, followed by whites of Mediterranean ancestry, followed by African Americans and Asians.
Pathophysiology:
The general pathology is the immune-mediated inflammatory demyelination of the optic nerve. The myelin undergoes destruction causing axons to poorly conduct impulses and the axons themselves become damaged.
After myelin destruction occurs, the retinal ganglion cell axons start to degenerate. Monocytes localize along blood vessels and macrophages follow to remove myelin. Astrocytes then proliferate with deposition of glial tissue where axons may have been present before. These gliotic (sclerotic) areas can be multiple in number throughout CNS, hence the term multiple sclerosis.
Inflammation of the central nervous system is the primary cause of damage in MS. The specific elements that start this inflammation are still unknown. Studies have suggested that genetic, environmental, and infectious agents may be among the factors influencing the development of MS.
Clinical Features:
Typical ON is mainly a clinical diagnosis. The Optic Neuritis Treatment Trial (ONTT) was a landmark randomized controlled trial that has provided the best prospective data regarding the clinical presentation, visual outcome, and risk of development of MS in patients with typical ON.
Symptoms:
- Prodromal viral illness (+/-)
- Sudden onset unilateral diminution of vision which worsens over days to stabilize around 2 weeks prior to the improvement in VA.
- Ocular pain/discomfort particularly with eye movement
- Reduced CV and field of vision
- Uhthoff phenomenon: Blurring of vision when body temperature rises during exercise or bathing in warm to hot water
- Phosphenes (flashes of lights)
- Altered perception of linear oscillating objects (Pulfrich phenomenon)
Signs:
- Decreased BCVA
- Decreased CV (red desaturation) and
- Decreased contrast sensitivity
- Visual Field Loss
- Normal looking optic disc (retrobulbar neuritis) is more common in typical ON.Optic disc may have oedema(in 35%) which is generally mild and not associated with haemorrhages or exudates
- Retinal vascular sheathing, pars planitis (periphlebitis occurs in 5-10% of MS patients)
Patients may present with atypical clinical features like bilateral vision loss, marked vision loss, absence of ocular pain, severe optic disc swelling with haemorrhages or retinal exudates or recurrent ON (Table 1). These cases should be considered for further work up to determine if an underlying inflammatory,autoimmune,infectious or CNS demyelinating disorder (NMOSD,MOG) can be found.
|
|
Typical Features |
Atypical Features |
|
Laterality |
Unilateral |
Bilateral |
|
Gender |
Female |
Male |
|
Age Group |
20-50 years |
<20 years or >50 years |
|
Pain |
Painful |
Painless or pain lasting >1-2 weeks |
|
Optic disc |
Normal optic disc(2/3rd), mild disc oedema(1/3rd) |
Severe disc oedema with haemorrhages, exudates |
|
Response to treatment |
Improvement with or without IVMP within 1 month |
OR
|
|
Vision Loss |
Colour vision loss> visual acuity loss |
Profound vision loss |
Table 1 Typical vs Atypical clinical features of ON
Ancillary Investigation:
1) MRI of Brain & Orbit with contrast:
ON is a clinical diagnosis, but MRI of the brain and orbit with contrast helps in documenting the contrast enhancement of the optic nerve and demyelinating brain lesions, thus helping in isolating the clinically isolated syndrome (CIS) from clinically definite (CD) MS.
During an acute optic neuritis attack, a fat-suppressed orbital MRI will show either T1-weighted gadolinium enhancement of the optic nerve or T2-weighted optic nerve hyperintensity. T2 /FLAIR sequences help to detect previous inflammation.
MS: A patient’s first demyelinating “attack” is called a clinically isolated syndrome (CIS). MS diagnosis requires dissemination of these attacks in both space and time with either objective clinical or radiographic evidence. Typical ON is a common CIS and approximately half of the patients with typical ON will go on to develop MS.
The main indication of MRI in ON is its prognostic value for the presence of or future development of MS.
In order to determine whether ON is a CIS or related to MS, McDonald criteria are applied. McDonald criteria revised in 2017(Table 2) outline the clinical, radiographic and laboratory evidence required to prove that demyelinating disease is disseminated in space (DIS) and disseminated in time (DIT). Essentially, a patient must have clinical evidence of at least two neurologic attacks with corresponding brain lesions to diagnose MS.
If there is only clinical evidence for one attack, then a combination of clinically silent MRI lesions in at least two of the four following areas: periventricular, cortical and juxtacortical, infratentorial, and spinal cord, is sufficient to diagnose MS. The optic nerve is not considered a typical lesion location for MS and the optic nerve lesion on MRI is not considered for DIS.
The presence of cerebrospinal fluid oligoclonal bands can also fulfill the MS diagnostic criteria if there is only clinical evidence of one attack.
|
Clinical Presentation |
Additional data needed for diagnosis of MS |
|
≥ 2 clinical attacks and objective evidence of ≥2 lesions |
None |
|
≥ 2 clinical attacks and objective evidence of 1 lesion |
DIS: an additional attack implicating a different CNS site or by MRI |
|
1 clinical attack and objective evidence of ≥2 lesions |
DIT: an additional clinical attack or by MRI OR CSF -specific oligoclonal bands |
|
1 clinical attack and objective evidence of 1 lesion |
DIS: an additional attack implicating a different CNS site or by MRI OR DIT: an additional clinical attack or by MRI OR CSF specific oligoclonal bands |
Table 2 Revised (2017) McDonald Criteria for MS diagnosis
Perimetry:
Almost every type of visual field defect pattern can be seen in ON -Generalised reduction of sensitivity/central/cecocentral scotoma/altitudinal field defect.
OCT pRNFL and GCC:
OCT is now an increasingly used tool in research on the pathogenesis, treatment, and follow-up of optic nerve disorders. In patients with acute optic neuritis pRNFL thickening is common (46%) within fifteen days of symptom onset. With the axonal loss secondary to the ON episode, pRNFL thinning may not be detected until 3 months after symptom onset, whereas GCC thinning may be seen earlier. GCC thickness is a better biomarker than pRNFL thickness early in the disease course to know the damage from the optic neuritis attack.
Visually Evoked Potential (VEP): Prolonged P100 latency on VEP is suggestive of demyelinating ON. The inter-ocular difference in latency of 8-10 ms is seen in ON. Reduced amplitudes but reproducible until small sizes is typical of ON.
Laboratory Investigation:
Extensive Serologic tests are not necessary if the presentation is of typical ON. If the features are atypical, then based on the history, clinical features and likely cause, tailored laboratory investigations are necessary (Table 3).
|
Baseline tests |
Additional tests based on possible etiology |
|
CBC |
Serum ACE, Lysozyme |
|
Blood sugar level |
VDRL, TPHA |
|
ESR, CRP |
Anti-Phospholipid antibody |
|
RA factor |
Anti-ds-DNA antibody |
|
Anti-Nuclear Antibody (ANA) |
c-ANCA, p-ANCA |
|
Chest X Ray |
HIV serology |
|
AQP4 antibody, MOG antibody |
Other infectious disease serology |
Table 3 Laboratory investigations for ON
CSF Analysis:
CSF analysis is not mandatory for the diagnosis of typical ON. But CSF examination can be considered for autoimmune and infectious etiologies with atypical presentation.
Presence of oligoclonal bands in CSF in a patient with optic neuritis with inconclusive MRI brain, may suggest higher risk of developing MS.
Treatment: Involves multidisciplinary approach involving ophthalmologist, neurologist, radiologist pathologist and sometimes immunologist.
Treatment of acute attack of typical ON is based on ONTT protocols.
ONTT outcomes:
1) IVMP treated patients recovered faster within the first 4-6 weeks post onset. However, at 6 months to 10 years out, there was no statistical difference in final visual outcome between IVMP treated patients and placebo.
2) Oral steroids in conventional doses(1mg/kg/day) alone are contraindicated for acute ON because of a higher rate of recurrences of ON.
Treatment of acute attack of ON involves
A)1gram IVMP daily for 3 days followed by an 11days oral prednisolone taper.
B) Mega dose oral prednisolone 1250 mg daily for 3 days has shown similar visual outcome in short term in the recent study but long-term follow-up of these patients is not yet available, so we do not know if there is a significant difference in recurrence rate in these patients.
Depending on the etiology (NMOSD, MOG, MS, etc.) and response to IVMP therapy of ON there may be a role for plasma exchange and IV immunoglobulin therapy after neurologist consultation. Unlike typical optic neuritis, atypical optic neuritis variants (NMOSD, MOG ON) may require early immunosuppressive therapy to minimize recurrences and long-term disability.
Patients with a high risk of developing CDMS need referral to a neurologist for early treatment with disease-modifying drugs (DMDs) like Interferon-beta 1 a(Avonex) to reduce the risk of progression to CDMS and MS. But before starting interferon therapy it is important to rule of NMO as it may worsen with interferon therapy.
An individual patient-centered approach based on the history, clinical features, and MRI findings helps in tailoring the investigations specific to the individual case of ON, treatment of the acute attack, and predicting the future course of the disease.
Summary:
TYPICAL OPTIC NEURITIS |
|
|
ETIOLOGY Autoimmune, Inflammatory, demyelinating process
|
SIGNS
|
|
SYMPTOMS
|
DIFFERENTIALS
|
|
INVESTIGATIONS
- Contrast enhancement of optic nerve on T1 -Hyperintensities on T2/FLAIR sequences in the brain and spinal cord help detect previous inflammation
|
TREATMENT ACUTE ATTACK
|
References:
1. Beck RW, Cleary PA, Anderson MM, et al. A randomized,controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med.1992;326(9):581e8
2. Beck RW, Cleary PA, Backlund JC. The course of visual recovery after optic neuritis. Experience of the optic neuritis treatment trial. Ophthalmology. 1994;101(11):1771e8
3. Chen JJ, Flanagan EP, Jitprapaikulsan J, et al. Myelin Oligodendrocyte Glycoprotein Antibody (MOG-IgG)-positive optic neuritis: Clinical characteristics, radiologic clues and outcome. Am J Ophthalmol. 2018;195:8e15
4. Filippi M, Rocca MA, Ciccarelli O, et al. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 2016;15(3):292e303
5. Filippi M, Preziosa P, Meani A, et al. Prediction of a multiple sclerosis diagnosis in patients with clinically isolated syndrome using the 2016 MAGNIMS and 2010 McDonald criteria: A retrospective study. Lancet Neurol.2018;17(2):133e42
6. Gass A, Costello FE. Optic neuritis in the diagnosis of MS:More than meets the eye. Neurology. 2018;91(12):545e6
7. Group ONS. The clinical profile of optic neuritis. Experience of the optic neuritis treatment trial. Arch Ophthalmol.1991;109(12):1673e8
8. Group ONS. Multiple sclerosis risk after optic neuritis: Final optic neuritis treatment trial follow-up. Arch Neurol.2008;65(6):727e32
9. Jitprapaikulsan J, Chen JJ, Flanagan EP, et al. Aquaporin-4 and myelin oligodendrocyte glycoprotein autoantibody status predict outcome of recurrent optic neuritis. Ophthalmology.2018;125(10):1628e37
10. Kim HJ, Paul F, Lana-Peixoto MA, et al. MRI characteristics of neuromyelitis optica spectrum disorder: An international update. Neurology. 2015;84(11):1165e73
11. Kupersmith MJ, Garvin MK, Wang JK, Durbin M, Kardon R.Retinal ganglion cell layer thinning within one month of presentation for optic neuritis. Mult Scler.2016;22(5):641e8
12. Morrow SA, Fraser JA, Day C, et al. Effect of treating acute optic neuritis with bioequivalent oral vs intravenous corticosteroids: A randomized clinical trial. JAMA Neurol.2018;75(6):690e6
13. Sellebjerg F, Nielsn HS, Fredniksen JL, Olesen J. A randomized,controlled trial of oral high-dose methylprednislone in acute optic neuritis. Neurology. 1999;52(7):1479e84
14. Shimizu J, Hatanaka Y, Hasegawa M, et al. IFNb-1b may severely exacerbate Japanese optic-spinal MS in
neuromyelitis optica spectrum. Neurology.2010;75(16):1423e7
15. Abel A, McClelland C, Lee MS. Critical review: Typical and atypical optic neuritis. Surv Ophthalmol. 2019 Nov-Dec;64(6):770-779. doi: 10.1016/j.survophthal.2019.06.001. Epub 2019 Jun 20. PMID: 31229520.
16. Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria.Lancet Neurol. 2018;17(2):162e73
17. Xu SC, Kardon RH, Leavitt JA, Flanagan EP, Pittock SJ, Chen JJ.Optical coherence tomography is highly sensitive in detecting prior optic neuritis. Neurology. 2019;92(6):e527e35
